The right preparation can turn an interview into an opportunity to showcase your expertise. This guide to Hematology and Coagulation interview questions is your ultimate resource, providing key insights and tips to help you ace your responses and stand out as a top candidate.
Questions Asked in Hematology and Coagulation Interview
Q 1. Describe the process of hemostasis.
Hemostasis is the physiological process that stops bleeding. It’s a complex cascade of events involving multiple components of the blood and the blood vessel wall, ensuring that blood loss is contained after vascular injury. Think of it as the body’s natural ‘plug’ for a leak in the plumbing system. This process can be broadly divided into three stages:
- Vascular Spasm: The immediate response to injury is vasoconstriction, reducing blood flow to the injured area. It’s like temporarily squeezing a pipe to reduce water flow.
- Primary Hemostasis (Platelet Plug Formation): Platelets adhere to the exposed subendothelial collagen, forming a temporary platelet plug. This is like using a small patch to cover the leak.
- Secondary Hemostasis (Coagulation Cascade): A complex series of enzymatic reactions involving coagulation factors leads to the formation of a stable fibrin clot that reinforces the platelet plug. This is like applying a stronger, more permanent seal over the patch.
Failure at any of these stages can lead to bleeding disorders.
Q 2. Explain the role of platelets in primary hemostasis.
Platelets are anuclear cell fragments crucial for primary hemostasis. Their role is multifaceted:
- Adhesion: Platelets adhere to exposed collagen at the site of injury via von Willebrand factor (vWF), acting as a bridge between the collagen and the platelet receptor glycoprotein Ib/IX/V.
- Activation: Upon adhesion, platelets undergo activation, changing shape and releasing granules containing various factors such as ADP, thromboxane A2, and serotonin. These factors amplify platelet aggregation.
- Aggregation: Activated platelets aggregate together, forming a platelet plug, sealing the vascular defect. This aggregation is mediated mainly by fibrinogen binding to glycoprotein IIb/IIIa receptors on the activated platelets.
Imagine platelets as tiny construction workers. They rush to the site of damage, stick to the damaged area, and then signal for more workers to help build a temporary dam to stop the bleeding.
Q 3. What are the coagulation factors and their function?
Coagulation factors are proteins primarily synthesized in the liver that participate in the coagulation cascade. They are usually designated by Roman numerals (I-XIII), with some exceptions. Each factor has a specific role, working in a tightly regulated sequence:
- Factor I (Fibrinogen): The final product of the coagulation cascade; converted to fibrin to form the clot.
- Factor II (Prothrombin): Converted to thrombin, a key enzyme in the process.
- Factor III (Tissue Factor): Initiates the extrinsic pathway.
- Factor V (Proaccelerin): Cofactor that accelerates several steps in the cascade.
- Factor VII (Proconvertin): Initiates the extrinsic pathway.
- Factor VIII (Antihemophilic Factor A): Crucial in the intrinsic pathway.
- Factor IX (Antihemophilic Factor B or Christmas Factor): Essential for the intrinsic pathway.
- Factor X (Stuart-Prower Factor): Critical component of both intrinsic and extrinsic pathways.
- Factor XI (Plasma Thromboplastin Antecedent): Part of the intrinsic pathway.
- Factor XII (Hageman Factor): Initiates the intrinsic pathway.
- Factor XIII (Fibrin-Stabilizing Factor): Cross-links fibrin, stabilizing the clot.
Deficiencies in these factors can cause bleeding disorders of varying severity.
Q 4. Explain the intrinsic and extrinsic pathways of coagulation.
The coagulation cascade is traditionally divided into intrinsic and extrinsic pathways, which converge into a common pathway.
- Intrinsic Pathway: Activated by contact with negatively charged surfaces (e.g., collagen) within the vascular system. It’s slower and involves factors XII, XI, IX, VIII, X.
- Extrinsic Pathway: Activated by tissue factor (TF), released from damaged tissues. It’s faster and involves factors VII, X, and tissue factor.
While traditionally taught as separate, it’s now understood that the pathways interact and influence each other, with the extrinsic pathway often being the primary initiator of clotting in vivo. Imagine them as two roads leading to the same highway (the common pathway).
Q 5. Describe the common pathway of coagulation.
The common pathway is where the intrinsic and extrinsic pathways converge. It begins with the activation of Factor X, which converts prothrombin (Factor II) to thrombin. Thrombin then converts fibrinogen (Factor I) to fibrin, forming the stable fibrin clot. This is the final and crucial step in the process of hemostasis.
Think of this as the main highway where both roads (intrinsic and extrinsic pathways) merge to reach the final destination (fibrin clot formation).
Q 6. What is the role of Vitamin K in coagulation?
Vitamin K is an essential cofactor for the synthesis of several coagulation factors, specifically Factors II, VII, IX, and X, as well as proteins C and S. These proteins require Vitamin K-dependent carboxylation of glutamic acid residues for their proper function. This modification allows them to bind calcium ions, which is crucial for their activity in the coagulation cascade. Without vitamin K, these factors are non-functional, resulting in impaired coagulation and increased bleeding risk. This is why individuals on anticoagulant medications like warfarin (Coumadin) which interferes with Vitamin K metabolism are carefully monitored.
Q 7. How do you interpret a PT/INR result?
PT (Prothrombin Time) measures the time it takes for a blood clot to form via the extrinsic and common pathways. INR (International Normalized Ratio) standardizes the PT results across different laboratories, making them comparable. A normal PT/INR result typically ranges from 1.0-1.3.
- Elevated PT/INR: Indicates a prolonged clotting time, which may be due to deficiencies in coagulation factors (e.g., liver disease, Vitamin K deficiency), or anticoagulant use.
- Decreased PT/INR: Indicates a shorter clotting time, potentially suggesting a hypercoagulable state (increased tendency to clot), although this is less common.
Interpreting PT/INR requires considering the clinical context. For example, an elevated INR in a patient on warfarin is expected and therapeutic within a certain range, whereas an elevated INR in a patient not on anticoagulants indicates a potential bleeding disorder or liver disease. The specific therapeutic range for INR will depend on the condition being treated.
Q 8. How do you interpret an aPTT result?
The activated partial thromboplastin time (aPTT) is a blood test that measures the time it takes for blood to clot. It assesses the intrinsic and common pathways of the coagulation cascade. A normal aPTT result indicates that these pathways are functioning correctly. A prolonged aPTT suggests a problem somewhere in these pathways.
