Feeling uncertain about what to expect in your upcoming interview? We’ve got you covered! This blog highlights the most important Autoclave Maintenance and Troubleshooting interview questions and provides actionable advice to help you stand out as the ideal candidate. Let’s pave the way for your success.
Questions Asked in Autoclave Maintenance and Troubleshooting Interview
Q 1. Explain the different types of autoclaves and their applications.
Autoclaves are categorized based on their sterilization mechanism and application. The most common types are gravity displacement, prevacuum (also known as pre-vacuum or high-vacuum), and tabletop autoclaves.
- Gravity Displacement Autoclaves: These rely on gravity to remove air and introduce steam. They are simpler and less expensive but slower and less effective for sterilizing porous loads. Think of it like a tea kettle—steam pushes the air out. They are commonly found in smaller medical practices or dental offices for sterilizing smaller loads of instruments.
- Prevaccum Autoclaves: These use a vacuum pump to remove air from the chamber before introducing steam, ensuring better steam penetration and faster sterilization times. This makes them ideal for porous loads like surgical dressings and wrapped instruments, which can trap air pockets that hinder sterilization. These are more sophisticated and are a staple in hospitals and larger surgical facilities.
- Tabletop Autoclaves: These are smaller, benchtop units, often used in smaller clinics, research labs or veterinary offices for sterilizing smaller loads. They can be either gravity displacement or prevacuum types.
The choice of autoclave depends on the volume and type of materials to be sterilized, budget, and the desired level of sterility assurance.
Q 2. Describe the sterilization process in a gravity displacement autoclave.
In a gravity displacement autoclave, sterilization occurs through a process of steam displacement. The process generally follows these steps:
- Air Removal: The autoclave is loaded, the door is closed, and the chamber is heated. As steam enters, the cooler, denser air is forced out through a vent at the bottom of the chamber. This is a slow, gravity-dependent process.
- Sterilization Phase: Once the air is mostly removed and the desired temperature (typically 121°C or 134°C) and pressure (typically 15 psi or higher) are reached, the sterilization cycle begins, lasting for a predetermined time (depending on the load type and temperature selected).
- Exhaust Phase: Once the sterilization cycle is complete, the steam is slowly released from the chamber, again relying on gravity, to prevent boiling and potential damage to the instruments.
- Drying Phase (often): Some models include a drying phase where the remaining moisture is removed. This can be through continued heat or a separate drying cycle.
The effectiveness of gravity displacement depends heavily on efficient air removal. Air pockets can create ‘cool spots’ that aren’t adequately sterilized.
Q 3. How does a prevacuum autoclave differ from a gravity displacement autoclave?
The key difference lies in how air is removed from the chamber before steam introduction. Gravity displacement autoclaves rely on gravity, resulting in slower air removal and potential for incomplete sterilization. In contrast, prevacuum autoclaves use a vacuum pump to actively remove air before steam entry, leading to faster, more complete sterilization, especially for items with complex geometries or porous materials.
- Air Removal: Gravity displacement is slow and passive; prevacuum is fast and active (using a vacuum pump).
- Sterilization Time: Prevaccum generally sterilizes faster due to more efficient steam penetration.
- Sterility Assurance: Prevaccum offers higher sterility assurance, particularly for wrapped instruments and porous loads.
- Cost: Prevaccum autoclaves are usually more expensive due to the added vacuum pump system.
Imagine trying to fill a water bottle with air in it: Gravity displacement is like slowly pouring water in, hoping the air escapes – some may be trapped. Pre-vacuum is like first sucking the air out with a straw, then pouring in the water—completely filling the bottle.
Q 4. What are the parameters (temperature, pressure, time) for sterilizing different types of instruments?
Sterilization parameters vary depending on the type of instrument and its packaging. The recommended parameters are often provided by the instrument manufacturer. However, general guidelines exist:
- 121°C (250°F) for 15-20 minutes: This is common for unwrapped instruments and some liquids, utilizing saturated steam under pressure. This is often the standard cycle in gravity displacement and prevacuum autoclaves.
- 134°C (273°F) for 3-5 minutes: This higher temperature, shorter cycle is used with prevacuum autoclaves for unwrapped instruments, reducing the cycle time. Note, some materials may be damaged by this higher temperature.
- Porous Goods (e.g., dressings): Require longer exposure times to ensure complete sterilization and are often best processed in prevacuum autoclaves.
- Wrapped Instruments: Generally require longer sterilization times to account for the additional barrier and potential for air entrapment. Usually 121°C for 20-30 min or 134°C for 10-15 min in prevacuum.
