Unlock your full potential by mastering the most common Healthcare Risk Management interview questions. This blog offers a deep dive into the critical topics, ensuring you’re not only prepared to answer but to excel. With these insights, you’ll approach your interview with clarity and confidence.
Questions Asked in Healthcare Risk Management Interview
Q 1. Describe your experience with implementing a risk management program.
Implementing a risk management program requires a systematic approach. It begins with securing executive sponsorship and buy-in, demonstrating the program’s value in terms of improved patient safety, regulatory compliance, and cost savings. I’ve led several implementations, each following a similar phased approach: First, we conduct a comprehensive risk assessment, using a combination of interviews, surveys, and data analysis to identify potential hazards. This is followed by developing a risk register, prioritizing risks based on likelihood and severity. Next, we create tailored mitigation strategies, assigning responsibilities and setting timelines. We then establish a robust monitoring and reporting system to track progress and ensure ongoing effectiveness. Finally, continuous improvement is paramount; regular reviews and updates to the risk register ensure the program remains relevant and responsive to changing circumstances. For example, in a previous role at a large hospital system, we implemented a program that reduced medication errors by 25% within the first year through improved medication reconciliation processes and enhanced staff training.
A key aspect is establishing a culture of safety. This involves open communication, encouragement of incident reporting, and a ‘just culture’ where individuals are not punished for reporting errors, but instead, the focus is on learning from mistakes to prevent future occurrences. Successful implementation requires strong leadership, effective communication, and continuous engagement from all levels of the organization.
Q 2. How do you identify and assess potential risks in a healthcare setting?
Identifying and assessing risks in healthcare requires a multi-faceted approach. We utilize several methods, including:
- Proactive Risk Assessments: These involve systematically reviewing processes and procedures to identify potential hazards. For example, we might review medication administration protocols, surgical checklists, or infection control procedures.
- Incident Reporting and Analysis: Analyzing past incidents, near misses, and adverse events provides valuable insights into areas needing improvement. This forms the basis of our reactive risk management.
- Regulatory Compliance Reviews: Staying updated on and adhering to regulations like HIPAA and Joint Commission standards is critical for identifying potential risks.
- Vulnerability Assessments: This is particularly relevant for IT systems and data security. We conduct regular assessments to identify weaknesses and implement appropriate safeguards.
- Stakeholder Engagement: We actively engage with staff at all levels, patients, families, and external stakeholders to gain different perspectives and uncover potential risks that might otherwise be overlooked. This often involves surveys, interviews, and focus groups.
Once potential risks are identified, we assess them using qualitative and quantitative methods, considering factors such as the likelihood of occurrence and the potential severity of the consequences. A risk matrix helps visualize this, allowing for prioritization of resources.
Q 3. What methods do you use to prioritize risks and allocate resources?
Prioritizing risks and allocating resources requires a structured approach. We typically use a risk matrix that plots risks based on their likelihood and impact. This enables us to focus on the highest-priority risks, those with both high likelihood and high impact. For example, a risk with a high likelihood of occurrence and a potentially catastrophic impact (e.g., a widespread system failure) will receive top priority.
Resource allocation is then guided by this prioritization. We may allocate more resources (personnel, funding, time) to mitigating high-priority risks. This includes developing detailed mitigation plans with clear timelines and assigned responsibilities. We also consider the cost-benefit analysis of different interventions. A less expensive but highly effective strategy is prioritized over a more expensive intervention of lesser impact. Regular review and adjustments of this process are crucial as risks evolve over time.
Q 4. Explain your experience with root cause analysis (RCA) and corrective action plans.
Root Cause Analysis (RCA) is a systematic approach to investigating adverse events and near misses to determine the underlying causes. I have extensive experience conducting RCAs, typically using a structured methodology like the ‘5 Whys’ technique or a fishbone diagram. The goal isn’t to assign blame but to identify systemic issues that contributed to the event. For example, a patient fall may initially seem like an isolated incident. However, an RCA might reveal inadequate staffing levels, lack of fall prevention protocols, or deficiencies in patient assessment as underlying causes.
Corrective action plans (CAPs) are developed based on the findings of the RCA. These plans outline specific actions to prevent similar events from recurring. We ensure that CAPs are measurable, achievable, relevant, and time-bound (SMART). Implementation is closely monitored, and effectiveness is evaluated through follow-up audits and ongoing data analysis. For instance, following a medication error, a CAP might involve implementing a double-check system, improving medication labeling, or providing additional staff training.
Q 5. How do you monitor and evaluate the effectiveness of risk management strategies?
Monitoring and evaluating the effectiveness of risk management strategies is an ongoing process. Key metrics include the number and types of incidents reported, the effectiveness of mitigation strategies, and the overall reduction in risk exposure. We regularly review key performance indicators (KPIs) such as the frequency of medication errors, infection rates, patient falls, and adverse events. Data from these indicators is compared against benchmarks and targets, allowing us to track progress and identify areas needing improvement.
Regular audits, both internal and external, are also crucial. These audits assess the adequacy of our risk management program, ensuring compliance with relevant regulations and standards. The findings from these audits are used to inform program updates and refine our strategies. This ensures our risk management program is continuously evolving and improving in line with best practices and changing circumstances.
Q 6. Describe your experience with HIPAA compliance and patient privacy.
HIPAA compliance and patient privacy are paramount in healthcare. My experience encompasses developing and implementing policies and procedures to ensure compliance with all relevant HIPAA regulations. This includes training staff on HIPAA regulations, implementing robust security measures to protect electronic health information (EHI), and developing protocols for handling patient data securely. We conduct regular security risk assessments, particularly focusing on vulnerabilities within IT systems and data storage.
