Are you ready to stand out in your next interview? Understanding and preparing for Alternate Medication Administration interview questions is a game-changer. In this blog, we’ve compiled key questions and expert advice to help you showcase your skills with confidence and precision. Let’s get started on your journey to acing the interview.
Questions Asked in Alternate Medication Administration Interview
Q 1. Describe your experience administering medications via different routes (e.g., IV, IM, Subcutaneous, Oral, Topical).
My experience encompasses a wide range of medication administration routes, honed over [Number] years of practice. I’m proficient in administering medications orally, topically, intramuscularly (IM), subcutaneously (SC), and intravenously (IV). Oral administration is straightforward, involving verifying the medication and dosage before instructing the patient on how to take it. Topical application involves cleaning the area and applying the medication as directed, ensuring proper coverage. IM injections require precise technique to ensure medication reaches the muscle tissue, avoiding nerve damage. Subcutaneous injections involve administering the medication into the fatty tissue under the skin, often utilizing insulin syringes. IV administration is the most complex, demanding aseptic technique and careful monitoring for complications. Each route requires a distinct understanding of absorption rates, potential side effects, and patient-specific considerations.
For example, I once administered an emergency dose of epinephrine intramuscularly to a patient experiencing a severe allergic reaction. The rapid absorption rate of this route was critical to stabilizing the patient quickly. In another instance, I carefully titrated an IV infusion of pain medication for a post-operative patient, closely monitoring their response and vital signs.
Q 2. Explain the process of preparing and administering intravenous medications.
Preparing and administering intravenous medications requires meticulous attention to detail and adherence to strict aseptic techniques to prevent infection. The process begins with verifying the six rights of medication administration (right patient, right medication, right dose, right route, right time, right documentation). Next, I would prepare the medication by checking the expiry date, visually inspecting for particulate matter or discoloration, and carefully drawing up the prescribed dose using sterile technique. The IV line is then accessed using sterile wipes and gloves. The medication is then slowly injected into the IV line, ensuring compatibility with the existing IV fluids. Throughout the process, I monitor the patient closely for any signs of adverse reactions.
For example, when preparing a potassium chloride infusion, I always ensure it is properly diluted to prevent rapid administration, which could damage the patient’s heart. I also double-check the compatibility of the potassium chloride with the existing IV fluids. After administration, I carefully document the medication, dose, route, time, and patient response.
Q 3. What are the potential complications associated with intravenous medication administration and how would you address them?
Intravenous medication administration carries potential complications, including infection (phlebitis), infiltration (leakage into surrounding tissue), extravasation (leakage of vesicant medication into surrounding tissue), thrombosis (blood clot formation), air embolism, and allergic reactions.
- Infection: Preventing infection is paramount; meticulous aseptic technique and maintaining the integrity of the IV line are key.
- Infiltration/Extravasation: Careful insertion technique and regular site monitoring can help prevent this. If it occurs, I’ll stop the infusion, elevate the limb, apply a warm or cold compress (depending on the medication), and document the incident.
- Thrombosis: Regular flushing of the IV line and selecting appropriate IV sites can minimize the risk.
- Air embolism: This is rare but serious and requires immediate medical attention if it occurs.
- Allergic reactions: Careful medication history and monitoring for signs like rash, hives, or difficulty breathing are crucial. Emergency treatment may be needed.
A recent example involved a patient who developed phlebitis at their IV site. I immediately stopped the infusion, removed the catheter, applied a warm compress, and documented the event, notifying the physician. The patient was monitored for further complications and responded well to treatment.
Q 4. How do you verify the six rights of medication administration?
Verifying the six rights of medication administration is a non-negotiable aspect of safe medication practice. I perform these checks at multiple points in the process:
- Right Patient: I check the patient’s identification bracelet against the medication order and confirm their identity verbally.
- Right Medication: I compare the medication label to the physician’s order, checking for name, dose, and form.
- Right Dose: I double-check the prescribed dose against the available medication and calculate the correct volume or amount. I also perform independent dosage calculations to ensure accuracy.
- Right Route: I confirm the route of administration is as ordered (e.g., IV, IM, oral).
- Right Time: I check the prescribed administration schedule and adhere to it.
- Right Documentation: I carefully document the medication administered, the time, the dose, the route, and the patient’s response, along with any other pertinent observations, immediately after administration.
