Preparation is the key to success in any interview. In this post, we’ll explore crucial Exome Sequencing interview questions and equip you with strategies to craft impactful answers. Whether you’re a beginner or a pro, these tips will elevate your preparation.
Questions Asked in Exome Sequencing Interview
Q 1. Explain the process of exome sequencing from sample preparation to data analysis.
Exome sequencing is a powerful technique focusing on the protein-coding regions (exons) of the genome, representing only about 1% of the total DNA. It’s a cost-effective alternative to whole-genome sequencing when focusing on identifying variations impacting protein function. The process unfolds in several key stages:
- Sample Preparation: This begins with extracting high-quality genomic DNA from a biological sample (blood, saliva, etc.). DNA is then fragmented to optimal sizes for library preparation.
- Library Preparation: Adapters are ligated to the DNA fragments, enabling amplification and sequencing. This step also involves quality control checks to ensure sufficient DNA quantity and quality.
- Exome Capture: This crucial step uses probes (short DNA sequences) to selectively enrich for exonic regions. The probes hybridize to the target DNA, allowing for the isolation of exons from the rest of the genome. Different capture methods exist, as discussed in the next question.
- Sequencing: The enriched exonic DNA is sequenced using high-throughput sequencing platforms (Illumina, PacBio, etc.), generating millions of short DNA reads.
- Data Analysis: This stage involves several steps:
- Read Mapping: Aligning the short reads to a reference human genome.
- Variant Calling: Identifying differences between the sequenced DNA and the reference genome (e.g., single nucleotide variations, insertions, deletions).
- Annotation: Adding information to the identified variants such as their location within genes, predicted effects on protein function, and known associations with diseases.
- Filtering and Prioritization: Reducing the number of identified variants to focus on those most likely to be clinically significant. (This will be discussed further in question 7).
The final output is a comprehensive report detailing the identified genetic variations, their potential clinical implications, and supporting evidence from various databases.
Q 2. Describe the different types of exome capture methods and their advantages/disadvantages.
Several methods exist for exome capture, each with its advantages and disadvantages:
- Solution-based hybrid capture: This is the most common method. It uses biotinylated oligonucleotide probes that bind to target DNA sequences. After hybridization, the probe-DNA complexes are captured using streptavidin beads, allowing for the isolation of enriched exonic DNA.
- Advantages: Relatively high coverage, good specificity, well-established protocols.
- Disadvantages: Can be expensive, may have some off-target capture, requires significant optimization for each target.
- Array-based capture: This method utilizes microarrays with probes attached to a solid surface. The fragmented DNA is hybridized to the microarray, and the bound DNA is then eluted and sequenced.
- Advantages: Potentially lower cost per sample than solution-based, suitable for high-throughput processing.
- Disadvantages: Typically lower coverage than solution-based capture, can be limited in the number of targets that can be captured.
The choice of method often depends on factors such as budget, throughput requirements, and desired coverage depth. Recent advancements are focusing on improving the efficiency, cost-effectiveness, and coverage uniformity of exome capture methods.
Q 3. How do you assess the quality of exome sequencing data?
Assessing exome sequencing data quality is crucial for ensuring the reliability of downstream analyses. Key metrics include:
- Sequencing depth: The average number of times each base in the exome is sequenced. Higher depth generally improves accuracy but increases cost.
- Coverage uniformity: How evenly the exome is sequenced. Uneven coverage can lead to missing variants in poorly covered regions. We aim for high uniformity.
- Mapping rate: Percentage of reads that successfully align to the reference genome. Low mapping rates might indicate poor library quality or contamination.
- Duplicate rate: Percentage of reads that are duplicates of other reads. High duplicate rates can indicate PCR amplification bias or problems with library preparation.
- GC bias: Variations in sequencing coverage across regions with different GC content (percentage of Guanine and Cytosine bases). This is a common artifact that needs to be corrected for during analysis.
- Base quality scores: Scores assigned to each base call, indicating the probability of it being correct. Low base quality scores can indicate sequencing errors.
Quality control metrics are often visualized using plots (e.g., coverage distribution plots, GC bias plots) to easily assess the quality and identify potential issues. Samples failing quality control checks need to be re-processed or excluded.
Q 4. What are common artifacts and biases in exome sequencing data, and how are they addressed?
Exome sequencing data is prone to several artifacts and biases:
- GC bias: Regions with high or low GC content are often under- or over-represented, respectively.
- PCR amplification bias: Certain regions may be amplified preferentially during PCR, leading to uneven coverage.