Interpreting an aPTT result involves considering the reference range provided by the laboratory. A result above the upper limit of normal indicates a prolonged aPTT. The degree of prolongation can give clues about the severity of the coagulation disorder. However, the aPTT alone is insufficient for diagnosis; it requires correlation with other tests like PT (prothrombin time), and often further investigations like mixing studies to differentiate between factor deficiencies and the presence of inhibitors.
For example, a significantly prolonged aPTT might indicate a deficiency in one or more clotting factors (like hemophilia A or B), the presence of a lupus anticoagulant, or liver disease affecting clotting factor synthesis. A mildly prolonged aPTT may be caused by medications such as heparin, or may be a borderline result needing repeat testing.
Q 9. What are the causes of prolonged PT and aPTT?
Prolonged prothrombin time (PT) and aPTT both signify problems within the coagulation cascade, but affect different parts of the process. PT assesses the extrinsic and common pathways, while aPTT assesses the intrinsic and common pathways. A prolonged PT indicates a defect in the extrinsic pathway or the common pathway, while a prolonged aPTT indicates a problem in the intrinsic or common pathway.
- Causes of prolonged PT: Vitamin K deficiency (essential for several clotting factors), liver disease (reduced clotting factor synthesis), disseminated intravascular coagulation (DIC – widespread clotting and depletion of clotting factors), warfarin therapy (anticoagulant medication), factor VII deficiency.
- Causes of prolonged aPTT: Hemophilia A (factor VIII deficiency), Hemophilia B (factor IX deficiency), von Willebrand disease (affecting factor VIII and platelet function), lupus anticoagulant (autoantibody interfering with clotting), heparin therapy (anticoagulant medication), deficiencies in factors XII, XI, X, IX, VIII, or V.
It is crucial to remember that multiple factors can contribute to prolonged PT and aPTT, and a thorough evaluation is necessary to determine the underlying cause. This often involves a detailed patient history, physical examination, and additional coagulation tests.
Q 10. Explain the difference between Hemophilia A and Hemophilia B.
Both Hemophilia A and Hemophilia B are inherited bleeding disorders caused by a deficiency in clotting factors, leading to prolonged bleeding times. The key difference lies in the specific factor deficient:
- Hemophilia A: A deficiency in factor VIII (antihemophilic factor). This is the more common type of hemophilia.
- Hemophilia B (Christmas disease): A deficiency in factor IX (Christmas factor).
Both conditions result in impaired blood clotting, leading to spontaneous bleeding or excessive bleeding after injury or surgery. The severity of symptoms varies depending on the level of factor deficiency. Diagnosis involves measuring factor VIII and IX levels in the blood using specific assays.
Imagine the clotting cascade as a chain reaction; each factor activates the next. In Hemophilia A, the missing link is factor VIII, halting the cascade and preventing proper clot formation. Similarly, in Hemophilia B, the absence of factor IX interrupts the chain.
Q 11. Describe the pathophysiology of Von Willebrand Disease.
Von Willebrand disease (VWD) is the most common inherited bleeding disorder. It’s characterized by a deficiency or dysfunction of von Willebrand factor (VWF), a large protein that plays a crucial role in primary hemostasis (the initial stages of blood clotting). VWF has two major functions:
- Carrier protein for factor VIII: VWF binds and protects factor VIII, preventing its degradation. A deficiency in VWF can lead to reduced levels of functional factor VIII, indirectly impacting the coagulation cascade (as seen in hemophilia A).
- Platelet adhesion: VWF mediates platelet adhesion to the injured vessel wall, facilitating the formation of a platelet plug, the first step in blood clot formation.
The pathophysiology of VWD varies depending on the type. Type 1 VWD involves a quantitative deficiency of VWF (less VWF). Type 2 involves qualitative defects (VWF is present but doesn’t function properly). Type 3 is characterized by almost complete absence of VWF.
This leads to symptoms ranging from mild to severe bleeding, depending on the severity and type of VWD. Common symptoms include easy bruising, prolonged nosebleeds, heavy menstrual bleeding, and excessive bleeding after surgery or injury. Diagnosis relies on measuring VWF antigen levels and activity, as well as factor VIII levels.
Q 12. What are the different types of anemia?
Anemia is a condition characterized by a deficiency of red blood cells or hemoglobin in the blood, resulting in reduced oxygen-carrying capacity. Anemia can be broadly classified into several types based on the underlying cause:
- Macrocytic anemias: Characterized by large, immature red blood cells (megaloblasts). Common causes include vitamin B12 deficiency (pernicious anemia) and folate deficiency.
- Normocytic anemias: Characterized by normal-sized red blood cells but reduced in number. Causes include acute blood loss, chronic diseases (anemia of chronic disease), and aplastic anemia.
- Microcytic anemias: Characterized by small, pale red blood cells. The most common cause is iron deficiency anemia, but other causes include thalassemia and sideroblastic anemia.
- Hemolytic anemias: Characterized by increased destruction of red blood cells. Causes can include inherited conditions like sickle cell anemia and thalassemia, as well as acquired conditions like autoimmune hemolytic anemia.
The classification helps guide further investigations to pinpoint the specific cause of the anemia.
Q 13. Explain the causes and diagnosis of iron deficiency anemia.
Iron deficiency anemia is the most common type of anemia worldwide, resulting from insufficient iron in the body. Iron is crucial for hemoglobin production, the protein in red blood cells that carries oxygen. Insufficient iron leads to smaller, paler red blood cells (microcytic) with lower hemoglobin levels, resulting in decreased oxygen-carrying capacity.
Causes:
- Dietary deficiency: Inadequate intake of iron-rich foods (meat, leafy greens, legumes).
- Blood loss: Chronic blood loss from conditions like heavy menstrual bleeding, gastrointestinal bleeding (ulcers, colon cancer), or internal bleeding.
- Malabsorption: Conditions that impair iron absorption from the gastrointestinal tract (e.g., celiac disease, Crohn’s disease).
- Increased iron demand: Pregnancy, rapid growth in children.
Diagnosis: Diagnosis typically involves:
- Complete blood count (CBC): Reveals low hemoglobin, hematocrit, and red blood cell indices (MCV, MCH, MCHC indicating microcytic, hypochromic anemia).
- Serum ferritin levels: Measures the amount of stored iron in the body. Low ferritin is indicative of iron deficiency.
- Serum iron levels: Measures the amount of iron in the blood. Usually decreased in iron deficiency.
- Transferrin saturation: Reflects the amount of iron bound to transferrin, a protein that transports iron. Usually decreased in iron deficiency.
Further investigations may be needed to identify the cause of iron deficiency (e.g., stool tests to check for gastrointestinal bleeding).