This multi-step approach is critical to avoid medication errors, which can have serious patient consequences. I treat this procedure as a checklist, to which I never deviate.
Q 5. Describe your experience with different types of infusion pumps and their functionalities.
My experience includes working with various infusion pumps, including volumetric pumps (delivering a set volume of medication over a specified time), syringe pumps (delivering medication from a syringe), and patient-controlled analgesia (PCA) pumps (allowing patients to self-administer pain medication). Each type has unique functionalities and programming requirements. Volumetric pumps are useful for continuous infusions, while syringe pumps are better suited for smaller volumes or medications that require precise delivery. PCA pumps provide pain relief while empowering the patient to control their analgesia.
I am familiar with the programming and troubleshooting of these devices, including setting infusion rates, checking alarms, and recognizing malfunctions. For example, I’ve used a syringe pump to administer a precise dose of a chemotherapeutic agent, and a PCA pump to manage a patient’s post-operative pain effectively.
Q 6. How do you calculate medication dosages for various routes of administration?
Dosage calculations vary depending on the medication, route of administration, and patient factors such as weight, age, and renal function. A fundamental understanding of pharmacology and mathematical principles is essential. For oral medications, the calculation might be straightforward, but intravenous, intramuscular, and subcutaneous calculations often require conversions between units (e.g., mg to mcg, mL to cc). I use standard formulas, reference drug handbooks, and double-check my calculations to ensure accuracy before administering the medication.
For example, when calculating the dose of a drug requiring weight-based adjustments, I use the formula: Dose = (Weight in kg) x (Dose per kg). If a physician orders 2mg/kg of a drug for a 70kg patient, the calculation is straightforward: Dose = 70kg * 2mg/kg = 140mg. I would then convert this dose to the appropriate volume based on the drug concentration.
Q 7. What are the safety precautions you take when handling and administering medications?
Safety is paramount in medication handling and administration. My precautions include:
- Hand Hygiene: I perform thorough handwashing before and after each medication administration procedure.
- Aseptic Technique: Strict adherence to sterile techniques is critical, especially for parenteral routes (IV, IM, SC). This includes using sterile gloves, gowns, and equipment.
- Medication Verification: As previously mentioned, rigorous verification of the six rights is non-negotiable.
- Environmental Safety: I maintain a clean and organized medication preparation area.
- Waste Disposal: I properly dispose of all used needles and other sharps in designated containers.
- Patient Education: I educate patients about their medications and any potential side effects.
- Documentation: I meticulously document all aspects of medication administration.
I always prioritize patient safety by adhering to these guidelines, ensuring that every step is completed to the highest standard. Ignoring even a single step could jeopardize patient safety.
Q 8. How do you recognize and respond to adverse reactions to medication?
Recognizing and responding to adverse medication reactions requires a keen eye for detail and prompt action. It starts with knowing the patient’s baseline – their vital signs, allergies, and pre-medication condition. During and after medication administration, I meticulously monitor for any deviations from this baseline. These deviations could manifest as a variety of symptoms:
- Changes in vital signs: A sudden drop in blood pressure, increased heart rate, or difficulty breathing could indicate a serious reaction.
- Skin reactions: Rashes, hives, itching, or swelling are common signs of allergic reactions.
- Gastrointestinal issues: Nausea, vomiting, diarrhea, or abdominal pain can also be signs of an adverse reaction.
- Neurological symptoms: Dizziness, confusion, seizures, or changes in consciousness require immediate attention.
My response is always guided by the severity of the reaction. For mild reactions, like mild itching, I might monitor the patient closely and document the findings. For more serious reactions, I immediately stop the medication administration, notify the physician or nurse practitioner, and initiate emergency protocols as needed, which could include administering counter-medications or preparing for intubation and ventilation. Accurate and timely documentation is crucial throughout this process.
For example, I once noticed a patient exhibiting rapid heart rate and shortness of breath after receiving a new antibiotic. Immediately, I stopped the infusion, notified the physician, and the patient received oxygen and appropriate countermeasures. The rapid response prevented a potentially life-threatening situation.
Q 9. Explain the process of documenting medication administration.