- Capture bias: Some exonic regions may not be captured efficiently by the probes, resulting in low or no coverage.
- Mapping bias: Reads with ambiguous mapping locations may be incorrectly assigned to the reference genome.
These biases can be addressed using various methods:
- Normalization: Adjusting the read counts to account for GC bias and PCR amplification bias.
- Improved capture methods: Utilizing optimized probes and capture protocols to minimize capture bias.
- Improved mapping algorithms: Using sophisticated mapping algorithms that handle ambiguous alignments more effectively.
- Quality control filtering: Removing reads or regions with low mapping quality or coverage.
Careful consideration of these biases and their mitigation is crucial for accurate variant interpretation.
Q 5. Explain the concept of variant calling and the algorithms used.
Variant calling is the process of identifying differences between the sequenced DNA and the reference genome. It involves comparing aligned reads to the reference sequence and detecting variations like single nucleotide polymorphisms (SNPs), insertions, and deletions (INDELS).
Algorithms used for variant calling are sophisticated and constantly evolving. Popular algorithms include:
- GATK HaplotypeCaller: A widely used algorithm that considers local haplotype information to improve variant calling accuracy.
- FreeBayes: An algorithm that uses Bayesian methods to call variants and estimate their quality.
- SAMtools mpileup: A simpler algorithm that calls variants based on read counts at each position.
These algorithms consider various factors such as read depth, base quality scores, mapping quality, and strand bias to determine the likelihood of a variant being true. The output of variant calling is a variant call format (VCF) file that lists the identified variants and associated quality metrics.
Q 6. Describe different types of genetic variants identified through exome sequencing (SNVs, INDELS, CNVs).
Exome sequencing identifies various types of genetic variants:
- Single Nucleotide Variants (SNVs): Changes in a single nucleotide base (e.g., A to G). SNVs can be synonymous (no change in amino acid sequence), missense (change in amino acid sequence), or nonsense (creating a premature stop codon).
- Insertions and Deletions (INDELS): Insertions or deletions of one or more nucleotides. INDELS can cause frameshift mutations, leading to altered protein sequences downstream from the INDEL.
- Copy Number Variations (CNVs): Variations in the number of copies of a DNA segment. CNVs can involve large genomic regions and can lead to dosage effects impacting gene expression.
Understanding the type and functional consequences of each variant is critical for interpretation. For example, a nonsense SNV is likely to be more damaging than a synonymous SNV.
Q 7. How do you filter and prioritize variants identified in an exome sequencing experiment?
Filtering and prioritizing variants is essential due to the large number of variants typically identified in an exome sequencing experiment (hundreds of thousands). This involves applying a series of filters to reduce the number of variants to a manageable set that warrants further investigation.
Filtering steps include:
- Filtering by quality metrics: Removing variants with low quality scores (e.g., low read depth, low variant allele frequency).
- Filtering by allele frequency: Removing common variants found in population databases (e.g., dbSNP, gnomAD), as these are less likely to be disease-causing in a given individual.
- Filtering by predicted impact: Removing variants that are predicted to be benign or have no effect on protein function using tools like SIFT or PolyPhen-2.
- Filtering by genomic location: Focusing on variants located within known disease-associated genes or regions.
Prioritization involves ranking the remaining variants based on various criteria, including predicted impact on protein function, evidence from literature or databases (ClinVar, OMIM), and their co-occurrence with other variants. This process often integrates information from multiple sources to establish a ranking that assists in guiding further investigation.
For example, a rare missense variant in a gene known to cause a specific disease, and with strong literature supporting its association, would be given higher priority than a common synonymous variant in a gene with unknown function.
Q 8. Explain the use of annotation databases (e.g., dbSNP, ClinVar, gnomAD) in variant interpretation.
Annotation databases are crucial in exome sequencing for interpreting the significance of identified variants. Think of them as comprehensive dictionaries for genomic variations. They contain information about previously identified variants, their frequencies in populations, and potential clinical implications. Key databases include dbSNP (a database of single nucleotide polymorphisms), ClinVar (a collection of interpretations of the clinical significance of variants), and gnomAD (a massive database of human genomic variation).
For example, if my analysis identifies a novel variant in the BRCA1 gene, I can consult ClinVar to see if this variant has been previously reported and whether it has been associated with an increased risk of breast cancer. Similarly, gnomAD helps assess the frequency of the variant in the general population. A very rare variant is more likely to be disease-causing than a common one. The combined information from these databases helps me classify the variant’s pathogenicity, moving from a purely computational finding to a potentially clinically relevant piece of information.