It is crucial to consult manufacturers’ instructions for specific instruments to prevent damage or inadequate sterilization. Always use appropriately validated cycles.
Q 5. What are the common causes of autoclave malfunctions?
Autoclave malfunctions can stem from various issues:
- Air Leaks: Leaks in the door seals, chamber gaskets, or tubing can prevent the achievement of adequate pressure and temperature.
- Faulty Sensors or Controls: Incorrect temperature or pressure readings from malfunctioning sensors can lead to inadequate sterilization.
- Blocked Drains or Vents: Accumulated debris can obstruct proper steam flow or air removal.
- Heating Element Issues: A faulty heating element may be unable to reach and maintain the required temperature.
- Vacuum Pump Problems (Prevaccum): Problems with the vacuum pump can result in inefficient air removal.
- Insufficient Water Supply: Lack of water can disrupt the steam generation process.
- Overloading the Chamber: Excessive loading can prevent adequate steam penetration to all items.
Regular maintenance and preventative measures are key to minimizing malfunctions.
Q 6. How do you troubleshoot a malfunctioning autoclave?
Troubleshooting a malfunctioning autoclave involves a systematic approach.
- Check the obvious: Begin by assessing the simplest issues: Is there sufficient water? Are the drains and vents clear? Is the autoclave overloaded?
- Check Sensor Readings: Verify that temperature and pressure gauges are providing accurate readings. Compare against the expected values for each phase of the cycle.
- Inspect for Leaks: Carefully check all seals, gaskets, and connections for leaks by visually inspecting for visible steam leakage or pressure drop during a cycle.
- Test the Vacuum Pump (if applicable): Check the vacuum pump’s operation, ensuring it achieves the proper vacuum level.
- Review Log Data: Review the autoclave’s service logs for any error codes or recorded malfunctions.
- Contact Service Personnel: If the problem persists after initial checks, it’s best to contact qualified service personnel to diagnose and repair the fault. Improper repair can be dangerous.
Remember, safety is paramount. Never attempt repairs beyond your expertise. Always consult the manufacturer’s manual for specific troubleshooting steps for your autoclave model.
Q 7. Explain the importance of autoclave validation and how it’s performed.
Autoclave validation is crucial to ensure that the equipment consistently delivers effective sterilization. It verifies that the autoclave is operating according to its specifications and is capable of achieving the required level of sterility. Validation involves a series of tests to confirm various aspects of the sterilization process.
- Physical testing: This assesses the parameters of the autoclave such as temperature, pressure, and vacuum levels to confirm that it reaches and maintains the desired settings throughout each cycle.
- Biological indicators (BIs): BIs contain living spores that are resistant to sterilization. Placement of the BIs within the autoclave during a cycle allows for verification that sterilization is indeed taking place throughout the chamber.
- Chemical indicators: These indicators change color when exposed to appropriate temperature and steam; they serve as a visual confirmation that the correct conditions were achieved. External chemical indicators are placed on the packages to confirm exposure to sterilization conditions. Internal indicators are placed inside the packages themselves to confirm penetration of sterilization conditions.
Validation is performed using specific protocols and should be conducted at installation, after repairs, and at regular intervals to maintain confidence in the autoclave’s performance.
A well-documented validation program is essential for compliance with regulatory requirements, patient safety, and quality assurance. Results of validation runs are carefully documented and help to establish traceability of the sterilization process.
Q 8. Describe the different types of autoclave cycles.
Autoclaves utilize various cycles tailored to different sterilization needs. The cycle type depends on the materials being sterilized and the desired level of sterility. Common types include:
- Gravity Displacement Cycle: This is a classic method relying on steam’s inherent displacement of air. It’s simple but slower and may leave air pockets in porous loads, leading to incomplete sterilization. Think of it like filling a glass with water – the water (steam) pushes the air (from the load) out from the top.
- Pre-vacuum Cycle: This cycle uses a vacuum pump to remove air from the chamber before steam injection. This ensures more efficient steam penetration and quicker sterilization, particularly for wrapped instruments or porous materials. Imagine using a straw to quickly suck air out of the glass before filling it with water; the water fills the glass more efficiently.
- Flash Sterilization Cycle: Used for unwrapped instruments that need quick sterilization. It’s fast but offers a lower sterility assurance level, primarily suitable for items that will be used immediately. This is like quickly rinsing a glass instead of thoroughly washing it.
- Liquid Sterilization Cycle: Specifically designed for liquids, this cycle requires careful control of temperature and pressure to avoid boiling over or damaging the contents. Think of gently heating a delicate sauce on the stove – you need precise temperature control.