We also establish clear procedures for accessing and disclosing patient information, ensuring that only authorized personnel have access. We routinely audit access logs to identify any unauthorized access attempts. Our breach response plan outlines procedures to be followed in the event of a data breach. In addition to HIPAA compliance, we also ensure adherence to state and local regulations related to patient privacy.
Q 7. How do you manage incidents and adverse events to mitigate future risks?
Managing incidents and adverse events is crucial for mitigating future risks. Our approach involves a structured process:
- Immediate Response: Providing immediate care to the affected individual and containing the situation are top priorities.
- Investigation: A thorough investigation is undertaken to determine the facts surrounding the event, using tools like RCA to identify root causes.
- Corrective Actions: Based on the RCA, we develop and implement CAPs to prevent recurrence.
- Reporting: We report incidents to relevant authorities as required (e.g., The Joint Commission, state health departments).
- Communication: Open and honest communication with patients, families, and staff is essential.
- Learning and Improvement: We use the experience to improve our processes, policies, and training programs.
For example, after a medication error, we might conduct an RCA, resulting in implementing a new medication administration protocol, enhanced staff training, and improved medication labeling. This systematic approach ensures that lessons learned from incidents contribute directly to improved patient safety and risk mitigation.
Q 8. What are your strategies for communicating risk information to stakeholders?
Effective risk communication is crucial in healthcare. My strategy involves tailoring the message to the audience’s understanding and needs. For example, communicating a potential medication error risk to physicians requires a different approach than explaining the same risk to patients or administrative staff.
- For Physicians and Clinical Staff: I utilize concise, evidence-based reports, focusing on the impact on patient safety and potential liability. I might present data on near misses or adverse events to highlight the seriousness and potential for future occurrences.
- For Patients and Families: I use clear, simple language avoiding medical jargon, focusing on the potential impact on their health and well-being. I’d emphasize steps taken to mitigate the risk and encourage open communication.
- For Administrative Staff: I provide data-driven reports on risk trends, financial implications, and regulatory compliance needs. This includes risk assessments, cost-benefit analyses, and resource allocation proposals.
- For Board Members: I use high-level summaries highlighting key risks, their potential impact on the organization’s strategic goals, and the effectiveness of mitigation strategies. This often includes visual aids and presentations emphasizing the financial and reputational aspects.
Regardless of the audience, open communication channels, feedback mechanisms, and transparency are essential to building trust and fostering a culture of safety.
Q 9. How do you ensure effective risk management training for healthcare staff?
Effective risk management training is multifaceted. It needs to be engaging, relevant, and regularly updated to reflect best practices and emerging threats. My approach involves a blended learning strategy combining online modules, interactive workshops, and on-the-job training.
- Needs Assessment: I start by identifying knowledge gaps and training needs through surveys, interviews, and analysis of incident reports. This ensures the training addresses specific challenges within the organization.
- Modular Training: Online modules provide flexibility and allow staff to learn at their own pace. These modules cover topics like incident reporting, root cause analysis, and specific risks relevant to their roles (e.g., infection control for nurses, medication safety for pharmacists).
- Interactive Workshops: Hands-on workshops allow for scenario-based training and group discussions. This fosters collaborative problem-solving and improves understanding of complex risk management concepts.
- On-the-Job Training and Mentoring: Experienced staff mentor new employees and provide ongoing support and guidance. Regular feedback sessions ensure continuous improvement and identify any challenges.
- Regular Updates: Training is regularly updated to reflect changes in regulations, best practices, and the organization’s risk profile.
Post-training assessments and evaluations ensure that the learning objectives are met and that the training is effective. I also track incident rates to measure the impact of the training on actual risk reduction.
Q 10. Describe your experience with risk mitigation strategies in various healthcare settings.
My experience encompasses diverse healthcare settings, including hospitals, clinics, and long-term care facilities. Risk mitigation strategies vary depending on the specific environment and identified risks.
- Hospitals: I’ve implemented strategies to reduce medication errors (e.g., barcoding medication, implementing automated dispensing cabinets), improve infection control (e.g., hand hygiene programs, enhanced cleaning protocols), and prevent falls (e.g., fall risk assessments, environmental modifications).
- Clinics: In smaller clinic settings, I’ve focused on streamlined workflows to reduce administrative errors, implemented robust patient identification procedures, and provided training on appropriate use of medical devices.
- Long-Term Care Facilities: Here, strategies have centered around preventing pressure ulcers (e.g., repositioning schedules, specialized mattresses), managing resident falls, and ensuring appropriate medication administration for cognitively impaired residents.
In all settings, a crucial aspect of my work involves a collaborative approach. Engaging front-line staff in the identification of hazards and the development of solutions is key to successful risk mitigation. A strong safety culture is created through open communication, staff empowerment, and proactive risk identification.
Q 11. How do you develop and maintain effective risk management policies and procedures?
Developing and maintaining effective policies and procedures requires a systematic approach, involving regular review and updates.
- Risk Assessment: A thorough assessment identifies potential hazards and vulnerabilities. This can involve surveys, incident reviews, and benchmarking against industry standards.
- Policy Development: Based on the risk assessment, clear, concise, and easy-to-understand policies and procedures are developed. They should be accessible to all staff and regularly reviewed for clarity and effectiveness.
- Implementation and Training: Policies and procedures are rolled out through comprehensive training programs and clear communication channels. This ensures that staff understand their responsibilities and can implement the procedures effectively.
- Monitoring and Evaluation: Regular monitoring and evaluation are crucial to identify areas for improvement. This may include auditing compliance, tracking incident reports, and reviewing feedback from staff.