- dbSNP: Provides a comprehensive list of known SNPs.
- ClinVar: Contains interpretations of variant clinical significance submitted by various labs and researchers.
- gnomAD: Offers allele frequencies across a diverse global population.
Q 9. What are the ethical considerations associated with exome sequencing?
Exome sequencing raises several significant ethical considerations. The most prominent is the potential for incidental findings – the discovery of unexpected variations unrelated to the reason for testing. For example, a patient undergoing exome sequencing for a suspected cardiac condition might also have a variant identified that indicates a predisposition to a different disease, like Alzheimer’s. This raises questions about the patient’s right to know, the potential for psychological distress, and the implications for family members who may also carry the variant.
Another key concern is data privacy and security. Exome sequencing data is highly personal and sensitive, containing intimate details about an individual’s genetic makeup. Strict protocols are necessary to ensure that this data is protected from unauthorized access and misuse. Informed consent is paramount; patients must fully understand what the test involves, its limitations, and the potential implications before consenting to it. Genetic discrimination is another concern, where individuals may face unfair treatment from employers or insurance companies based on their genetic information.
Q 10. Describe your experience with variant interpretation and classification.
I have extensive experience in variant interpretation and classification, using a combination of computational and manual review techniques. My workflow typically involves several steps. First, I use variant annotation tools to gather information from databases like dbSNP, ClinVar, and gnomAD (as discussed previously). Next, I assess the variant’s predicted impact on protein function, using tools that predict changes to amino acid sequences and protein structure. I also consider the variant’s frequency in the population, as rare variants are more suspicious for pathogenicity.
A crucial aspect is considering the clinical context. For example, a variant associated with a specific phenotype (observable characteristic or trait) is more likely to be causative if the patient shows that very phenotype. Finally, I utilize established guidelines like ACMG (American College of Medical Genetics and Genomics) standards to classify the variant’s pathogenicity (benign, likely benign, uncertain significance, likely pathogenic, pathogenic). This involves weighing the available evidence and often requires careful consideration and judgment. I’ve worked on various projects involving rare diseases, cancer genomics, and pharmacogenomics, which have honed my variant interpretation skills.
Q 11. Explain the difference between germline and somatic variants.
Germline and somatic variants differ in their origin and inheritance. Germline variants are present in all cells of the body from the time of conception and are inherited from parents. These variations are passed down through generations and contribute to inherited genetic conditions. In contrast, somatic variants arise in somatic cells (non-reproductive cells) after conception. These mutations aren’t inherited and typically affect only a subset of cells within the body. A prime example of somatic variants are those found in cancer cells.
Think of it this way: Germline variants are like a blueprint error present in all the building’s plans, while somatic variants are like damage occurring to some parts of the already built structure during its lifespan. Exome sequencing can identify both types, depending on the sample source. Blood samples usually reveal germline variants, while tumor biopsies mainly show somatic mutations.
Q 12. How do you handle missing data in exome sequencing analysis?
Missing data is a common challenge in exome sequencing. Several strategies can be employed to handle this. The first step is to identify the cause of missing data; it can result from low sequencing coverage, alignment difficulties, or issues with the sample preparation. Once the reason is known, appropriate methods can be applied.
One approach is to simply exclude variants located in regions with excessive missing data; this is a conservative approach that minimizes the risk of false positives. Alternatively, imputation methods can be employed to infer the missing genotypes based on surrounding data and population frequency information. The choice of strategy depends on the amount of missing data, the study’s goals, and the tolerance for uncertainty.
Q 13. Describe your experience with various bioinformatics tools used in exome sequencing analysis (e.g., BWA, GATK, Picard).
My experience encompasses a wide range of bioinformatics tools used in exome sequencing analysis. I’m proficient in using tools for read mapping (such as BWA – Burrows-Wheeler Aligner), variant calling (GATK – Genome Analysis Toolkit), and variant annotation (ANNOVAR, SNPEff). Picard is a valuable tool for preprocessing steps like sorting and marking duplicates. I’m also experienced in using variant filtering tools, which are essential for prioritizing variants worthy of further investigation from the massive dataset generated by exome sequencing.
For example, I have used BWA to align sequencing reads to the human reference genome, then GATK for variant calling, followed by ANNOVAR to annotate the called variants with information about their location, predicted effect on genes, and frequency in population databases. Picard is always used for quality control and data cleaning before downstream analyses. This combined pipeline is crucial for accurate and efficient analysis of exome sequencing data.