The choice of cycle is critical for effective sterilization. Improper cycle selection can compromise the sterility of instruments and materials.
Q 9. How do you interpret autoclave printouts and logs?
Autoclave printouts and logs are crucial for documenting sterilization cycles and ensuring proper functioning. They typically include:
- Date and Time: Records when the cycle ran.
- Cycle Type: Specifies the sterilization cycle used (gravity, pre-vacuum, etc.).
- Chamber Temperature and Pressure: Charts the temperature and pressure throughout the cycle, showing that the required parameters were reached and maintained.
- Duration: Indicates the total cycle time.
- Sterility Assurance Level (SAL): States the probability of a single viable microorganism surviving the cycle (e.g., 10-6 means one in a million chance of survival).
- Error Messages (if any): Highlights any malfunctions or deviations from the expected cycle profile.
Analyzing these parameters allows you to verify the efficacy of each sterilization cycle. Deviations from the expected values may indicate a problem that needs attention. For example, if the temperature doesn’t reach the required level, it suggests a possible malfunction in the heating element or a faulty temperature sensor.
Regular review of logs is essential for preventative maintenance and troubleshooting. Trends in cycle parameters can identify potential problems before they become serious.
Q 10. What safety precautions must be followed when operating and maintaining an autoclave?
Autoclave operation and maintenance require strict adherence to safety protocols to prevent injury and contamination. Key precautions include:
- Proper Training: Only trained personnel should operate and maintain the autoclave.
- Personal Protective Equipment (PPE): Always wear appropriate PPE, including gloves, eye protection, and a lab coat when handling materials or performing maintenance.
- Load Preparation: Items must be properly wrapped or contained to prevent contamination and ensure steam penetration. Overloading the chamber can compromise sterilization.
- Pressure Relief: Never open the door until the pressure has completely dropped to atmospheric pressure. The sudden release of high-pressure steam can cause serious burns.
- Regular Inspection: Conduct regular visual inspections for leaks, damage to seals, and proper functioning of safety mechanisms.
- Maintenance Logs: Keep accurate records of maintenance performed, including dates, types of service, and any issues encountered.
- Waste Disposal: Dispose of contaminated materials according to established protocols.
Ignoring these precautions can result in serious accidents, including burns, infections, and equipment damage. Regular training and adherence to safety protocols are paramount.
Q 11. What are the common types of autoclave chamber failures?
Autoclave chamber failures can stem from various sources, impacting sterilization efficacy and safety. Common issues include:
- Leaks: Leaks in the chamber door seals or body can lead to pressure loss, preventing adequate steam generation and sterilization. This is similar to a leaky faucet – the pressure is lost before it can perform its intended task.
- Faulty Heating Elements: A malfunctioning heating element will fail to reach the required temperature for sterilization, rendering the cycle ineffective. This is akin to a broken stove burner that cannot heat food properly.
- Malfunctioning Vacuum Pump (in pre-vacuum cycles): If the vacuum pump fails, proper air removal is impossible, leading to incomplete sterilization. This is like trying to drink from a straw with a hole in it.
- Temperature Sensor Errors: Inaccurate temperature readings can result in incorrect sterilization cycles, either too short or too long. A faulty thermometer would lead to inaccurate cooking times.
Early detection of these failures is crucial to prevent compromised sterilization and potential accidents. Regular maintenance and inspections are critical to identify and address these issues before they become significant problems.
Q 12. How do you perform a Bowie-Dick test and what does it assess?
The Bowie-Dick test is a daily, pre-sterilization test that specifically assesses the air removal capacity of a pre-vacuum autoclave. It uses a special test pack containing a chemical indicator that changes color upon proper steam penetration.
Procedure:
- Place the Bowie-Dick test pack in the autoclave chamber. It should be placed centrally and not stacked with other materials.
- Run a short pre-vacuum sterilization cycle (typically 3.5 to 4 minutes at 132-134°C).
- After the cycle, carefully remove the test pack and visually inspect the chemical indicator. Uniform color change across the entire pack indicates proper air removal. Uneven coloration suggests inadequate air removal and potential sterilization problems.
Assessment: The test verifies that the autoclave’s vacuum system effectively removes air from the chamber, crucial for successful sterilization. A failed test indicates a potential problem with the vacuum pump, air leaks, or other components affecting air removal. It does not test the complete sterilization process but rather a critical step within it.
Regular Bowie-Dick testing helps ensure that the pre-vacuum sterilization cycles are functioning as expected and will identify potential issues before they affect patient care or research validity.