- Revision and Updates: Policies and procedures should be reviewed and updated regularly to reflect changes in regulations, best practices, and the organization’s risk profile. This ensures continued relevance and effectiveness.
Using a well-defined policy and procedure development framework allows for consistent, auditable, and effective risk management throughout the organization. I leverage tools like workflow diagrams and decision trees to help staff understand complex procedures clearly.
Q 12. Explain your understanding of Joint Commission standards and accreditation.
The Joint Commission (TJC) sets the gold standard for healthcare accreditation in the United States. Their standards are designed to improve patient safety and quality of care. My understanding encompasses their focus on various aspects of risk management.
- National Patient Safety Goals (NPSGs): I’m intimately familiar with the NPSGs and how they translate into practical measures in a healthcare setting. For example, the NPSG on medication safety guides the development of policies and procedures related to medication reconciliation, safe medication administration, and preventing medication errors.
- Performance Measurement: TJC accreditation demands ongoing performance measurement to demonstrate compliance with standards. This includes regular auditing, data analysis, and identifying opportunities for improvement.
- Root Cause Analysis (RCA): When adverse events occur, conducting a thorough RCA according to TJC guidelines is essential. This identifies the underlying causes of the event and enables the implementation of corrective actions to prevent recurrence.
- Sentinel Events: I understand the significance of sentinel events (unexpected occurrences involving death or serious physical or psychological injury) and the rigorous reporting and investigation processes required by TJC.
Maintaining TJC accreditation is a continuous process requiring ongoing attention to detail, commitment to quality improvement, and a deep understanding of their standards. The accreditation process strengthens an organization’s commitment to patient safety and provides external validation of its safety efforts.
Q 13. What experience do you have with claims management and litigation prevention?
Experience in claims management and litigation prevention is a critical component of healthcare risk management. Proactive measures can significantly reduce liability.
- Claims Management: This involves coordinating with legal counsel, insurance providers, and relevant departments within the healthcare organization to manage claims efficiently and effectively. It includes gathering medical records, preparing documentation, and working with adjusters to achieve fair settlements.
- Litigation Prevention: This proactive approach uses various strategies to minimize the likelihood of lawsuits.
- Effective Communication: Clear and consistent communication with patients and their families is crucial in preventing misunderstandings and potential disputes.
- Thorough Documentation: Comprehensive and accurate medical records can significantly reduce the risk of litigation.
- Incident Reporting and Analysis: A robust system for reporting and analyzing incidents allows for early identification of potential problems and the development of preventive measures.
- Risk Assessment: Regular risk assessments identify potential areas of vulnerability that can lead to litigation.
Understanding legal implications and maintaining strong documentation practices are essential to minimizing the risk of lawsuits and reducing the financial and reputational impact on the organization.
Q 14. How do you utilize data analytics to inform risk management decisions?
Data analytics plays a vital role in informing risk management decisions, moving beyond reactive approaches to proactive and predictive ones.
- Incident Reporting Databases: Analyzing incident reports using data analytics identifies patterns and trends. For example, we can identify high-risk areas, such as particular units with increased medication errors or falls, and target interventions accordingly.
- Patient Data: Analyzing patient data can reveal risk factors associated with adverse events. This allows us to proactively implement risk mitigation strategies for high-risk patients.
- Financial Data: Analyzing claims data helps to identify areas with high claim frequency or costs, allowing for focused efforts on risk mitigation and cost reduction.
- Predictive Modeling: Advanced analytics can be used to develop predictive models for identifying patients at high risk for specific adverse events (e.g., sepsis, pressure ulcers). This allows for timely intervention and prevention.
Data visualization tools are essential for communicating insights to stakeholders, making complex data easily understandable and fostering data-driven decision-making. This empowers proactive risk mitigation and continuous improvement.
Q 15. Describe a situation where you identified a significant risk and your actions to mitigate it.
In my previous role at a large hospital system, we noticed a concerning trend: a significant increase in medication errors related to look-alike/sound-alike (LASA) drugs. This wasn’t just a minor issue; it presented a direct threat to patient safety and could lead to serious adverse events, even death. This was a significant risk that required immediate attention.
My actions involved a multi-pronged approach. First, I initiated a thorough root cause analysis (RCA) to understand the underlying factors contributing to the errors. This involved interviewing staff, reviewing incident reports, and analyzing medication administration processes. The RCA revealed several key issues: insufficient staff training on LASA drug identification, inconsistent labeling practices, and a lack of robust double-checking procedures.
Next, I developed and implemented a comprehensive mitigation plan. This included:
- Mandating a hospital-wide, intensive training program for all clinical staff on LASA drug recognition and safe medication administration practices.
- Implementing a standardized medication labeling system using barcodes and electronic medication administration records (eMAR) to minimize errors related to incorrect drug selection and administration.
- Introducing a mandatory ‘double-check’ system involving two nurses verifying medication orders before administration, especially for high-risk drugs.
- Implementing technology-based solutions, such as automated dispensing cabinets with built-in safeguards to reduce medication errors.
Finally, I established ongoing monitoring and evaluation systems to track the effectiveness of the mitigation strategies. This included regular data analysis, staff feedback sessions, and periodic audits of medication administration practices. The implemented changes resulted in a 70% reduction in LASA-related medication errors within six months, showcasing the effectiveness of a proactive and data-driven approach to risk mitigation.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How familiar are you with different risk assessment methodologies?
I’m very familiar with a variety of risk assessment methodologies, and my selection depends greatly on the context of the risk. I commonly employ methods such as Failure Mode and Effects Analysis (FMEA), Fault Tree Analysis (FTA), and Hazard and Operability studies (HAZOP).