Documenting medication administration is not merely a bureaucratic task; it’s a critical component of patient safety and legal compliance. Each entry must be precise and complete. My documentation process typically includes:
- Patient identification: Verifying the patient’s identity using two identifiers (e.g., name and date of birth) before every medication administration.
- Medication details: Recording the medication name, dosage, route, time, and location of administration.
- Assessment data: Noting any relevant observations before and after medication administration, such as vital signs, pain levels, or any patient comments.
- Any adverse reactions: Detailed documentation of any adverse reactions, including the time of onset, symptoms, and interventions taken.
- Signature or electronic signature: Verifying the administration with a clear signature or electronic signature, depending on the facility’s system.
Think of medication documentation as a detailed medical story. Every entry contributes to a complete picture of the patient’s treatment and helps track the effectiveness and safety of the prescribed medications. Inconsistent or incomplete documentation can lead to errors and jeopardize patient safety.
Q 10. How do you handle medication errors?
Medication errors are a serious concern, and the response is multifaceted. The first step involves immediate assessment of the patient’s condition. Then:
- Notify the physician or nurse practitioner immediately: Providing them with all relevant details about the error.
- Implement necessary interventions: Administering counter-medications or other corrective actions as directed by the physician.
- Complete an incident report: This detailed report should include a clear and accurate account of the error, its cause, the steps taken to correct it, and the patient’s subsequent status.
- Follow institutional protocols: Adhering to established procedures for reporting and managing medication errors, which often includes a review to prevent similar events in the future.
I’ve personally handled medication errors involving wrong dosages or administering medication via the incorrect route. In each case, following these steps helped mitigate potential harm and ensure patient safety. Learning from errors is crucial; it improves the system and personal practice. Reporting errors without blame, with focus on system improvements is key.
Q 11. What are your experiences with electronic medication administration record (eMAR) systems?
Electronic Medication Administration Records (eMARs) have significantly enhanced medication safety and efficiency. My experience with eMAR systems includes using them to scan barcodes for medication verification, ensuring the “five rights” of medication administration (right patient, right medication, right dose, right route, right time) are consistently adhered to. eMARs also provide real-time medication administration tracking, generate alerts for potential drug interactions, and facilitate better documentation. They allow for clear and concise record keeping, minimizing errors stemming from illegible handwriting.
For instance, an eMAR can alert me to a potential drug interaction before I even administer the medication, preventing a potentially harmful situation. The integrated alerts provide an extra layer of safety. Data reporting capabilities also enable better analysis of medication trends and efficacy within the healthcare facility.
Q 12. How do you ensure patient safety during medication administration?
Ensuring patient safety during medication administration is paramount. My approach involves a multi-layered strategy encompassing various techniques. I start with the most basic steps and build upon them:
- Verification: Always verifying the patient’s identity using at least two identifiers before administering any medication.
- Five Rights: Rigorously adhering to the five rights of medication administration to prevent errors.
- Double-checking: Double-checking medication calculations and dosages to minimize mathematical errors.
- Allergy checks: Checking for allergies and potential drug interactions before administering any medication.
- Patient education: Educating the patient about the medication being administered, its purpose, potential side effects, and how to report any concerns.
- Post-administration monitoring: Closely monitoring the patient for any adverse reactions after medication administration.
Think of it like a chain—each link needs to be strong to ensure the entire process is safe. Neglecting even one aspect can compromise patient safety. Using technology like eMARs further enhances the safety measures by providing an additional layer of verification.
Q 13. Describe your understanding of different types of intravenous solutions.
Intravenous (IV) solutions are crucial for delivering fluids and medications directly into the bloodstream. They are classified based on their tonicity (how they affect the cells) and composition.
- Isotonic solutions: These have the same osmolarity as blood plasma and don’t cause a shift in fluid between the cells and the bloodstream. Examples include normal saline (0.9% NaCl) and lactated Ringer’s solution.
- Hypotonic solutions: These have lower osmolarity than blood plasma. They cause fluid to shift into the cells, potentially causing them to swell. Examples include 0.45% saline.
- Hypertonic solutions: These have higher osmolarity than blood plasma. They draw fluid out of the cells, potentially causing them to shrink. Examples include 3% saline.
The choice of IV solution depends on the patient’s specific needs. For example, isotonic solutions are often used for hydration, while hypotonic solutions might be used to treat cellular dehydration. Hypertonic solutions might be used to treat certain fluid imbalances, but require careful monitoring due to potential risks.