Q 13. What is the purpose of a biological indicator in autoclave sterilization?
Biological indicators (BIs) are crucial for confirming the lethality of a sterilization cycle. Unlike chemical indicators that only show if a parameter (e.g., temperature, pressure) was achieved, BIs provide definitive proof that the cycle killed resistant microorganisms.
A BI typically contains a known number of highly resistant bacterial spores (e.g., Geobacillus stearothermophilus for steam sterilization). These spores are inoculated onto a carrier and placed within the sterilization load. After the cycle, the BI is incubated. If sterilization was successful, no growth will be observed. If growth is detected, the sterilization cycle failed.
The use of BIs adds an extra layer of assurance beyond the physical parameters recorded by the autoclave. This is essential for ensuring sterility, especially for critical medical devices and materials.
Q 14. How do you interpret the results of a biological indicator test?
Interpreting BI results is straightforward: Absence of growth signifies successful sterilization, while the presence of growth indicates that the sterilization cycle failed. Here’s a breakdown:
- Negative Result (No Growth): The BI shows no bacterial growth after incubation. This confirms that the sterilization process was effective in killing the highly resistant spores. This is the desired outcome.
- Positive Result (Growth): The BI shows bacterial growth after incubation. This unequivocally demonstrates that the sterilization process failed to kill the spores. Immediate investigation is needed to determine the cause of failure (e.g., malfunctioning equipment, improper loading, inadequate cycle parameters).
Detailed record-keeping of BI results is essential for quality assurance. Positive results necessitate immediate corrective actions and a thorough review of the sterilization process and equipment.
Remember, a negative result from a BI only guarantees the sterility of that specific load; ongoing monitoring through routine BI testing remains crucial for consistently reliable sterilization.
Q 15. Explain the importance of regular autoclave maintenance.
Regular autoclave maintenance is paramount for ensuring sterilization efficacy, protecting personnel safety, and extending the lifespan of this crucial piece of equipment. Think of it like regular car maintenance – neglecting it leads to breakdowns, costly repairs, and potentially dangerous situations. Consistent maintenance prevents malfunctions that can compromise sterilization cycles, leading to potentially serious health risks in healthcare or research settings.
- Improved Sterilization Effectiveness: Regular checks and cleaning ensure the autoclave consistently achieves the required temperature and pressure for effective sterilization.
- Reduced Downtime: Preventative maintenance minimizes unexpected breakdowns, reducing costly downtime and lost productivity.
- Enhanced Safety: Routine inspections identify and rectify potential safety hazards, like faulty seals or electrical issues, preventing accidents.
- Extended Equipment Lifespan: Proper maintenance significantly extends the operational life of the autoclave, delaying the need for expensive replacements.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Describe the steps involved in cleaning and maintaining an autoclave chamber.
Cleaning and maintaining the autoclave chamber is a crucial step in ensuring its proper functioning and preventing contamination. Always follow the manufacturer’s instructions, but generally, the process involves these steps:
- Power Down and Cool Down: Ensure the autoclave is completely powered off and cooled down before commencing any cleaning.
- Remove Debris: Carefully remove any debris, instruments, or waste from the chamber using appropriate tongs or gloves. Avoid touching hot surfaces.
- Wipe Down Interior: Use a non-abrasive cleaner designed for autoclaves to thoroughly wipe down the chamber walls, shelves, and door seals. Pay attention to corners and crevices.
- Rinse Thoroughly: Rinse the chamber thoroughly with clean, distilled water to remove any residual cleaner.
- Dry Completely: Allow the chamber to air dry completely before running a test cycle. Leaving moisture inside can promote corrosion and bacterial growth.
- Run a Sterilization Cycle: After cleaning, run a short sterilization cycle with distilled water only to further sanitize the chamber.
For example, using a mixture of distilled water and a commercially available autoclave cleaner according to the manufacturer’s dilution instructions is a common and effective practice. Always consult your autoclave’s manual for specific cleaning procedures and recommended cleaning agents.
Q 17. What are the common problems associated with autoclave door seals?
Autoclave door seals are critical for maintaining pressure and ensuring proper sterilization. Problems with these seals can compromise the entire sterilization process and pose safety risks. Common issues include:
- Leaks: Small cracks, tears, or deterioration in the seal can lead to pressure leaks, resulting in inconsistent sterilization.
- Compression Issues: The seal may not compress properly, leading to insufficient sealing and pressure loss. This could be due to seal wear, damage, or misalignment of the door.
- Contamination: A damaged or improperly cleaned seal can harbour bacteria, which can contaminate subsequent sterilization cycles.