FMEA is excellent for systematically identifying potential failures in a process and assessing their severity, probability, and detectability. Imagine assessing the risk of a surgical procedure: FMEA would help us analyze each step, from pre-operative check-in to post-operative recovery, for potential problems and their consequences.
FTA, on the other hand, works backward from an undesired event to determine the root causes. For instance, if a patient falls and sustains an injury, an FTA would help us investigate what series of events led to that outcome.
HAZOP is especially valuable for complex systems. It uses guided questioning techniques to identify potential hazards and operability issues within a process. This approach is well-suited for evaluating the safety of a new medical device or the potential risks in a newly designed hospital workflow.
Beyond these, I also have experience with qualitative risk assessments, which are often used for prioritizing risks based on expert opinions, and quantitative risk assessments, which use statistical methods to estimate the likelihood and impact of potential risks. The choice depends entirely on the nature of the risk, the available data, and the resources available.
Q 17. What are your strategies for managing risks related to medical errors and patient safety?
Managing risks related to medical errors and patient safety requires a multifaceted strategy centered around prevention, detection, and response. My strategies focus on enhancing safety culture, improving processes, and leveraging technology.
- Strengthening Safety Culture: Fostering a blame-free environment where staff feel comfortable reporting errors without fear of retribution is crucial. This involves promoting open communication, providing regular safety training, and actively engaging staff in the development and implementation of safety initiatives. Think of this as building a team spirit where everyone is dedicated to safety.
- Process Improvement: Streamlining workflows, standardizing procedures, and using checklists can significantly reduce errors. For example, implementing a standardized surgical checklist can help ensure that crucial steps aren’t missed.
- Technology Integration: Implementing electronic health records (EHRs) with built-in safety features, such as medication alerts and clinical decision support systems, can dramatically improve accuracy and reduce the risk of medication errors. Using barcodes and RFID tags in the medication dispensing and administration process is also an effective method.
- Proactive Risk Identification: Regularly reviewing incident reports, conducting root cause analyses (RCA) for errors, and implementing corrective actions based on findings are essential aspects of proactive risk management. It’s about learning from mistakes and preventing future incidents.
- Patient Engagement: Empowering patients to actively participate in their care by providing clear instructions and opportunities to ask questions can help prevent errors.
A key component of this is continuous monitoring and improvement. Regularly reviewing data, gathering feedback, and adapting our strategies to account for emerging challenges is essential.
Q 18. How do you handle conflicting priorities or limited resources in risk management?
Conflicting priorities and limited resources are common challenges in healthcare risk management. My approach involves prioritization using a structured framework.
First, I’d conduct a thorough risk assessment to identify all potential risks. Then, I’d prioritize these risks using a matrix based on likelihood and impact. Risks with a high likelihood and high impact would be addressed first, even if it means temporarily delaying less critical projects.
Next, I’d explore creative solutions to manage resources effectively. This might involve partnering with other departments, negotiating for additional resources, or leveraging technology to automate processes. For instance, instead of hiring additional staff, we might invest in an automated system for a task to reduce human error.
Open and transparent communication with all stakeholders is vital in navigating these challenges. This includes clearly explaining the rationale behind decisions and involving stakeholders in the process of resource allocation and prioritization. Building consensus and finding compromises is key to effective resource management in a constrained environment.
Q 19. How do you build and maintain relationships with key stakeholders in risk management?
Building and maintaining strong relationships with key stakeholders is fundamental to effective risk management. My approach relies on open communication, active listening, and collaboration.
I begin by identifying all relevant stakeholders, including clinicians, administrators, patients, and external regulatory bodies. I then establish regular communication channels, such as meetings, email updates, and formal reports, to keep everyone informed about risk management activities.
Active listening and empathy are crucial in understanding the perspectives and concerns of different stakeholders. This helps build trust and facilitates collaborative problem-solving. I make a point of involving stakeholders in the decision-making process, seeking their input and incorporating their feedback into risk mitigation strategies.
For example, I might hold regular meetings with the nursing staff to understand their challenges and incorporate their suggestions into our safety protocols. Transparency in reporting risk assessment findings and mitigation strategies is vital to gain their trust and confidence.
Q 20. Describe your experience with regulatory compliance and reporting requirements.
I have extensive experience with regulatory compliance and reporting requirements, including HIPAA, OSHA, and Joint Commission standards. My approach is proactive and systematic.
I stay current with all relevant regulations and guidelines, and I ensure that our risk management processes align with those requirements. This includes regularly reviewing policies and procedures, providing training to staff on compliance matters, and conducting audits to monitor adherence to regulations.
When incidents occur, I manage the reporting process meticulously, ensuring accurate and timely submission of all required documentation to the appropriate agencies. This includes documenting all steps taken to investigate the incident, determine root causes, and implement corrective actions. Maintaining comprehensive documentation is crucial not only for regulatory compliance but also for learning and improvement.
I approach regulatory compliance as an integral part of our risk management program, not just as a set of obligations. By proactively addressing compliance issues, we can minimize our risk of penalties and ensure that our operations are conducted safely and ethically.
Q 21. How do you leverage technology to improve the efficiency of risk management processes?
Technology plays a crucial role in enhancing the efficiency and effectiveness of risk management. I leverage various technological tools to improve data collection, analysis, and communication.
- Electronic Health Records (EHRs): EHRs are a fundamental resource, providing valuable data for identifying trends, patterns, and potential risks. Analyzing data from EHRs can help us identify areas prone to errors, such as medication administration or patient falls.