Q 14. What is your experience with central venous catheters (CVCs)?
Central venous catheters (CVCs) are essential for long-term intravenous access, providing a route for administering fluids, medications, and parenteral nutrition. My experience includes inserting, maintaining, and troubleshooting CVCs. This involves:
- Insertion technique: Following sterile technique to minimize the risk of infection.
- Site care: Providing regular site care to prevent complications like infection and thrombosis.
- Fluid and medication administration: Administering fluids and medications via the CVC, carefully monitoring the patient for any adverse reactions.
- Troubleshooting: Identifying and resolving any complications, such as catheter occlusion or infection.
- Removal: Safely removing the CVC when it is no longer needed.
CVCs, while providing vital access, carry a risk of infection and other complications. Therefore, meticulous attention to sterile technique and careful monitoring of the insertion site are paramount. For example, proper flushing techniques are critical for preventing catheter occlusion. A patient’s response to the CVC procedure, post-insertion, is crucial to monitor. Regular assessment and thorough documentation of the procedure help reduce the chances of complications and are vital to patient safety.
Q 15. How do you manage medication incompatibility issues?
Medication incompatibility is a serious concern, potentially leading to adverse drug reactions or rendering the medication ineffective. Managing it involves a multi-step process starting with a thorough review of the medication administration record (MAR). I always cross-reference the MAR with the patient’s complete medication profile, including over-the-counter drugs and supplements, to identify potential interactions. This includes checking for physical incompatibilities like precipitation or discoloration when mixing medications in the same syringe or infusion bag.
Secondly, I rely heavily on pharmaceutical resources, like drug interaction databases and hospital formularies, to verify compatibility. For instance, if a patient requires both heparin and an aminoglycoside, I’d consult these resources to ensure compatibility and determine the optimal administration sequence or method to avoid issues. If incompatibility is identified, I immediately consult with the pharmacist to find an alternative solution – perhaps administering the drugs through separate IV lines or at different times, or switching to an equivalent medication with better compatibility.
For example, I once encountered incompatibility between two antibiotics intended for intravenous administration. By consulting the formulary, we discovered that administering them through separate IV lines, flushed with saline in between, was the safest approach. Finally, meticulous documentation of the incompatibility, the steps taken to resolve it, and the final administration plan is crucial for patient safety and legal compliance.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Describe your experience with PICC line insertion and maintenance.
I have extensive experience with PICC line insertion and maintenance, having participated in numerous procedures and provided ongoing care for countless patients. My role typically involves assisting the physician or nurse practitioner during the insertion procedure, ensuring the patient’s comfort and monitoring vital signs. Post-insertion, my responsibilities include meticulous site care to prevent infection—this involves regular assessment of the insertion site for signs of inflammation, redness, or drainage. I teach patients and caregivers proper hygiene techniques for maintaining the PICC line and educate them on recognizing signs of infection or complications.
Regular flushing of the PICC line with appropriate solutions (usually saline) is vital to prevent clotting. I am proficient in executing this procedure using aseptic techniques, carefully monitoring the patient’s response throughout. Additionally, I’m skilled in drawing blood samples via the PICC line, utilizing appropriate precautions to avoid contamination. Managing complications like infiltration or thrombophlebitis also falls under my purview, which involves taking immediate action to address the issue, often requiring immediate communication with the physician or nurse practitioner.
I remember a patient who developed a mild infiltration at their PICC site. I immediately stopped the infusion, elevated the limb, and applied a warm compress. I closely monitored the site and documented the incident, escalating it to the physician for further assessment. Early intervention prevented significant complications.
Q 17. How do you assess a patient’s readiness for medication administration?
Assessing patient readiness for medication administration is a critical step that ensures safety and efficacy. It encompasses several facets. First, I always verify the patient’s identity using at least two identifiers (name and date of birth). This crucial step prevents medication errors. Then I thoroughly review the medication order, ensuring it’s accurate, complete, and appropriate for the patient. This includes checking the medication name, dose, route, frequency, and any relevant allergies or contraindications.