Q 14. Explain your understanding of different sequencing platforms (Illumina, PacBio, etc.) and their applications in exome sequencing.
Illumina sequencing platforms are currently the dominant technology for exome sequencing due to their high throughput, relatively low cost, and high accuracy. They’re ideal for generating large amounts of data needed for comprehensive exome coverage. However, Illumina’s short read lengths can pose challenges in resolving complex regions of the genome.
PacBio and Oxford Nanopore Technologies offer long-read sequencing, which can resolve repetitive regions and structural variations more effectively than Illumina. This is particularly beneficial in situations where these genomic features are expected to play a crucial role. While long-read technologies are becoming more cost-effective, they are currently less widely used for exome sequencing due to their higher error rates and lower throughput compared to Illumina. The choice of platform often depends on the specific research question and the trade-offs between cost, read length, accuracy, and throughput.
Q 15. How do you assess the coverage and depth of exome sequencing data?
Assessing coverage and depth in exome sequencing is crucial for ensuring the reliability of our findings. Coverage refers to the percentage of target exonic regions that are sequenced, while depth signifies the number of times each base is sequenced. Think of it like painting a wall – coverage is how much of the wall is painted, and depth is how many coats of paint you applied to each section.
We typically use visualization tools and metrics like the following to evaluate coverage and depth:
- Mean coverage: The average number of reads covering each base. A higher mean coverage generally indicates better data quality.
- Uniformity of coverage: We look at the distribution of coverage across the exome. Ideally, we want uniform coverage, avoiding regions with significantly low or high coverage, indicating potential biases in library preparation or target enrichment.
- Percentage of bases with at least X coverage: This metric helps determine the percentage of the exome covered at a minimum depth (e.g., 95% of bases at 20x coverage). This ensures that we’ve sequenced most regions sufficiently to detect variants with reasonable confidence.
We analyze these metrics using dedicated bioinformatics tools such as Picard and Qualimap, generating coverage reports and visualizations to identify potential problems. For instance, a low mean coverage may necessitate re-sequencing or optimization of library preparation.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Describe your experience with quality control metrics for exome sequencing data.
Quality control (QC) is paramount in exome sequencing. It involves rigorous checks at each stage, from raw data to variant calling, to ensure data accuracy and reliability. We routinely assess various QC metrics:
- Alignment rate: The percentage of reads successfully mapped to the reference genome. Low alignment rates could indicate problems with sequencing quality or library preparation.
- Duplicate rate: The percentage of PCR duplicates. High duplicate rates suggest PCR amplification bias, which can lead to false positive variant calls.
- GC bias: Sequencing biases caused by the GC content of the target region, often influencing coverage uniformity. We check if the coverage is uniform across various GC content regions.
- Base quality scores: These scores indicate the probability that a base call is accurate. Low base quality scores increase the chances of false variant calls.
- Mapping quality scores: These scores represent the accuracy of read alignment to the reference genome. Lower mapping quality scores reduce confidence in variant calls.
We use software like FastQC, Picard, and Genome Analysis Toolkit (GATK) to analyze these metrics, identify and correct issues like adapter contamination or low-quality reads. For example, if we observe a high duplicate rate, we investigate potential problems in the library preparation and consider using unique molecular identifiers (UMIs) to reduce duplication in future experiments. These QC steps are crucial before proceeding to variant calling and downstream analysis.
Q 17. How would you troubleshoot low coverage or high error rates in exome sequencing data?
Troubleshooting low coverage or high error rates necessitates a systematic approach. We first review the QC metrics (as described above) to identify potential causes.
- Low Coverage: Low coverage can stem from several factors: inadequate DNA input, poor library preparation, insufficient sequencing depth. We might investigate DNA quality and concentration, repeat library preparation with optimization of the protocol, or increase the sequencing depth.
- High Error Rates: High error rates can arise from low-quality sequencing data, poor alignment, or incorrect variant calling parameters. Here, we examine base quality scores, mapping quality, and reassess the variant calling parameters, potentially rerunning the analysis with stricter filters.
For example, if a specific region shows consistently low coverage, we can investigate the design of the capture probes (if using target enrichment) or re-evaluate the mappability of that genomic region. In the case of systematic errors across the whole dataset, problems with the sequencer may need further investigation.
Debugging is an iterative process. We often need to revisit previous steps, re-evaluate experimental procedures, and adjust bioinformatic pipelines to resolve these issues. A thorough understanding of the experimental workflow and bioinformatic tools is essential for efficient troubleshooting.