- Risk Management Software: Specialized software can streamline the risk assessment process, facilitating the identification, analysis, and tracking of risks. These platforms often include features for creating and managing risk registers, conducting root cause analyses, and monitoring corrective actions.
- Data Analytics and Reporting Tools: Data analytics can provide insights into the effectiveness of risk mitigation strategies. By analyzing trends and patterns in incident reports, we can identify areas requiring improvement and measure the impact of our interventions.
- Communication and Collaboration Platforms: Secure messaging and collaboration tools facilitate efficient communication among healthcare professionals and improve the timely sharing of important risk-related information.
By integrating these technologies effectively, we can automate many aspects of risk management, improving efficiency, reducing manual effort, and facilitating a more data-driven approach to risk mitigation.
Q 22. What are your strategies for promoting a culture of safety within a healthcare organization?
Promoting a culture of safety in healthcare requires a multi-faceted approach, moving beyond simple compliance to genuine organizational commitment. It’s about fostering an environment where reporting errors isn’t punished but seen as an opportunity for learning and improvement.
- Open Communication: Establishing transparent communication channels is paramount. This includes regular safety huddles, staff meetings dedicated to safety concerns, and readily available reporting systems for near misses and adverse events. For example, we implemented a ‘Just Culture’ program where staff felt safe reporting errors without fear of retribution, leading to a significant increase in incident reporting and a subsequent decrease in actual errors.
- Leadership Engagement: Visible and active leadership support is crucial. Leaders must champion safety initiatives, participate in safety rounds, and consistently reinforce the importance of safety in all organizational decisions. I’ve seen firsthand how a CEO’s personal commitment to safety can cascade down, influencing the behavior and attitudes of every employee.
- Education and Training: Ongoing education and training programs on risk management, incident reporting, and best practices are essential. This should encompass all levels of staff, from clinicians to administrative personnel. We incorporated simulation-based training to help staff practice their responses to high-risk situations, resulting in improved teamwork and quicker reaction times in real emergencies.
- Continuous Improvement: A robust system for analyzing incident reports, identifying root causes, and implementing corrective actions is critical. This often involves using root cause analysis (RCA) and Failure Mode and Effects Analysis (FMEA) techniques. We regularly review our safety data, identify trends, and proactively implement changes to prevent future incidents. For example, a recurring issue with medication errors led us to implement barcode medication administration, significantly reducing errors.
Q 23. Describe your experience with incident reporting and investigation.
My experience with incident reporting and investigation is extensive. I’ve managed systems for reporting, tracking, and analyzing various adverse events, near misses, and safety concerns. The process begins with a thorough and timely investigation of each incident. This typically involves collecting data from multiple sources including medical records, interview with involved staff, and review of relevant policies and procedures.
I utilize structured methods like root cause analysis (RCA) to identify the underlying causes of incidents rather than just focusing on the immediate events. RCA helps to identify systemic failures and implement changes that prevent recurrence. For example, in one case, RCA revealed a flaw in our medication dispensing process, leading to a complete overhaul of the system and a significant reduction in medication errors. We also use tools like the Five Whys to delve deeper into the causal chain of events. Finally, all investigations culminate in a detailed report that outlines findings, recommendations, and implemented corrective actions.
Q 24. How familiar are you with different insurance coverage options for healthcare risks?
I am very familiar with various insurance coverage options for healthcare risks, ranging from general liability and professional liability (malpractice) insurance to more specialized coverages like cyber liability and directors and officers (D&O) insurance. Understanding the nuances of each policy is crucial for effective risk management.
- General Liability: Protects against claims of bodily injury or property damage on healthcare premises.
- Professional Liability (Malpractice): Covers claims of negligence or misconduct by healthcare providers.
- Cyber Liability: Addresses risks associated with data breaches and cyberattacks.
- Workers’ Compensation: Covers medical expenses and lost wages for employees injured on the job.
- Excess/Umbrella Liability: Provides additional coverage beyond primary policies.
The selection of appropriate coverage depends on the specific risks faced by the organization, its size, and its financial capacity. It’s essential to work with experienced insurance brokers to assess needs and secure comprehensive coverage.
Q 25. How do you measure the return on investment (ROI) of risk management initiatives?
Measuring the ROI of risk management initiatives can be challenging, as the benefits are often difficult to quantify directly. However, a comprehensive approach involves considering both direct and indirect costs and benefits.
- Direct Costs: Include the cost of implementing risk management programs, such as training, software, and consultant fees.
- Direct Benefits: Include reductions in medical malpractice claims, decreased incident rates, improved patient safety, and avoidance of regulatory penalties. These can often be quantified through data analysis of incident rates before and after the implementation of risk mitigation strategies.
- Indirect Costs: Include the cost of lost productivity due to incidents, reputational damage, and decreased patient satisfaction.
- Indirect Benefits: Include improved patient outcomes, increased staff morale, enhanced organizational reputation, and a stronger culture of safety. These are often harder to quantify but are critical to overall organizational success.
A successful ROI analysis requires a holistic perspective, incorporating both qualitative and quantitative data. We often use a combination of metrics including incident rates, claims costs, patient satisfaction scores, and staff survey data to assess the overall impact of our risk management initiatives.
Q 26. How do you stay current with changes in healthcare regulations and best practices?
Staying current with healthcare regulations and best practices requires a proactive and multifaceted approach.
- Professional Organizations: Active membership in relevant professional organizations such as the American Society for Healthcare Risk Management (ASHRM) provides access to publications, conferences, and networking opportunities to stay abreast of the latest developments.
- Regulatory Agencies: Closely monitoring updates from regulatory bodies like the Centers for Medicare & Medicaid Services (CMS) and the Joint Commission is crucial to ensure compliance. This often involves subscribing to regulatory alerts and participating in webinars and training sessions offered by these agencies.