Next, I assess the patient’s physical and mental condition. For instance, can they safely swallow an oral medication? Are they alert and oriented enough to understand the medication instructions? For intravenous medications, the integrity of the IV access site is critical. If the patient is receiving subcutaneous injections, I assess the chosen injection site for any contraindications like bruising, lesions, or inflammation.
Furthermore, I always consider the patient’s understanding of the medication. I explain the purpose, dosage, side effects, and potential interactions in terms they can easily understand, ensuring they provide informed consent. This ensures they understand what to expect and what to report. If the patient has a family member or caregiver present, I include them in the education process, ensuring they know how to support the patient’s medication regimen.
Q 18. What is your experience with pain management via alternate routes?
My experience with pain management via alternate routes is substantial. I have administered numerous medications via different routes, including intravenous, subcutaneous, intramuscular, transdermal, and rectal routes. The choice of route depends on several factors, including the type of pain, the patient’s condition, and the properties of the analgesic medication. For instance, acute, severe pain often necessitates intravenous administration for rapid onset of action.
Subcutaneous administration is suitable for sustained-release analgesics, where a slower, more prolonged pain relief is desired. Transdermal patches provide consistent drug delivery over an extended period. Rectal administration can be beneficial for patients who are unable to take oral medications. I always carefully monitor the patient’s response to the pain medication, assessing both the intensity and duration of pain relief, as well as the presence of any adverse effects. I meticulously document these observations to inform subsequent pain management strategies.
I recall a patient with severe post-operative pain. While intravenous morphine provided immediate relief, we later transitioned to a patient-controlled analgesia (PCA) pump to empower the patient to manage their pain effectively. This involved educating the patient on the proper use of the pump and monitoring their respiratory rate and sedation levels. The patient’s pain was managed effectively, leading to improved comfort and faster recovery. This highlights the importance of adapting pain management strategies to suit individual needs and preferences.
Q 19. Explain your understanding of pharmacokinetics and pharmacodynamics.
Pharmacokinetics describes what the body does to a drug, encompassing absorption, distribution, metabolism, and excretion (ADME). Absorption refers to how the drug enters the bloodstream. Distribution details how the drug spreads throughout the body. Metabolism describes the process of breaking down the drug in the liver, and excretion explains how the body eliminates the drug, primarily through the kidneys. These processes influence the drug’s concentration in the body over time.
Pharmacodynamics, conversely, describes what the drug does to the body. It encompasses the drug’s mechanism of action, its effects on the body, and the relationship between drug concentration and its therapeutic effect. Understanding both pharmacokinetics and pharmacodynamics is essential for choosing the appropriate medication, dosage, and route of administration. For example, a drug with rapid absorption and short half-life might be suitable for acute pain relief, whereas a drug with slow absorption and a long half-life might be better suited for chronic pain management.
Understanding these concepts helps predict a drug’s effectiveness and potential side effects. If a patient experiences unexpected side effects or a lack of therapeutic effect, reviewing the pharmacokinetic and pharmacodynamic properties of the drug can provide valuable insights into adjusting the treatment plan.
Q 20. How do you educate patients and family members about medication administration?
Educating patients and their families about medication administration is a crucial aspect of my role. I always employ a patient-centered approach, tailoring my explanations to the individual’s level of understanding. I start by explaining the purpose of each medication, its intended effects, and the potential side effects in simple, non-technical terms, using analogies whenever possible to enhance comprehension. I also demonstrate the proper techniques for medication administration, offering hands-on training and visual aids whenever feasible.
I strongly advocate for active participation, encouraging patients and families to ask questions and clarify any doubts. I provide written instructions, ensuring they are clear and easy to follow. I also schedule follow-up conversations to address any concerns that may arise after the initial education session. If a patient is struggling to manage their medication regimen, I collaborate with other healthcare professionals, such as pharmacists or social workers, to develop a supportive plan.
For instance, I once educated a patient’s family on administering insulin injections. I provided step-by-step instructions, demonstrated the technique, and encouraged them to practice. I also provided written instructions and a contact number for follow-up support. This patient-centered approach empowered the family, ensuring they could safely administer the medication.
Q 21. Describe your experience with subcutaneous injections.
Subcutaneous injections involve administering medications into the fatty tissue just below the skin. I have extensive experience in this technique, employing aseptic techniques to prevent infection. The choice of injection site is crucial; common areas include the abdomen, outer thighs, and upper arms. The skin is cleansed with an antiseptic solution before the injection. I use a 25-30 gauge needle appropriate for subcutaneous administration, and I select the site carefully, avoiding areas with bruising, scars, or inflammation.