- Hardening or Brittleness: Over time, the seal material can become brittle and less effective, increasing the likelihood of leaks.
Think of the seal as a critical gasket in your car engine – a leak there compromises performance and could even lead to catastrophic failure. The same applies to an autoclave.
Q 18. How do you troubleshoot a faulty autoclave door seal?
Troubleshooting a faulty autoclave door seal begins with a visual inspection. Look for any obvious signs of damage, such as cracks, tears, or significant wear. If visual inspection reveals a problem, replacement is usually necessary.
- Visual Inspection: Examine the seal for any visible damage, cracks, or signs of wear and tear.
- Pressure Test: Conduct a pressure test (following manufacturer guidelines) to identify leaks. This often involves running a sterilization cycle and monitoring the pressure gauge for drops indicating leakage.
- Seal Compression Check: Check if the door seal is compressing evenly when the door is closed. Uneven compression may indicate misalignment or damage to the door mechanism.
- Replacement: If the seal is damaged beyond repair, replace it with a genuine OEM (Original Equipment Manufacturer) replacement seal. Using a non-OEM seal could compromise safety and performance.
If a pressure test reveals a leak, and visual inspection doesn’t immediately show a problem, a qualified technician should investigate further to identify the exact source of the leak. Attempting complex repairs without proper training is dangerous and could lead to further damage or injury.
Q 19. How do you maintain the autoclave’s water supply system?
Maintaining the autoclave’s water supply system is crucial for its proper operation and prevents mineral buildup that can impact heating elements and cause corrosion. This usually includes:
- Water Quality: Use only distilled or deionized water in the autoclave to prevent mineral deposits and scale buildup. Tap water contains minerals that can damage internal components over time.
- Regular Flushing: Regularly flush the water reservoir and lines according to the manufacturer’s recommendations to remove any sediment or mineral deposits.
- Filter Maintenance: If the autoclave has a water filter, replace or clean it at the recommended intervals to ensure clean water supply. A clogged filter can reduce efficiency and performance.
- Inspection: Visually inspect water lines and connections for leaks or damage. Address any issues immediately to prevent water damage and operational problems.
Imagine the water system as the circulatory system of the autoclave. If it’s clogged or contaminated, the whole system suffers. Regular maintenance is key for longevity.
Q 20. What are the regulatory requirements for autoclave operation and maintenance?
Regulatory requirements for autoclave operation and maintenance vary depending on location and the specific industry. However, common regulations often emphasize:
- Validation and Qualification: Regular validation of sterilization cycles and qualification of the equipment is essential to demonstrate consistent sterilization performance. This often involves biological indicators.
- Documentation: Meticulous record-keeping of maintenance activities, sterilization cycles, and any malfunctions is crucial for compliance audits. This includes documenting the use of biological indicators.
- Operator Training: Operators must be adequately trained on the safe and proper operation and maintenance procedures of the autoclave. This is vital for preventing accidents and ensuring the effectiveness of sterilization.
- Safety Standards: Adherence to relevant safety regulations and guidelines regarding pressure vessels, electrical safety, and the handling of potentially hazardous materials is mandatory.
These regulations are designed to ensure patient safety and prevent cross-contamination, emphasizing the importance of stringent operational protocols. Non-compliance can lead to severe penalties.
Q 21. How do you handle a malfunctioning autoclave during an emergency?
Handling a malfunctioning autoclave during an emergency requires a calm and systematic approach, prioritizing safety. The specific steps may vary depending on the type of malfunction, but the general principles include:
- Power Down: Immediately power down the autoclave if safe to do so.
- Isolate: Isolate the autoclave to prevent access by unauthorized personnel.
- Evacuate: If necessary, evacuate the area, following established emergency protocols.
- Contact Support: Contact qualified service technicians or the manufacturer for immediate assistance. Do not attempt repairs without proper training.
- Document: Document the malfunction, including the time, date, and any observed issues. This information is crucial for troubleshooting and future preventative measures.
Safety is paramount. Never attempt to force the autoclave open or operate it if it’s malfunctioning. Improper handling can lead to serious injuries or equipment damage. Professional assistance is always the safest option.
Q 22. Explain the importance of proper documentation in autoclave maintenance.
Proper documentation in autoclave maintenance is paramount for ensuring safe and effective operation, regulatory compliance, and traceability. Think of it as the autoclave’s medical record – it tracks its health and performance over time. Without it, you’re flying blind.
Preventive Maintenance Logs: These meticulously record scheduled maintenance activities, like cleaning, filter changes, and component inspections. This allows us to predict potential failures and avoid costly downtime.