Q 14. Describe the pathophysiology of sickle cell anemia.
Sickle cell anemia is a severe, inherited disorder characterized by abnormal hemoglobin S (HbS). HbS differs from normal hemoglobin A (HbA) by a single amino acid substitution. This seemingly small change has profound consequences.
Pathophysiology: Under low-oxygen conditions, HbS polymerizes (clumps together), causing red blood cells to deform into a sickle shape. These rigid, sickle-shaped cells are less flexible and prone to clogging small blood vessels (vasoocclusion), leading to a cascade of complications:
- Vasoocclusive crises: Painful episodes due to blocked blood flow to organs and tissues.
- Hemolysis: Premature destruction of sickle cells, leading to anemia.
- Organ damage: Repeated episodes of vasoocclusion can damage various organs, including the spleen, kidneys, lungs, and brain.
- Infection susceptibility: Impaired spleen function increases susceptibility to infections.
The sickling process is cyclical: low oxygen levels cause sickling, which further reduces oxygen delivery, leading to more sickling. This chronic hemolysis and vasoocclusion are the hallmarks of sickle cell anemia’s pathophysiology. The severity of the disease varies, depending on the percentage of HbS in the blood.
Q 15. What are the different types of leukemia?
Leukemia is a cancer of the blood-forming tissues, primarily affecting the bone marrow. There are two main categories: acute and chronic, further subdivided by the type of blood cell affected (myeloid or lymphoid).
- Acute Leukemias: These progress rapidly and require immediate treatment.
- Acute Myeloid Leukemia (AML): Affects myeloid cells (which give rise to red blood cells, platelets, and some white blood cells).
- Acute Lymphoblastic Leukemia (ALL): Affects lymphoid cells (which develop into lymphocytes, a type of white blood cell involved in immune response).
- Chronic Leukemias: These progress more slowly, sometimes developing over many years.
- Chronic Myeloid Leukemia (CML): A myeloid leukemia characterized by a specific genetic abnormality, the Philadelphia chromosome.
- Chronic Lymphocytic Leukemia (CLL): A lymphoid leukemia affecting mature B lymphocytes.
Understanding these categories is crucial for appropriate diagnosis and treatment planning, as each type responds differently to therapy.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Explain the diagnostic criteria for acute myeloid leukemia (AML).
Diagnosing AML involves a combination of clinical findings, blood tests, and bone marrow examination. The key criteria include:
- Peripheral blood findings: A CBC typically shows anemia (low red blood cells), thrombocytopenia (low platelets), and an elevated white blood cell count that often includes blasts (immature myeloid cells). However, it’s important to note that sometimes the WBC count can be normal or even low.
- Bone marrow examination: A bone marrow biopsy and aspirate are crucial for confirming the diagnosis. This shows the percentage of blasts (usually >20% is diagnostic), cytogenetic abnormalities, and other features characteristic of AML subtypes.
- Cytochemical stains and flow cytometry: These specialized tests help identify and characterize the blasts, providing information about the specific type of AML.
- Molecular studies: These tests detect specific gene mutations, which can impact prognosis and treatment decisions. Examples include FLT3 mutations and NPM1 mutations.
Meeting these criteria allows clinicians to confidently diagnose AML and initiate appropriate treatment strategies tailored to the patient’s specific subtype and risk factors.
Q 17. Describe the presentation of multiple myeloma.
Multiple myeloma is a cancer of plasma cells, a type of white blood cell that produces antibodies. The presentation is highly variable, but common features include:
- Bone pain: Often the initial symptom, due to bone lesions caused by plasma cell infiltration.
- Anemia: Plasma cell infiltration of the bone marrow reduces red blood cell production.
- Hypercalcemia: Elevated calcium levels in the blood, due to bone destruction.
- Renal failure: Due to the accumulation of abnormal proteins produced by myeloma cells.
- Recurrent infections: Due to impaired antibody production.
- Laboratory findings: Elevated levels of monoclonal immunoglobulin (M protein) in the blood and urine, as well as an elevated level of Beta-2-microglobulin are commonly found.
These symptoms can significantly impact a patient’s quality of life. Diagnosis requires bone marrow biopsy, showing clonal plasma cells, along with supporting laboratory findings.
Q 18. What are the different types of lymphoma?
Lymphoma is a cancer of the lymphatic system, which is part of the immune system. The two main categories are Hodgkin Lymphoma and Non-Hodgkin Lymphoma.
- Hodgkin Lymphoma: Characterized by the presence of Reed-Sternberg cells, a type of abnormal lymphocyte. It typically involves contiguous lymph node spread.
- Non-Hodgkin Lymphoma: A heterogeneous group of lymphomas with various presentations and behaviors. These lymphomas are further classified by cell type (B-cell, T-cell, or NK-cell) and by their aggressiveness (low-grade, intermediate-grade, or high-grade).
Staging is crucial in both types to determine the extent of the disease and guide treatment. The treatment strategies differ greatly between Hodgkin and Non-Hodgkin lymphomas and even within the subtype of Non-Hodgkin Lymphoma.
Q 19. What are the common causes of thrombocytopenia?
Thrombocytopenia refers to a low platelet count, increasing the risk of bleeding. Several factors can cause it:
- Decreased platelet production: This can be due to bone marrow disorders (like leukemia, aplastic anemia), vitamin deficiencies (B12 or folate), or medications.
- Increased platelet destruction: This can be caused by autoimmune diseases (like immune thrombocytopenic purpura – ITP), certain infections, or medications.
- Platelet sequestration: Platelets can be trapped in the spleen, causing a falsely low count (seen in splenomegaly).
- Dilution: Large volumes of fluid can dilute the platelet count (e.g., in massive blood transfusions).
Identifying the underlying cause is crucial for effective treatment. For example, ITP might require corticosteroids or immunomodulatory therapy, while treating an infection or discontinuing a medication causing thrombocytopenia can resolve the problem.
Q 20. How do you interpret a complete blood count (CBC)?
A complete blood count (CBC) provides a comprehensive overview of blood components. Interpretation involves analyzing several key parameters:
- White Blood Cell (WBC) count: Indicates the overall number of white blood cells. An elevated count (leukocytosis) can suggest infection, inflammation, or leukemia; a low count (leukopenia) can indicate bone marrow suppression or infection.
- Red Blood Cell (RBC) count and Hemoglobin (Hgb): Reflect the oxygen-carrying capacity of the blood. Low values (anemia) suggest various underlying causes, including iron deficiency, blood loss, or bone marrow disorders.