The injection itself is administered slowly, ensuring the medication is deposited into the subcutaneous tissue. After the injection, the needle is withdrawn, and gentle pressure is applied to the injection site to minimize bleeding or bruising. I always teach patients or caregivers proper injection techniques, including selecting appropriate injection sites, preparing the medication correctly, and disposing of needles safely. I also educate them on recognizing signs of complications, such as infection or hematoma formation.
For example, I often teach patients with diabetes how to self-administer insulin injections. I guide them through each step, highlighting the importance of correct technique and self-monitoring to prevent complications.
Q 22. What are the considerations for administering medications to pediatric or geriatric patients?
Administering medication to pediatric and geriatric patients requires extra care due to their physiological differences compared to adults. Dosage calculations are crucial and often require precise adjustments based on weight, body surface area, or age-specific considerations.
- Pediatric Patients: Their smaller size necessitates smaller doses and careful selection of administration routes. Oral medications might be challenging if the child refuses or can’t swallow pills. Intramuscular injections require smaller needles and precise injection sites to avoid complications. We must also consider developmental stages, psychological factors (fear of needles), and the need for parental/guardian involvement.
- Geriatric Patients: Older adults often have multiple comorbidities and take multiple medications, increasing the risk of drug interactions. Age-related physiological changes, such as reduced kidney and liver function, impact drug metabolism and excretion, potentially leading to toxicity. Decreased cognitive function may affect adherence to medication regimens. We need to assess their physical abilities, dexterity, and visual acuity to choose the most appropriate administration method. For example, using easy-to-open containers or pre-filled syringes may improve compliance.
For both populations, thorough assessment of the patient’s condition, accurate dosage calculation, and careful monitoring for adverse effects are paramount. Clear communication with the patient and their families is vital to ensuring safe and effective medication administration.
Q 23. How do you handle difficult IV insertions or infiltration?
Difficult IV insertions or infiltrations require a systematic approach. First, we assess the site thoroughly for any signs of infection or inflammation. If the initial attempt is unsuccessful, we would consider alternative sites, possibly using ultrasound guidance for better visualization of vessels.
If infiltration occurs (fluid leaking into surrounding tissue), we immediately stop the infusion, remove the IV cannula, elevate the affected limb, and apply a warm compress to alleviate discomfort. Documentation is crucial, including the time, location, and assessment of the infiltration. Depending on the severity, we might consider administering analgesics or anti-inflammatory medications. In severe cases, local interventions or pharmacological treatment might be necessary.
For repeated difficulty, we re-evaluate the patient’s vascular access options. This might involve consulting a vascular access specialist or considering alternative routes like a central venous catheter if peripheral access remains challenging. We continuously monitor the patient for any signs of complications, such as cellulitis or thrombophlebitis.
Q 24. What is your experience with Total Parenteral Nutrition (TPN)?
Total Parenteral Nutrition (TPN) involves administering nutrition intravenously when the patient’s gastrointestinal tract cannot absorb sufficient nutrients. My experience includes preparing and administering TPN solutions, which is a sterile procedure requiring meticulous attention to detail.
This involves calculating the exact nutrient composition based on the patient’s individual needs, including carbohydrates, proteins, lipids, vitamins, and electrolytes. The preparation process necessitates a laminar flow hood to maintain sterility, and all components must be accurately measured and mixed to prevent contamination and medication errors.
After the solution is prepared, it is hung on an infusion pump for controlled delivery. Close monitoring of the patient’s blood glucose, electrolyte levels, and overall nutritional status is essential to adjust the TPN formulation as needed. Potential complications like infections, hyperglycemia, or electrolyte imbalances need prompt recognition and management.
Q 25. Describe your knowledge of different types of needles and syringes.
Various needles and syringes are used depending on the medication, administration route, and patient’s condition.
- Needles: These vary in gauge (diameter) and length. Smaller gauge needles (e.g., 25-gauge) are used for subcutaneous injections, while larger gauge needles (e.g., 18-gauge) might be required for IV administration. Needle length depends on the injection site and patient’s anatomy.