Q 18. Explain the concept of Mendelian inheritance and how it applies to exome sequencing analysis.
Mendelian inheritance describes how traits are passed from parents to offspring. In exome sequencing, we use this principle to identify variants that might explain a patient’s phenotype (observable characteristics). For example, if a child has a recessive disorder, we’d expect to find two copies of the same variant in the child’s genome, one inherited from each parent.
In analysis, we look at variant segregation within families. For example:
- Autosomal recessive: Affected individuals inherit one copy of the variant from each parent who may be carriers (heterozygous). Unaffected siblings might be homozygous for the wild-type allele or heterozygous carriers.
- Autosomal dominant: Affected individuals need only one copy of the variant to exhibit the phenotype. Affected individuals typically have at least one affected parent.
- X-linked recessive: More common in males as they only need one affected X chromosome.
This information is essential for filtering variants and prioritizing those likely to be causative. We use specialized tools that integrate pedigree information to predict inheritance patterns and identify candidate variants based on Mendelian principles. Departures from Mendelian inheritance (e.g., de novo mutations) also offer crucial insights into the disease mechanism.
Q 19. How do you distinguish between pathogenic and benign variants?
Distinguishing pathogenic from benign variants is a critical step in exome sequencing analysis. It’s not a simple task, and it often requires a multi-faceted approach.
We utilize several strategies:
- Variant frequency in population databases: Rare variants are more likely to be pathogenic than common variants. We consult databases like gnomAD to assess the frequency of a given variant in the general population.
- Prediction tools: Software predicts the functional impact of a variant based on its location (exonic, intronic, etc.) and the type of change (missense, nonsense, etc.). Popular tools include SIFT, PolyPhen-2, CADD, and REVEL.
- Clinical databases: ClinVar compiles information on variants observed in patients with specific diseases, providing insights into their clinical significance. We use these databases to check for prior observations of the variant in similar phenotypes.
- Conserved regions: Variants in highly conserved regions of the genome, meaning regions that have remained similar over long evolutionary timescales, are more likely to be harmful as changes there may disrupt critical protein function.
- Co-segregation with the phenotype in family studies: Observing consistent inheritance of a variant with the disease phenotype strengthens the evidence for pathogenicity.
- Experimental validation: In some cases, additional experiments (e.g., functional assays) are necessary to determine whether a variant is truly pathogenic.
The interpretation of variants involves careful consideration of all this evidence. It’s an iterative process, and expert review is often needed, especially for variants with uncertain significance.
Q 20. Describe your experience with different variant effect prediction tools.
I have extensive experience using several variant effect prediction tools. Each tool has its strengths and weaknesses. It’s important to use a combination of tools and not rely solely on one for accurate prediction.
- SIFT (Sorting Intolerant From Tolerant): Predicts whether an amino acid substitution affects protein function based on sequence homology.
- PolyPhen-2 (Polymorphism Phenotyping): Uses multiple sequence alignments and physical-chemical properties of amino acids to predict the effect of amino acid substitutions.
- CADD (Combined Annotation Dependent Depletion): Integrates multiple annotations to generate a single score representing the deleteriousness of a variant. Higher CADD scores imply a greater likelihood of pathogenicity.
- REVEL (Rare Exome Variant Ensemble Learner): Combines predictions from multiple algorithms to improve accuracy.
I use these tools to filter variants, prioritize those with high prediction scores for further investigation, and incorporate the results into the overall assessment of pathogenicity alongside other lines of evidence (as mentioned in the previous answer). We always critically evaluate the outputs of these tools, mindful that they provide probabilities, not definitive answers. Contextual information and manual review remain crucial.
Q 21. What are the limitations of exome sequencing?
While exome sequencing is a powerful tool, it has limitations:
- Coverage gaps: Some regions of the genome are difficult to capture or sequence effectively, leading to incomplete coverage. This can result in missing variants.
- Intronic and regulatory variants: Exome sequencing primarily focuses on exons, missing potentially important variants in introns or regulatory regions.
- Copy number variations (CNVs): Exome sequencing is less effective at detecting CNVs, which involve duplications or deletions of larger genomic segments.
- Non-coding RNA: The majority of non-coding RNAs are typically not captured in exome sequencing, neglecting a portion of the genome with important regulatory functions.
- Variant interpretation challenges: As mentioned before, differentiating pathogenic from benign variants can be difficult, requiring careful consideration of multiple lines of evidence and expert judgment. Variants of uncertain significance are common.
- Cost and time: Exome sequencing can be expensive and time-consuming, representing a considerable investment.