- Industry Publications: Reading industry-specific journals and publications keeps me informed about emerging trends and best practices. This includes keeping up to date on legal cases and their implications for risk management.
- Continuing Education: Participating in regular continuing education programs ensures that my knowledge and skills remain current and relevant. This allows for continuous learning and adaptation to the ever-changing regulatory and technological landscape.
Q 27. Describe your experience with risk transfer strategies such as insurance.
Risk transfer, primarily through insurance, is a key strategy in healthcare risk management. It involves shifting the financial burden of potential losses to an insurance company. My experience includes working with insurance brokers to assess our organization’s risk profile and select appropriate coverage. This involves negotiating policy terms, ensuring adequate coverage limits, and managing claims when necessary.
Beyond traditional insurance, other risk transfer mechanisms exist, such as captive insurance companies (insurance companies owned by the organization) and contractual risk transfers (shifting liability through contracts with vendors). The choice of risk transfer strategy depends on the organization’s risk tolerance, financial capacity, and the specific risks involved. A balanced approach that combines risk mitigation strategies with appropriate risk transfer mechanisms is often the most effective approach.
Q 28. How do you handle ethical dilemmas related to risk management decisions?
Ethical dilemmas in risk management are unavoidable, often involving conflicts between patient safety, cost considerations, and legal requirements.
When faced with such dilemmas, I follow a structured approach:
- Identify the ethical conflict: Clearly define the competing values and interests involved.
- Gather information: Collect relevant data and consult with relevant stakeholders, including legal counsel, ethics committees, and clinical staff.