- Platelet (Plt) count: Reflects the ability of blood to clot. Low counts (thrombocytopenia) increase bleeding risk.
- White blood cell differential: Shows the proportions of different types of white blood cells (neutrophils, lymphocytes, monocytes, eosinophils, basophils).
- Mean Corpuscular Volume (MCV): Indicates the average size of red blood cells, useful in classifying anemias.
A CBC is a fundamental test in hematology, providing important clues to diagnose and monitor various conditions. Deviations from normal ranges warrant further investigation.
Q 21. Explain the significance of different white blood cell differentials.
The white blood cell differential provides valuable insights into the body’s immune response. Each type of white blood cell has a specific function:
- Neutrophils: The most abundant type, crucial for fighting bacterial infections. Increased neutrophils (neutrophilia) can indicate infection or inflammation. Decreased neutrophils (neutropenia) increases susceptibility to infections.
- Lymphocytes: Involved in immune response to viruses and other pathogens. Increased lymphocytes (lymphocytosis) can suggest viral infections, leukemia, or other immune disorders. Decreased lymphocytes (lymphocytopenia) indicates impaired immune function.
- Monocytes: Phagocytic cells that engulf pathogens and cellular debris. Increased monocytes (monocytosis) is seen in certain infections and chronic inflammatory conditions.
- Eosinophils: Involved in allergic reactions and parasitic infections. Increased eosinophils (eosinophilia) often points towards allergic conditions, parasitic infections, or certain cancers.
- Basophils: Release histamine during allergic reactions. Increased basophils (basophilia) is less commonly seen but can be associated with allergic conditions or certain blood cancers.
Analyzing the differential helps clinicians determine the nature of an infection or inflammatory process and identify underlying hematological disorders.
Q 22. Describe the principle of flow cytometry in hematology.
Flow cytometry is a powerful technique used in hematology to analyze the physical and chemical characteristics of individual cells within a heterogeneous population. It works by suspending cells in a fluid and passing them through a laser beam, one at a time. As each cell passes, its properties are measured based on the light it scatters or emits. Forward scatter (FSC) measures cell size, while side scatter (SSC) measures cell granularity or internal complexity. Fluorescently labeled antibodies, specific for various cell surface markers (like CD markers on lymphocytes), are used to identify and quantify different cell types.
Imagine it like a high-speed cell sorting system. Each cell is interrogated, and based on its size, granularity, and expression of specific surface markers, it gets categorized. This allows hematologists to precisely identify and count different blood cell populations, such as lymphocytes, monocytes, and neutrophils, and analyze their maturity stages. This is crucial for diagnosing diseases like leukemia, lymphoma, and immunodeficiencies.
For example, in diagnosing acute lymphoblastic leukemia (ALL), flow cytometry can identify the presence of immature lymphoid blasts, characterizing their specific immunophenotype (surface markers), which helps guide treatment decisions. Flow cytometry provides a quantitative and qualitative analysis, offering much more detail than a simple blood count.
Q 23. What are the limitations of different coagulation tests?
Coagulation tests, while invaluable, have limitations. The results can be affected by various pre-analytical factors, such as the patient’s hydration status, medication use, and even the time elapsed between blood collection and analysis. For example, prolonged tourniquet application can lead to hemoconcentration and falsely elevated coagulation factors.
- Prothrombin Time (PT): Primarily assesses the extrinsic and common pathways of coagulation. It’s affected by factors II, V, VII, and X, and is highly sensitive to vitamin K deficiency. However, it lacks specificity, as multiple factor deficiencies can prolong the PT.
- Activated Partial Thromboplastin Time (aPTT): Assesses the intrinsic and common pathways. Its prolonged value can indicate several factor deficiencies (VIII, IX, XI, XII) or the presence of inhibitors. However, like the PT, it’s not highly specific.
- Thrombin Time (TT): Measures the conversion of fibrinogen to fibrin. It’s affected by fibrinogen levels and the presence of inhibitors of thrombin. However, it doesn’t provide information about the earlier steps in the coagulation cascade.
- D-dimer: A marker of fibrin degradation. While useful for ruling out deep vein thrombosis (DVT) when negative, a positive result isn’t always diagnostic, as it can be elevated in various conditions, including pregnancy and inflammation.
Furthermore, many coagulation tests are only snapshots in time and may not reflect the dynamic nature of the coagulation system. Individual variation also exists, making interpretation complex.
Q 24. How do you manage a patient with a bleeding disorder?
Managing a patient with a bleeding disorder requires a multi-faceted approach, starting with a thorough history and physical examination to understand the bleeding pattern and severity. A detailed family history is crucial, as many bleeding disorders are inherited. Laboratory investigations are essential, including a complete blood count (CBC), coagulation tests (PT, aPTT, TT), and often specialized assays to identify specific factor deficiencies, such as factor VIII or IX for hemophilia.
Management strategies vary widely depending on the specific disorder and its severity. They may include:
- Factor replacement therapy: For hemophilia A and B, this involves administering the missing clotting factor intravenously. This is the cornerstone of treatment for acute bleeds and before invasive procedures.
- Desmopressin (DDAVP): This medication stimulates the release of von Willebrand factor and factor VIII from endothelial cells. It’s beneficial for some patients with mild hemophilia A and von Willebrand disease.
- Antifibrinolytic agents: Such as tranexamic acid or aminocaproic acid, these agents help stabilize clots and reduce bleeding. They’re useful for managing menorrhagia in patients with von Willebrand disease or other bleeding disorders.
- Supportive care: This includes measures like avoiding contact sports, prompt treatment of injuries, and the use of prophylactic measures, like dental prophylaxis, to prevent bleeding episodes.
Regular monitoring of bleeding episodes and appropriate prophylactic measures are essential to improve the patient’s quality of life. Patient education and counseling are vital aspects of long-term management.
Q 25. How do you investigate a patient with unexplained anemia?
Investigating unexplained anemia requires a systematic approach. It begins with a thorough history (including dietary habits, medications, travel history, and family history), physical examination (looking for signs of bleeding, pallor, splenomegaly), and a complete blood count (CBC) with peripheral blood smear. The CBC provides critical information about red blood cell indices (MCV, MCH, MCHC), which helps classify the anemia as microcytic, normocytic, or macrocytic.
The next steps depend on the initial findings:
- Microcytic anemia: Suggests iron deficiency, thalassemia, or sideroblastic anemia. Further investigations may include iron studies (serum ferritin, iron, total iron-binding capacity), hemoglobin electrophoresis, and bone marrow examination.