Repair and Service Records: Detailed notes on any repairs, replacements, or service calls, including the nature of the problem, parts used, and technician signatures. This aids in identifying recurring issues and patterns.
Sterilization Cycle Records: Each sterilization cycle should be logged, including date, time, parameters (temperature, pressure, duration), and the load details. This ensures the efficacy of sterilization and provides evidence for regulatory compliance.
Calibration Records: Regular calibration of temperature and pressure gauges is crucial for accurate sterilization. These records demonstrate the accuracy of the readings and ensure the autoclave is operating within acceptable parameters.
In a nutshell, comprehensive documentation protects both the equipment and the users. It’s vital for auditing purposes and helps establish a proactive maintenance strategy.
Q 23. How do you identify and address potential hazards related to autoclave operation?
Autoclave operation presents several potential hazards, primarily related to high-pressure steam, high temperatures, and the potential for exposure to infectious agents. Identifying and mitigating these hazards requires a multi-faceted approach.
High-Pressure Steam Burns: This is the most significant risk. Proper training on safe operating procedures, including the use of appropriate personal protective equipment (PPE) like heat-resistant gloves and eye protection, is crucial. Regular inspection of safety valves and pressure gauges is also vital.
Infectious Agent Exposure: Always treat all materials processed as potentially infectious. Adhering to strict sterilization protocols and proper waste disposal practices minimizes the risk of exposure. Following established decontamination procedures before handling materials is essential.
Equipment Malfunction: Regular maintenance, including leak checks and component inspections, significantly reduces the risk of malfunction. Proper training on emergency shut-off procedures is vital in case of an unexpected event.
Improper Waste Disposal: Failure to properly dispose of contaminated waste can lead to environmental contamination and the spread of infectious agents. Following the established procedures and using appropriate biohazard containers is non-negotiable.
Think of safety as a layered defense: proper training, regular inspections, maintenance protocols, and adherence to safety standards form the layers that minimize risks significantly. This proactive approach is not just a checklist; it is a life-saving measure.
Q 24. What are the different types of autoclave pumps and their maintenance requirements?
Autoclaves utilize different types of pumps depending on their design and application. The most common are vacuum pumps and peristaltic pumps.
Vacuum Pumps: These pumps remove air from the autoclave chamber before steam injection, ensuring efficient and uniform sterilization. They require regular maintenance, including oil changes (for oil-sealed pumps), filter replacements, and leak checks. Ignoring this maintenance can lead to reduced vacuum performance and potential equipment damage.
Peristaltic Pumps: These are often used for liquid delivery systems in autoclaves, such as those employing a gravity feed system. Their maintenance involves regular inspection of the pump tubing for wear and tear, promptly replacing worn or damaged tubing to prevent leaks and ensure accurate fluid delivery. Lubrication, if required, must be done according to manufacturer’s instructions.
The specific maintenance requirements will depend on the manufacturer and the pump’s model. Always consult the manufacturer’s service manual for detailed instructions and recommended maintenance schedules. Proactive maintenance will save you considerable time and money in the long run by preventing unexpected breakdowns and ensuring reliable operation.
Q 25. How do you ensure the proper disposal of contaminated waste from an autoclave?
Proper disposal of contaminated waste from an autoclave is critical for maintaining a safe and compliant environment. This is not simply about putting waste in a bin; it’s about following a rigorous process that protects both personnel and the environment.
Biohazard Containers: All waste from the autoclave should be placed in appropriately labeled and sealed biohazard containers. These containers must be puncture-resistant and leak-proof.
Decontamination Procedures: Before removal from the autoclave, ensure items have completed the sterilization cycle. For particularly hazardous materials, additional decontamination steps may be necessary following the sterilization cycle (e.g., chemical disinfection).
Waste Stream Management: Properly follow the waste stream protocols of your facility and local regulations. This will vary depending on the type of waste (e.g., sharps, liquid waste, solid waste). This often involves autoclaving the waste to decontaminate it before disposal via incineration or other approved methods.
Documentation: Every disposal procedure should be carefully documented, including the date, time, type of waste, and method of disposal. This provides a clear audit trail and helps ensure compliance with regulations.
Ignoring these protocols can lead to serious health risks and environmental damage, as well as regulatory penalties. Consider the potential consequences – it’s a significant responsibility.
Q 26. What are the key components of an autoclave and their function?
An autoclave is a complex piece of equipment, and understanding its key components is essential for effective operation and maintenance. Let’s break down the key players:
Chamber: This is the heart of the autoclave, where the sterilization process occurs. It’s designed to withstand high pressure and temperature.