- Explore alternative solutions: Brainstorm various options, weighing their ethical implications and potential consequences.
- Consult with ethics committees: Seek guidance from institutional ethics committees or other independent ethical review boards.
- Document the decision-making process: Maintain a thorough record of the ethical dilemma, the decision-making process, and the rationale behind the chosen course of action.
Transparency and open communication are essential throughout the process. The goal is to reach a decision that is both ethically sound and practically feasible, prioritizing patient well-being while adhering to relevant legal and regulatory guidelines. For example, balancing the cost of implementing a new safety protocol with the potential to prevent serious harm often necessitates carefully weighing the ethical implications of each decision.
Key Topics to Learn for Healthcare Risk Management Interview
- Risk Assessment & Identification: Understanding methodologies for identifying potential risks across various healthcare settings (e.g., hospitals, clinics, long-term care facilities). This includes analyzing patient safety incidents, regulatory compliance issues, and potential financial liabilities.
- Risk Mitigation Strategies: Developing and implementing practical strategies to reduce identified risks. This involves applying both proactive and reactive measures, leveraging data analysis, and collaborating with interdisciplinary teams to improve processes and protocols.
- Incident Reporting & Investigation: Mastering effective incident reporting systems, conducting thorough investigations, and implementing corrective actions to prevent recurrence. This requires understanding root cause analysis techniques and regulatory reporting requirements.