- Normocytic anemia: Can be caused by chronic disease, hemolysis, or acute blood loss. Investigations might include reticulocyte count, lactate dehydrogenase (LDH), haptoglobin, Coombs test (to detect autoimmune hemolysis), and renal function tests.
- Macrocytic anemia: Usually suggests vitamin B12 or folate deficiency, or myelodysplastic syndromes. Investigations include vitamin B12 and folate levels, and sometimes bone marrow examination.
Once the type of anemia is identified, further investigations are tailored to establish the underlying cause. This might involve endoscopic procedures (to detect gastrointestinal bleeding) or genetic testing.
Imagine solving a detective case. The CBC provides clues, and further investigations pinpoint the culprit behind the anemia.
Q 26. Explain the use of anticoagulants in the management of thrombosis.
Anticoagulants are crucial in the management of thrombosis, which involves the formation of blood clots within blood vessels. They work by either inhibiting the formation of thrombin (the enzyme crucial for fibrin clot formation) or interfering with the coagulation cascade. The choice of anticoagulant depends on several factors, including the type of thrombosis (e.g., deep vein thrombosis, pulmonary embolism, atrial fibrillation), the patient’s comorbidities, and potential drug interactions.
Examples of anticoagulants include:
- Direct thrombin inhibitors (e.g., dabigatran, argatroban): These drugs directly inhibit thrombin, preventing fibrin formation. They are often preferred for patients with atrial fibrillation.
- Factor Xa inhibitors (e.g., rivaroxaban, apixaban): These drugs inhibit factor Xa, a crucial factor in the coagulation cascade. They are also widely used for prevention and treatment of venous thromboembolism (VTE).
- Vitamin K antagonists (e.g., warfarin): These drugs inhibit the synthesis of vitamin K-dependent clotting factors (II, VII, IX, X). They require regular monitoring of the International Normalized Ratio (INR) to ensure therapeutic efficacy and avoid bleeding complications.
- Heparin (unfractionated and low-molecular-weight): These are parenteral anticoagulants used for acute treatment of VTE and in various other settings.
Careful patient selection, monitoring of anticoagulation levels (when applicable), and close attention to potential side effects (especially bleeding) are crucial aspects of anticoagulant management. Therapeutic drug monitoring and regular assessment of the patient’s clinical condition are essential to optimize treatment and minimize risks.
Q 27. Discuss the principles of bone marrow aspiration and biopsy.
Bone marrow aspiration and biopsy are invasive procedures performed to obtain samples of bone marrow for diagnostic and therapeutic purposes. They provide essential information about the cellularity, morphology, and hematopoietic activity of the bone marrow.
Aspiration: A needle is inserted into the bone (usually the posterior iliac crest) to withdraw a sample of liquid bone marrow. This sample is then used for cytological examination, flow cytometry, and other tests to assess the number and characteristics of various blood cell precursors.
Biopsy: A small core of bone marrow tissue is removed using a special needle. The biopsy sample allows for histological examination, providing detailed information about the tissue architecture, fibrosis, and the distribution of different cell types. This is crucial for diagnosing disorders that affect the bone marrow structure, such as myelofibrosis.
The procedures are usually performed under local anesthesia, with the patient lying on their side. Possible complications include bleeding, infection, and pain at the puncture site. Before performing the procedures, informed consent is essential. Both aspiration and biopsy are complementary. Aspiration offers a cell count and morphology, while biopsy provides tissue architecture and assessment of extracellular matrix. The two provide a comprehensive assessment of the bone marrow.
Q 28. Describe your experience with quality control and quality assurance in a hematology laboratory.
Quality control (QC) and quality assurance (QA) are integral parts of a hematology laboratory. My experience involves implementing and maintaining a robust QC program that ensures the accuracy and reliability of laboratory results. This involves:
- Daily QC: Running control materials with each batch of patient samples to monitor the performance of instruments and assays. Any deviations from acceptable ranges trigger troubleshooting and corrective actions.
- Internal Quality Control (IQC) and External Quality Assessment (EQA): Participating in regular EQA programs to compare our results with those from other labs, identifying any systemic biases or errors and implementing corrective actions.
- Instrument maintenance: Regular calibration and preventative maintenance of all analytical instruments, ensuring their optimal performance and minimizing errors.
- Reagent management: Proper storage and handling of reagents, preventing degradation and ensuring optimal reagent performance.
- Staff training: Regular training for laboratory staff on proper techniques, safety procedures, and the interpretation of results.
- Documentation: Detailed documentation of all QC data, instrument maintenance, and training activities. This is crucial for traceability and compliance with accreditation standards.
In my experience, adherence to strict QC and QA practices is not just about ensuring the accuracy of results; it’s also about patient safety. A well-maintained QC program prevents misdiagnosis and guides appropriate treatment decisions.
For example, monitoring the precision and accuracy of CBC analyzers is paramount to detect and correct issues that could lead to erroneous diagnoses of anemia or leukocytosis. Likewise, ensuring the proper calibration of coagulation instruments is vital for appropriate management of patients on anticoagulants, preventing both thrombosis and bleeding complications.
Key Topics to Learn for Hematology and Coagulation Interview
- Red Blood Cell Disorders: Understand the pathophysiology, diagnosis, and management of anemias (e.g., iron deficiency, megaloblastic, hemolytic), polycythemia vera, and other red cell abnormalities. Consider practical applications like interpreting CBC results and correlating them with clinical presentations.
- White Blood Cell Disorders: Master the characteristics and clinical significance of leukemias (acute and chronic myeloid and lymphoid), lymphomas (Hodgkin and non-Hodgkin), and myeloproliferative neoplasms. Focus on differential diagnosis and treatment approaches.
- Platelet Disorders: Gain a strong understanding of thrombocytopenia, thrombocytosis, and inherited platelet disorders. Practice applying your knowledge to case studies involving bleeding and thrombotic events.
- Hemostasis and Coagulation: Thoroughly review the coagulation cascade, intrinsic and extrinsic pathways, common coagulation factor deficiencies (hemophilia A and B, von Willebrand disease), and the interpretation of coagulation tests (PT, aPTT, INR). Develop problem-solving skills in identifying bleeding disorders.
- Bone Marrow Disorders: Explore the various bone marrow disorders, their diagnostic approaches (bone marrow biopsy and aspiration), and treatment strategies. Understand the significance of cytogenetic and molecular analyses.
- Transfusion Medicine: Familiarize yourself with blood group systems, transfusion reactions, and the indications for blood component therapy. Be prepared to discuss the management of transfusion-related complications.