- Syringes: Syringes are available in different sizes (volumes) depending on the medication volume to be administered, typically ranging from 1ml to 60ml. Insulin syringes are calibrated in units, not milliliters, for precise insulin dosing.
Knowing the appropriate needle and syringe to use is critical to avoid complications. For example, using a needle that is too large can cause tissue damage, while a needle that is too small can cause pain and hinder the administration process. Proper selection ensures comfort and minimizes risks for the patient.
Q 26. How do you maintain sterility during medication preparation and administration?
Maintaining sterility during medication preparation and administration is paramount to prevent infections. We adhere strictly to aseptic techniques. This includes hand hygiene, wearing clean gloves and gowns, and using sterile equipment and supplies.
Medication preparation takes place in a clean environment, ideally a laminar flow hood for TPN preparation. All equipment and supplies are meticulously inspected for any signs of damage or contamination before use. We follow specific procedures for drawing up medications and preparing intravenous infusions to ensure that no contamination occurs.
During administration, the injection site is thoroughly cleaned with an antiseptic solution to reduce the risk of infection. We use proper techniques for intravenous access, ensuring the integrity of the IV line and using sterile connectors to minimize contamination risk. After administration, proper disposal of used needles and syringes into designated sharps containers is crucial to minimize the risk of accidental needlesticks.
Q 27. Explain your understanding of medication reconciliation.
Medication reconciliation is a process of comparing a patient’s medication orders with the medications they are currently taking. This crucial step helps prevent medication errors, adverse drug reactions, and duplication.
It typically involves comparing medication lists from various sources, including the patient’s home medication list, the physician’s orders, and the hospital’s pharmacy records. Any discrepancies are identified, investigated, and resolved to ensure medication safety and efficacy.
For example, a patient admitted to the hospital might be taking a particular medication at home, but the hospital’s order might omit it. Medication reconciliation would identify this discrepancy, allowing the medical team to clarify the dosage and administration instructions, ensuring the patient receives the appropriate medication without interruption or error. This process is particularly important for patients with multiple chronic conditions or those taking numerous medications.
Q 28. How do you stay updated on current best practices for medication administration?
Staying updated on current best practices in medication administration is a continuous process. I utilize several strategies to ensure my knowledge remains current.
- Professional Organizations: Active membership in professional organizations like the Infusion Nurses Society (INS) or similar groups provides access to continuing education opportunities, publications, and guidelines.
- Journals and Publications: I regularly review peer-reviewed journals and professional publications focused on pharmacology, medication safety, and IV therapy.
- Continuing Education Courses: I actively participate in workshops, conferences, and online courses to enhance my knowledge and skills in medication administration.
- Institutional Policies and Procedures: I closely follow our institution’s policies and procedures, which are regularly updated based on the latest evidence-based practices and guidelines.
- Collaboration and Teamwork: Frequent discussions and collaboration with pharmacists, physicians, and other healthcare professionals ensure best practice implementation.
This multi-faceted approach guarantees that I am consistently informed about the latest advancements and safety measures in medication administration, enabling me to provide the highest quality of care.
Key Topics to Learn for Alternate Medication Administration Interview
- Routes of Administration: Understanding and comparing various routes (oral, sublingual, transdermal, topical, inhalation, rectal, etc.), including advantages, disadvantages, and patient considerations for each.
- Pharmacokinetics and Pharmacodynamics: How different routes affect drug absorption, distribution, metabolism, and excretion; relating this to patient outcomes and medication effectiveness.
- Medication Calculations: Mastering accurate dosage calculations for different routes and formulations, demonstrating proficiency in solving practical problems related to medication preparation and administration.
- Safety and Compliance: Understanding and applying principles of safe medication administration, including the “six rights” (right patient, right medication, right dose, right route, right time, right documentation), and recognizing potential errors and adverse effects.
- Legal and Ethical Considerations: Familiarity with relevant laws, regulations, and ethical guidelines governing medication administration, including patient consent and confidentiality.
- Patient Education and Communication: Explaining medication regimens clearly and effectively to patients, addressing their concerns, and ensuring understanding of instructions for safe and effective medication use.
- Emergency Situations: Knowing how to handle unexpected situations, such as medication errors, adverse reactions, or emergency medication administration.