- Regulatory Compliance: Demonstrating a strong grasp of relevant regulations and accreditation standards (e.g., HIPAA, Joint Commission). This includes understanding the implications of non-compliance and the importance of maintaining accurate documentation.
- Insurance & Claims Management: Familiarity with healthcare insurance processes and claims management techniques. This involves understanding risk transfer mechanisms and strategies for minimizing financial losses.
- Data Analysis & Reporting: Utilizing data analysis tools to identify trends, patterns, and areas of improvement in risk management. This involves presenting findings effectively to stakeholders and using data to support decision-making.
- Ethical Considerations: Understanding and applying ethical principles in all aspects of risk management, including patient confidentiality, informed consent, and conflict of interest.
Next Steps
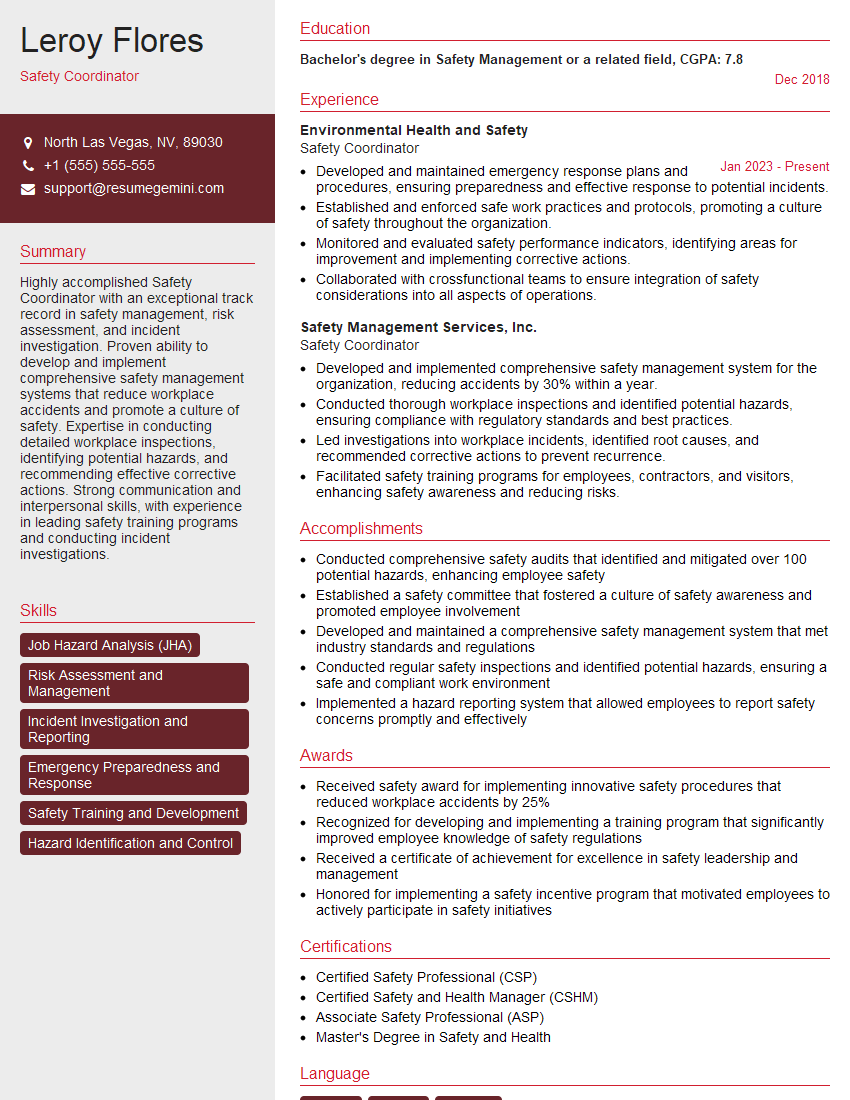
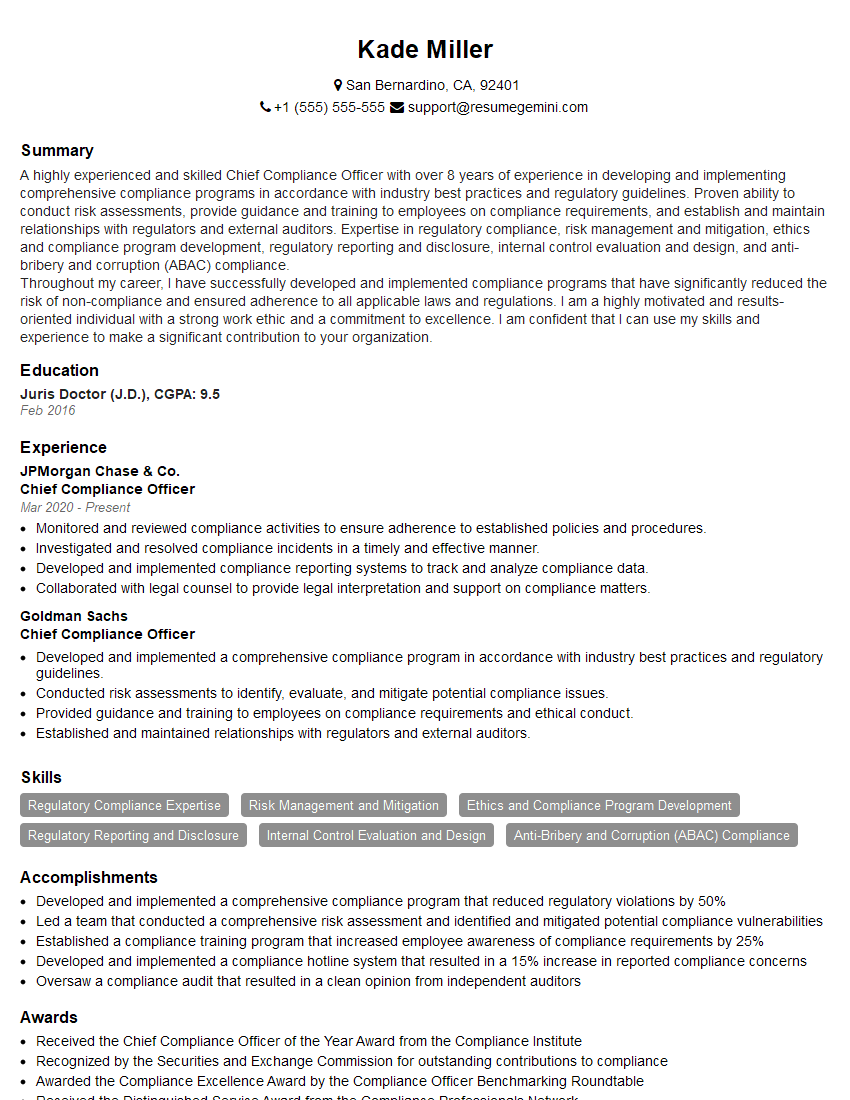
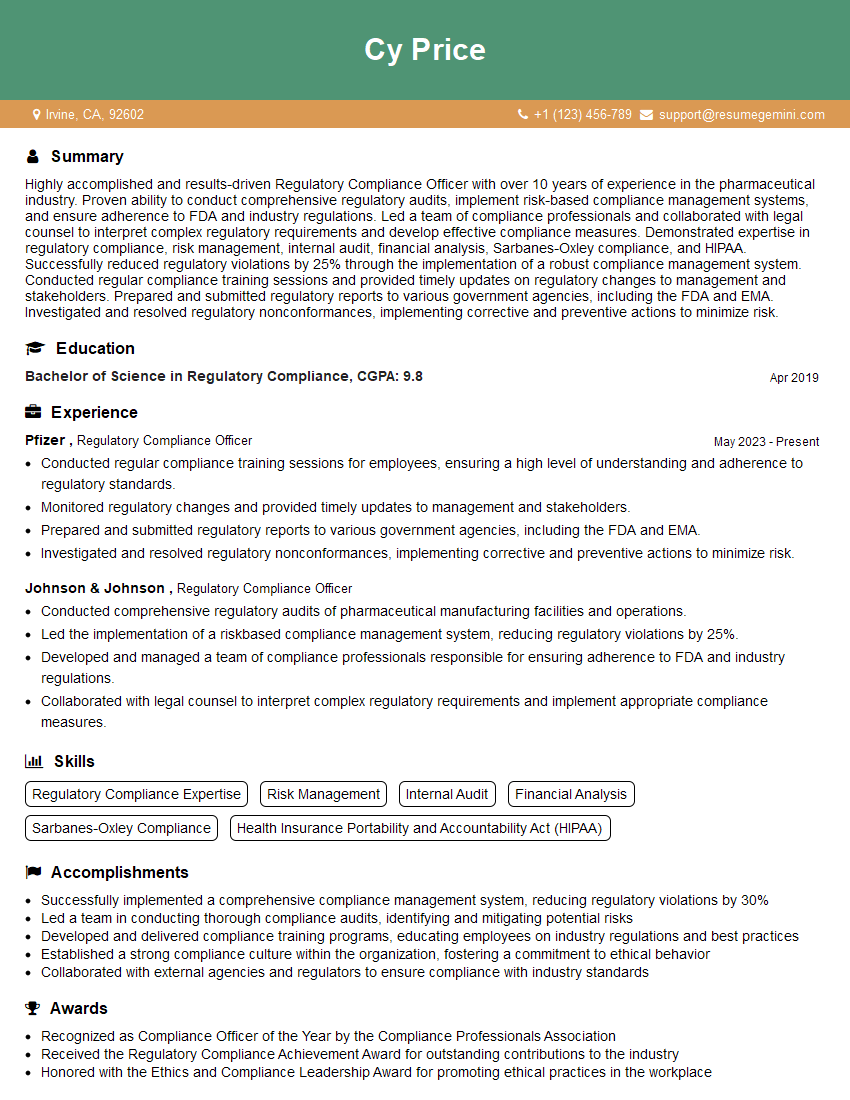
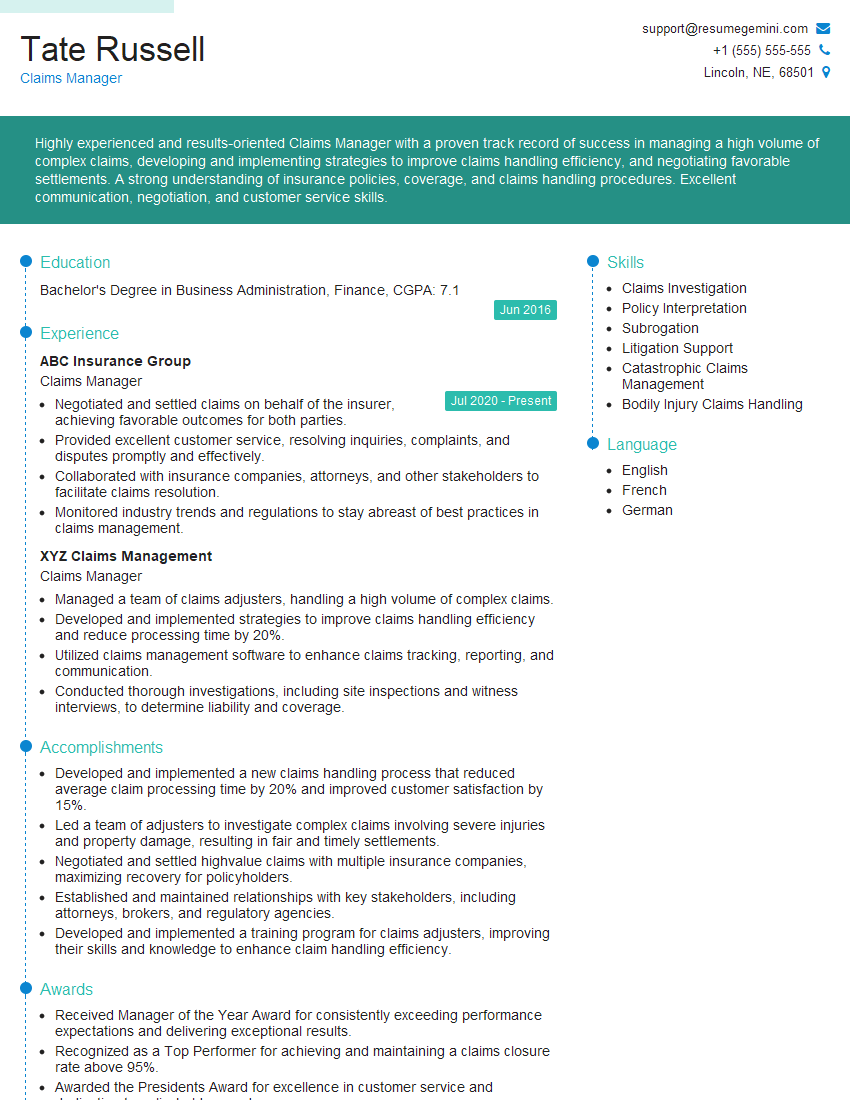
Mastering Healthcare Risk Management opens doors to exciting career advancements and leadership opportunities within the healthcare industry. A strong understanding of risk mitigation, compliance, and patient safety is highly sought after, making you a valuable asset to any healthcare organization. To enhance your job prospects, creating an ATS-friendly resume is crucial. This ensures your application is effectively scanned and reviewed by hiring managers. We encourage you to leverage ResumeGemini, a trusted resource for building professional and impactful resumes. Examples of resumes tailored to Healthcare Risk Management are available to help you create a compelling application that showcases your skills and experience.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Interesting Article, I liked the depth of knowledge you’ve shared.
Helpful, thanks for sharing.
Hi, I represent a social media marketing agency and liked your blog
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?