Door: The airtight door secures the chamber and prevents steam leakage during operation. Regular inspection and lubrication of seals are crucial to maintain this airtight seal.
Heating Element: This generates the heat necessary to produce steam for sterilization. Regular inspection and maintenance are vital to ensure efficient heating and prevent failure.
Pressure Gauge: This indicates the pressure inside the chamber. Regular calibration is critical for accurate and safe operation.
Temperature Gauge: This monitors the chamber temperature. Just like the pressure gauge, regular calibration is critical for accuracy and effective sterilization.
Control System: This regulates the temperature, pressure, and duration of the sterilization cycle. Proper functioning of the control system is vital for reliable sterilization and safety.
Safety Valves: These are critical safety features designed to release excess pressure to prevent explosions in case of malfunction. Regular inspection and testing are critical.
Vacuum Pump (for some models): This removes air from the chamber before steam injection, ensuring efficient and uniform sterilization.
Each component plays a vital role, and their proper function is essential for safe and effective sterilization. Neglecting even one can jeopardize the entire process.
Q 27. Explain the concept of steam sterilization and its limitations.
Steam sterilization is a widely used method for decontaminating and sterilizing medical instruments and other materials. It relies on the lethal effects of saturated steam under pressure to eliminate microorganisms.
The Process: Saturated steam, under pressure, achieves higher temperatures than boiling water at atmospheric pressure. This elevated temperature denatures proteins and disrupts the cellular structure of microorganisms, rendering them inactive. The combination of heat and moisture is particularly effective at killing both vegetative bacteria and their spores.
Limitations: While highly effective, steam sterilization has limitations:
Material Compatibility: Some materials, such as certain plastics and heat-sensitive electronics, cannot withstand the high temperatures and pressures used in steam sterilization. This necessitates the use of alternative sterilization methods for these materials.
Penetration Limitations: Steam penetration can be hindered by dense materials or porous structures. Ensuring adequate steam penetration requires proper loading techniques and the use of appropriate packaging materials.
Residue Concerns: Depending on the material, certain materials may interact negatively with steam, possibly producing residues. Careful selection of packaging can help mitigate this issue.
Size and Shape Limitations: The design and size of the autoclave can restrict the size and shape of objects that can be effectively sterilized.
Understanding these limitations helps select the most appropriate sterilization method for the materials being processed. In practice, you often have to balance the effectiveness of steam sterilization with the sensitivity of the materials to heat and moisture.
Q 28. Describe your experience with different types of autoclave manufacturers and their service protocols.
Over my career, I’ve worked with various autoclave manufacturers, each with its own service protocols and strengths. For example, I’ve extensively used and maintained autoclaves from Tuttnauer, Steris, and Getinge. Each manufacturer has a unique approach to maintenance and service.
Tuttnauer: Known for their robust designs and user-friendly interfaces, Tuttnauer’s service protocols focus on preventative maintenance, with scheduled inspections and service visits designed to catch potential issues before they become significant problems. Their documentation is exceptionally thorough.
Steris: Steris autoclaves often incorporate advanced features, such as integrated monitoring systems and sophisticated control software. Their service protocols reflect this complexity, often including remote diagnostics and proactive alert systems. Their focus is on minimizing downtime through comprehensive monitoring.
Getinge: Getinge’s autoclaves are often found in large-scale healthcare facilities, and their service protocols emphasize validation and regulatory compliance. Their focus is on thorough documentation to ensure compliance with stringent industry standards.
In my experience, regardless of the manufacturer, proactive maintenance is key to ensuring longevity and optimal performance. This includes adherence to scheduled maintenance, prompt attention to any alarms or malfunctions, and maintaining thorough documentation of all service activities. The key is to build a strong partnership with your service provider for prompt, effective support.
Key Topics to Learn for Autoclave Maintenance and Troubleshooting Interview
- Understanding Autoclave Operation Principles: Grasp the fundamental processes of sterilization, including steam generation, pressure control, and temperature regulation. Be prepared to discuss different autoclave types and their unique operating characteristics.
- Preventive Maintenance Procedures: Detail your knowledge of routine maintenance tasks such as cleaning, lubrication, and component inspection. Explain the importance of adhering to scheduled maintenance protocols and maintaining accurate records.
- Troubleshooting Common Malfunctions: Be ready to discuss diagnosing and resolving issues like pressure leaks, temperature inconsistencies, and malfunctioning safety mechanisms. Highlight your experience with using diagnostic tools and interpreting error codes.