- Laboratory Techniques: Review common hematology and coagulation laboratory techniques, including cell counts, peripheral blood smears, and coagulation assays. Understand the limitations and interpretations of these tests.
- Treatment Modalities: Be prepared to discuss various treatment options for hematologic and coagulation disorders, including chemotherapy, targeted therapy, stem cell transplantation, and supportive care.
Next Steps
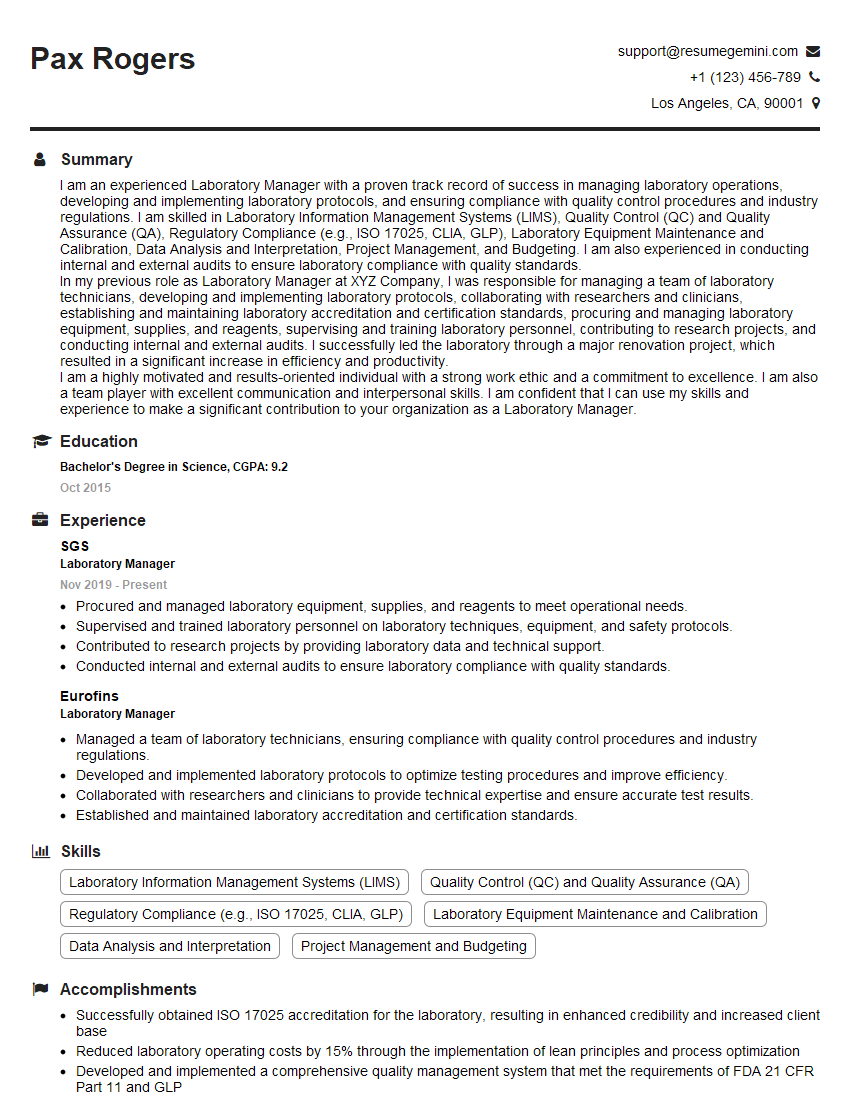
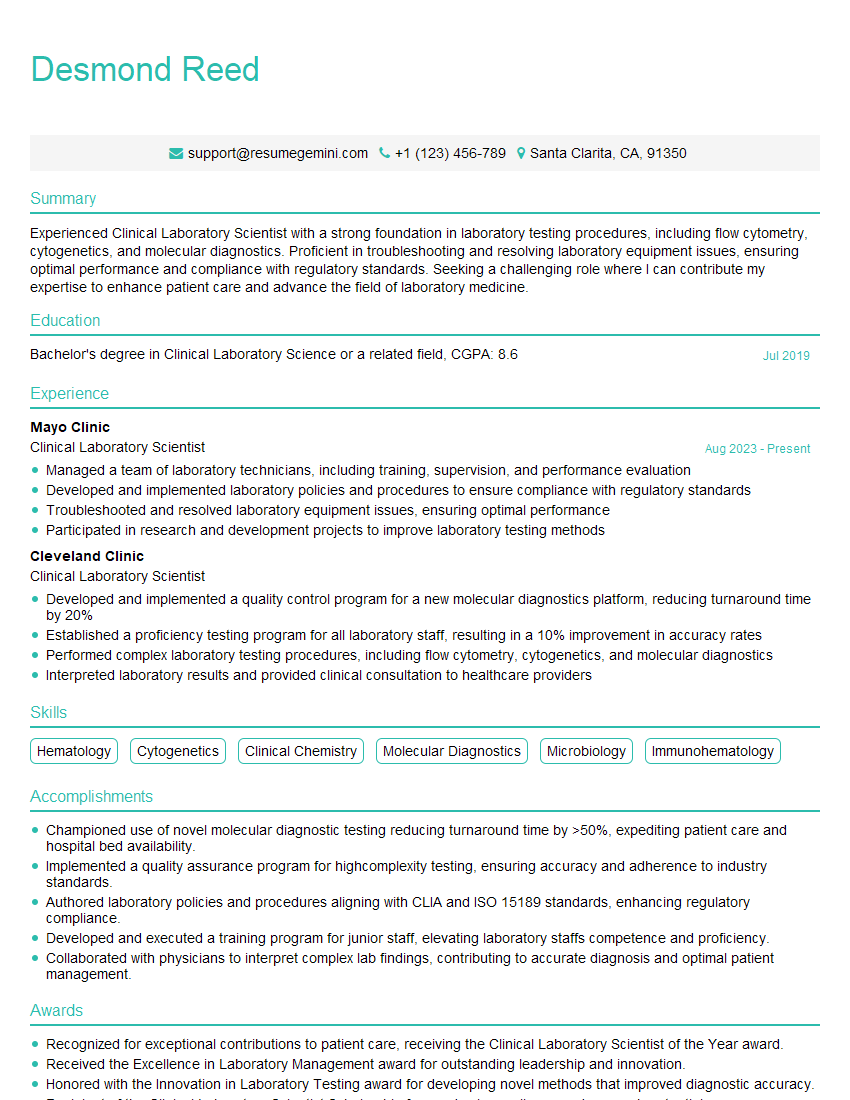