- Documentation and Record Keeping: Maintaining accurate and thorough records of medication administration, adhering to established protocols and demonstrating meticulous attention to detail.
- Technology in Medication Administration: Familiarity with automated medication dispensing systems, electronic health records (EHRs), and other technological advancements impacting medication management.
Next Steps
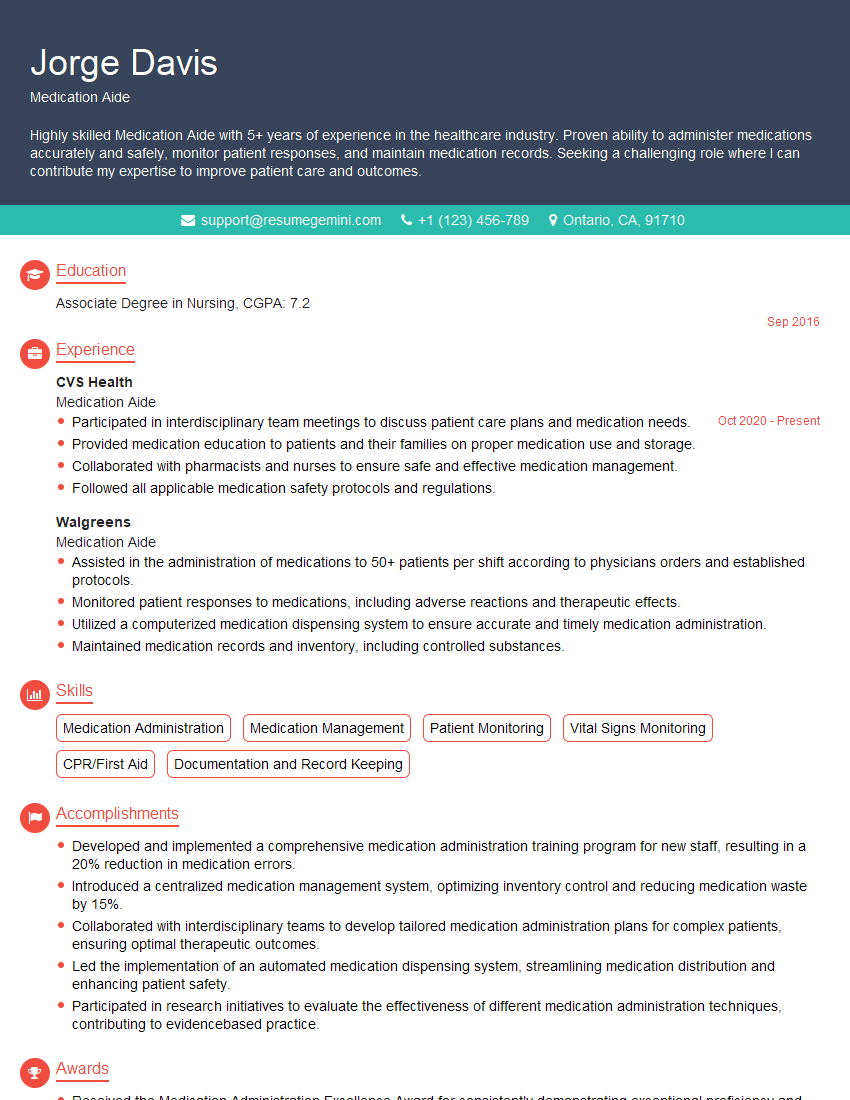
Mastering Alternate Medication Administration significantly enhances your career prospects in healthcare, opening doors to advanced roles and increased responsibility. A strong resume is crucial for showcasing your skills and experience to potential employers. To maximize your job search success, create an ATS-friendly resume that highlights your expertise in this critical area. We recommend using ResumeGemini, a trusted resource, to build a professional and impactful resume. ResumeGemini provides examples of resumes tailored to Alternate Medication Administration to help you create a compelling application.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Take a look at this stunning 2-bedroom apartment perfectly situated NYC’s coveted Hudson Yards!
https://bit.ly/Lovely2BedsApartmentHudsonYards
Live Rent Free!
https://bit.ly/LiveRentFREE
Interesting Article, I liked the depth of knowledge you’ve shared.
Helpful, thanks for sharing.
Hi, I represent a social media marketing agency and liked your blog
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?