- Safety Regulations and Compliance: Demonstrate your understanding of relevant safety regulations and procedures for operating and maintaining autoclaves. This includes proper handling of biohazardous materials and the importance of adhering to strict safety protocols.
- Calibration and Validation: Explain the significance of regular calibration and validation procedures to ensure the autoclave’s accuracy and reliability. Discuss different validation methods and their importance in maintaining sterilization efficacy.
- Record Keeping and Documentation: Discuss the importance of meticulous record keeping for maintenance, calibration, and sterilization cycles. Explain how to properly document procedures and troubleshooting steps for compliance and traceability.
- Component Identification and Repair: Demonstrate knowledge of autoclave components and their functions. Discuss your experience repairing or replacing common parts and troubleshooting specific component failures.
Next Steps
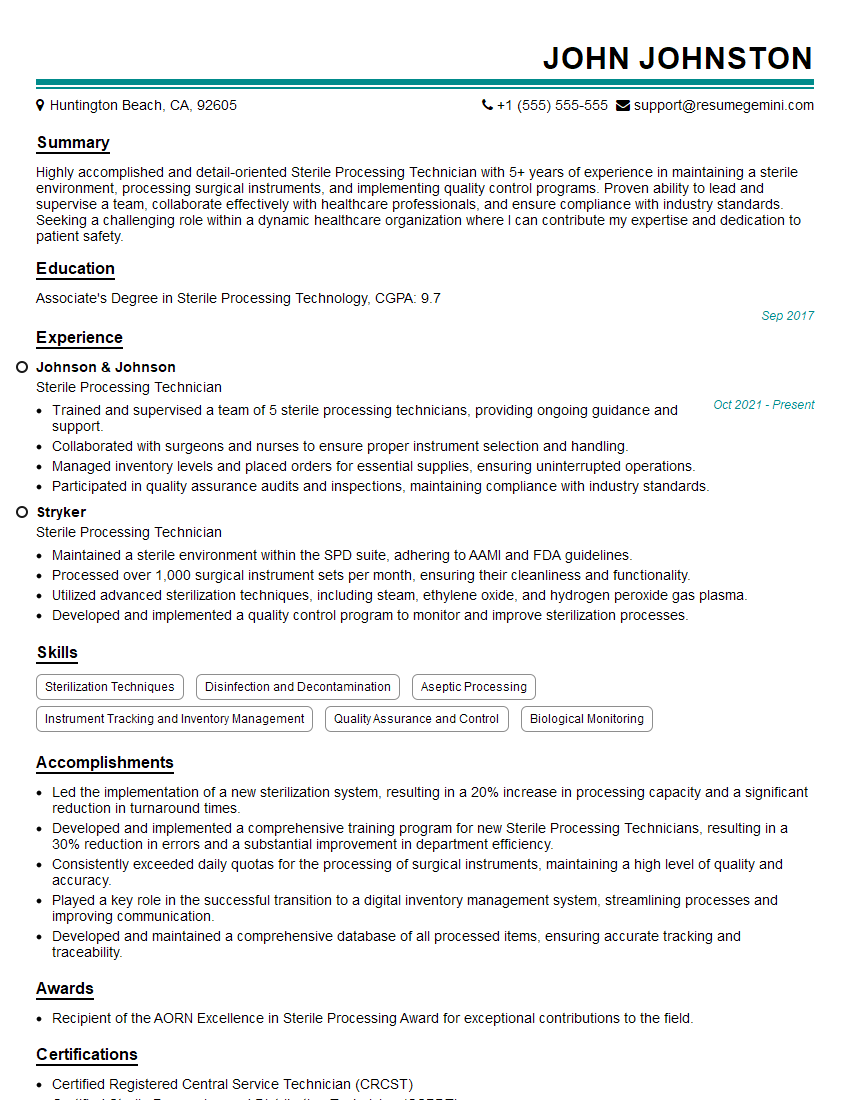
Mastering Autoclave Maintenance and Troubleshooting is crucial for career advancement in the medical, pharmaceutical, and research industries. These skills are highly sought after, opening doors to specialized roles and increased earning potential. To stand out from the competition, it’s vital to create a compelling and ATS-friendly resume that showcases your expertise effectively. ResumeGemini is a trusted resource to help you build a professional resume tailored to your specific skills and experience. They offer examples of resumes specifically designed for Autoclave Maintenance and Troubleshooting professionals, providing you with a significant advantage in your job search.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Live Rent Free!
https://bit.ly/LiveRentFREE
Interesting Article, I liked the depth of knowledge you’ve shared.
Helpful, thanks for sharing.
Hi, I represent a social media marketing agency and liked your blog
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?