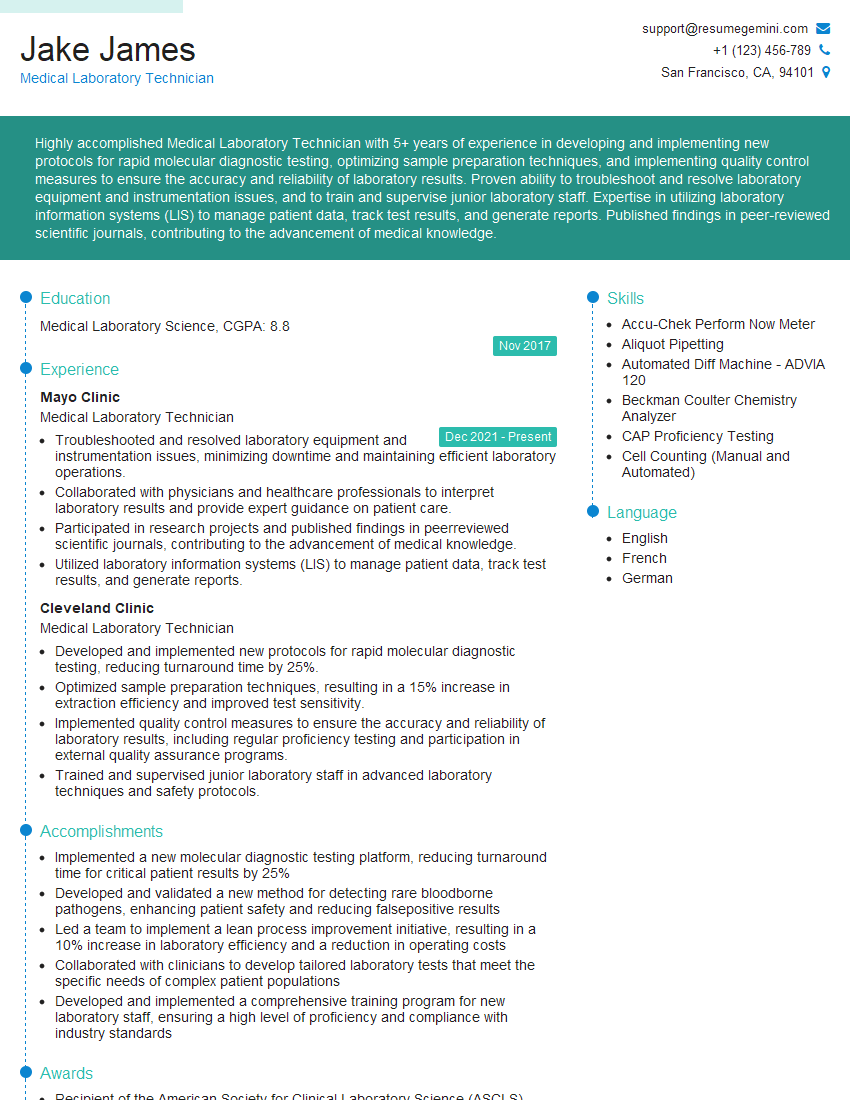
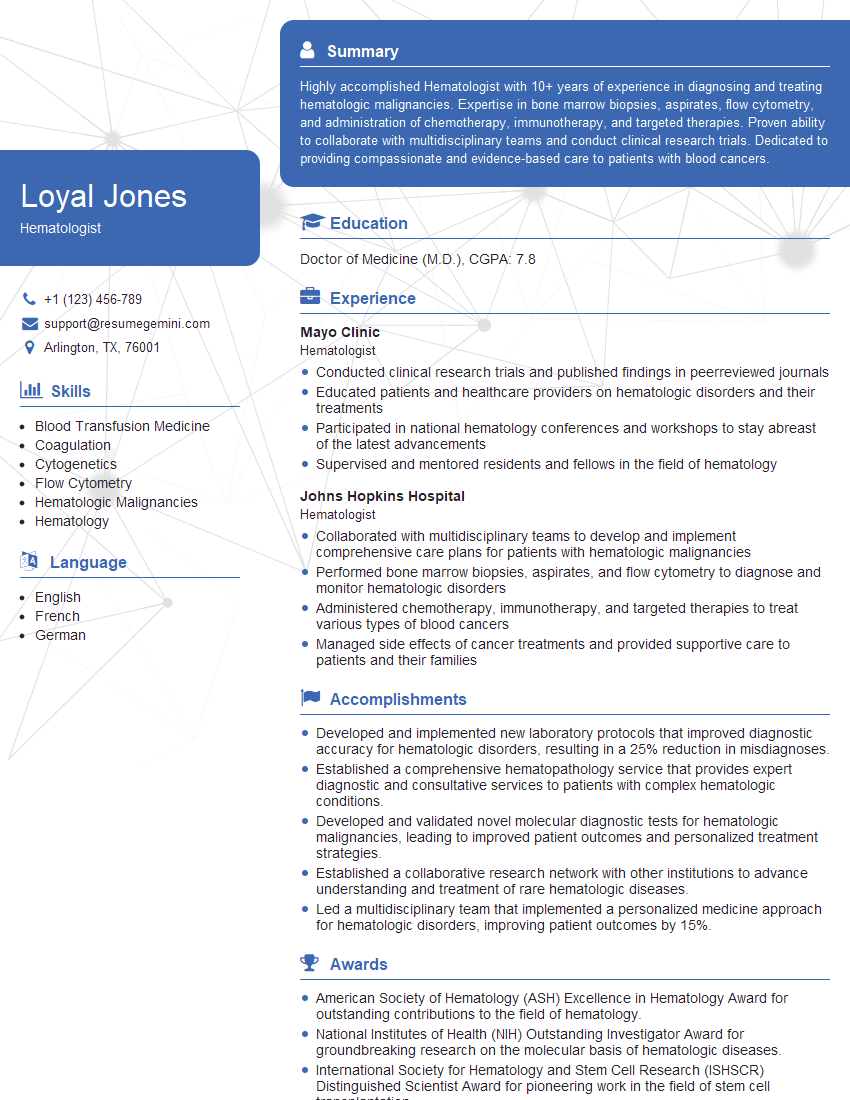
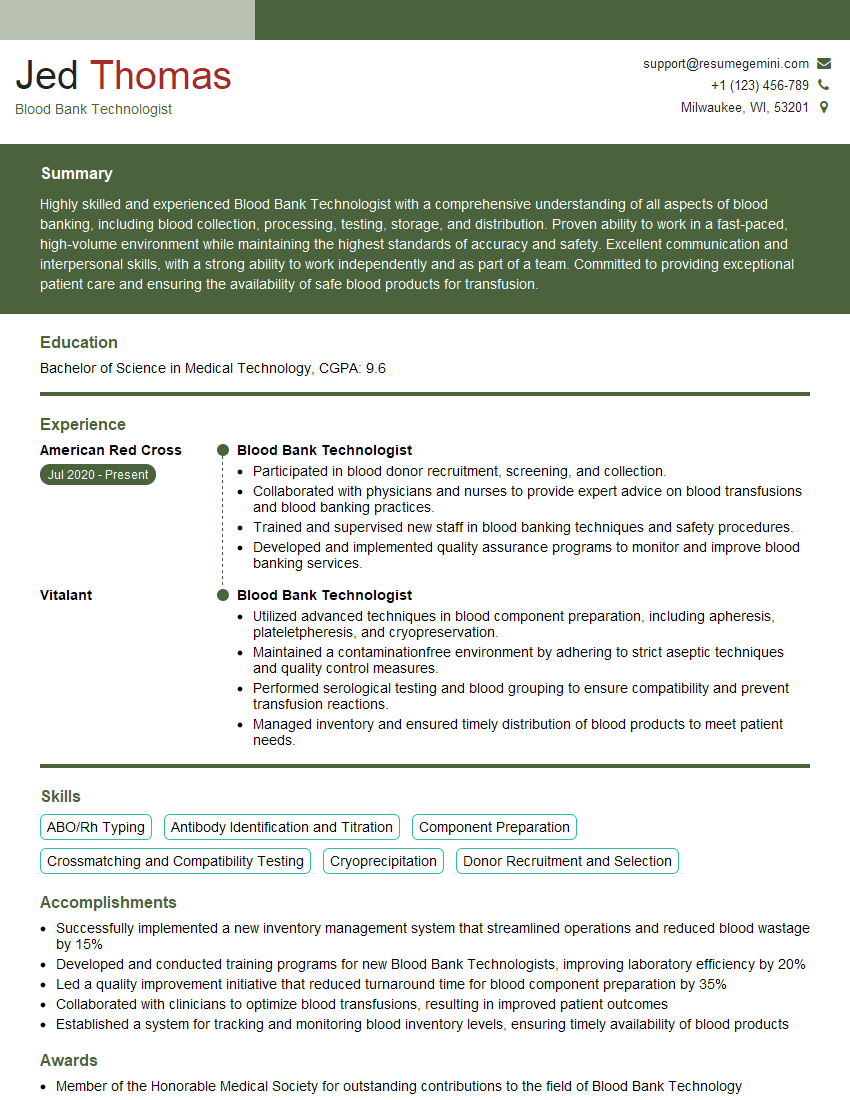
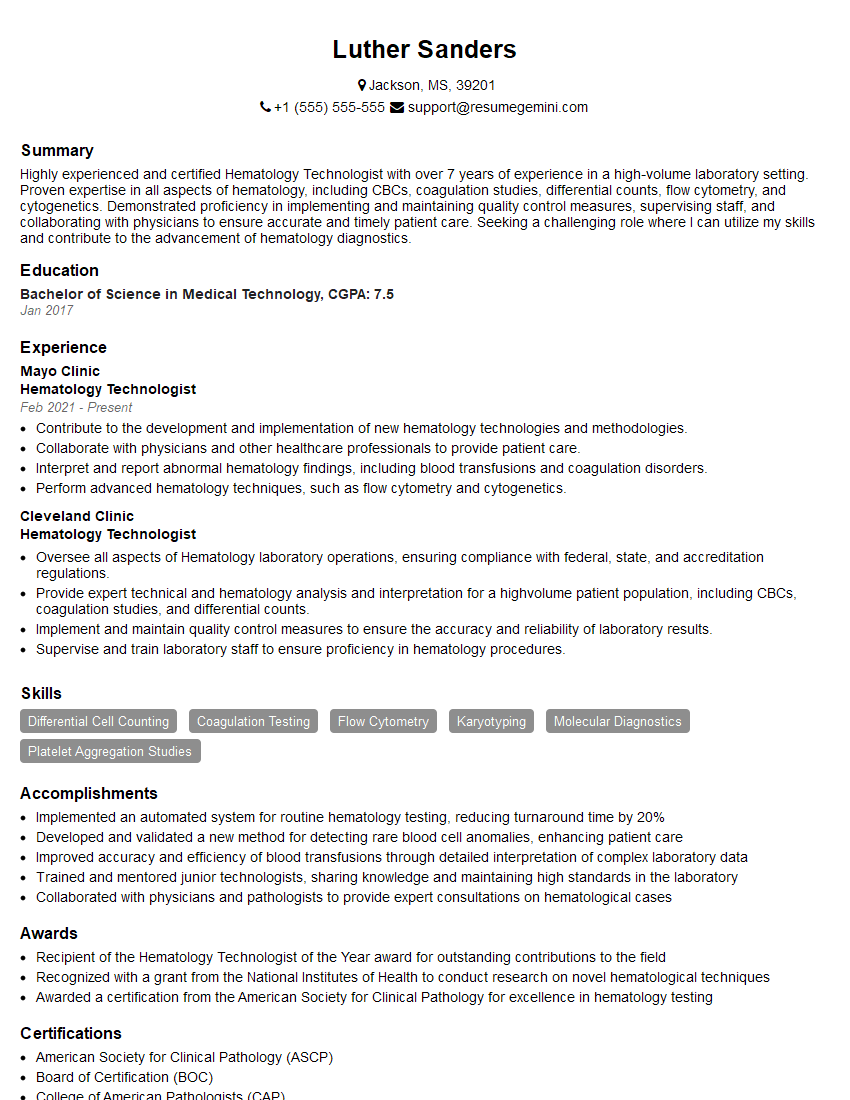
Mastering Hematology and Coagulation is crucial for career advancement in this specialized field, opening doors to exciting opportunities in research, clinical practice, and industry. To significantly enhance your job prospects, crafting an ATS-friendly resume is essential. ResumeGemini is a trusted resource to help you build a professional and impactful resume that highlights your skills and experience effectively. We provide examples of resumes tailored specifically to Hematology and Coagulation to guide you in creating a compelling application.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Interesting Article, I liked the depth of knowledge you’ve shared.
Helpful, thanks for sharing.
Hi, I represent a social media marketing agency and liked your blog
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?