It’s crucial to understand these limitations and appropriately interpret the results. Often, exome sequencing serves as one component of a larger diagnostic strategy, which may involve other genetic testing modalities, such as genome sequencing or targeted gene panels, to address these limitations.
Q 22. Explain the role of exome sequencing in different clinical applications (e.g., diagnostics, pharmacogenomics).
Exome sequencing, focusing on the protein-coding regions (exons) of the genome, plays a crucial role across various clinical applications. Its power lies in its ability to identify disease-causing variants efficiently and cost-effectively compared to whole-genome sequencing.
- Diagnostics: Exome sequencing is invaluable in diagnosing rare genetic disorders. For example, a child with unexplained developmental delays might undergo exome sequencing to identify potential mutations in genes associated with such conditions. The results help clinicians confirm a diagnosis, guide treatment strategies, and offer genetic counseling to the family. This is particularly useful when a clinical presentation is atypical or when multiple genes are implicated.
- Pharmacogenomics: Understanding an individual’s genetic makeup through exome sequencing allows for personalized medicine. By analyzing genes involved in drug metabolism (e.g., CYP450 genes), we can predict a patient’s response to specific medications. This enables clinicians to select the most effective drug and dosage, minimizing adverse effects and maximizing therapeutic benefit. For instance, identifying variants in genes affecting warfarin metabolism allows for precise dose adjustment, preventing bleeding complications.
- Cancer Genomics: Exome sequencing is used to identify somatic mutations (mutations present in tumor cells but not in normal cells) driving cancer development. This informs targeted cancer therapies and helps monitor disease progression. The identification of driver mutations in a tumor sample can guide the selection of specific cancer drugs that target these mutations.
In essence, exome sequencing acts as a powerful diagnostic and predictive tool, moving healthcare towards personalized and precision medicine.
Q 23. Describe your experience with analyzing exome sequencing data from different sample types (e.g., blood, saliva, tumor tissue).
My experience encompasses analyzing exome sequencing data from various sample types, each presenting unique challenges. I’ve worked extensively with blood samples (DNA extracted from peripheral blood mononuclear cells or PBMCs), which are the most common source. However, I also have experience with saliva samples, which, while easier to collect, often have lower DNA yields and higher rates of degradation, requiring careful processing and quality control.
Tumor tissue presents its own set of complexities. Tumor heterogeneity—the presence of different genetic variations within the tumor—requires careful consideration during analysis. We need to distinguish between germline variants (inherited mutations) and somatic variants (mutations acquired during the individual’s lifetime), which are often the key drivers of tumor growth. I’ve used techniques like matched normal-tumor comparisons to effectively identify somatic variants. The quality of tumor DNA is often affected by the presence of non-tumorous cells within the sample, necessitating methods for assessing tumor purity. For all samples, rigorous quality control measures, starting from DNA extraction to bioinformatic analysis, are essential to ensure data reliability.
Q 24. How do you manage large exome sequencing datasets?
Managing large exome sequencing datasets requires a multi-faceted approach that leverages both computational resources and efficient data management strategies. The sheer size of these datasets necessitates specialized storage solutions and powerful computational infrastructure.
- Cloud Computing: We utilize cloud platforms like AWS or Google Cloud to store and process exome sequencing data. These platforms offer scalability and cost-effectiveness, enabling efficient handling of large volumes of data.
- Data Compression: Employing appropriate data compression techniques significantly reduces storage requirements and speeds up data transfer and analysis.
- Database Management: We employ relational databases (such as MySQL or PostgreSQL) and NoSQL databases (like MongoDB) to effectively manage and query the data. This structured approach allows for efficient retrieval of specific information.
- Parallel Processing: Utilizing parallel processing techniques, such as those found in software like GATK or Picard, significantly speeds up the bioinformatic analysis pipeline.
- Data Version Control: Implementing a robust version control system ensures data integrity and traceability, allowing easy tracking of changes and reproducibilty.
By implementing these strategies, we ensure efficient data management, facilitating fast and accurate analysis while minimizing storage costs.
Q 25. Explain your experience with data visualization and reporting techniques for exome sequencing data.
Data visualization and reporting are critical for effectively communicating exome sequencing findings. I’m proficient in using various tools and techniques to create clear and informative visualizations and reports, tailored to the specific audience (clinicians, researchers, or patients).
- Genome Browsers (IGV, UCSC Genome Browser): These are essential for visualizing variant calls in the context of the genome, allowing for assessment of variant location and surrounding genomic features.
- Variant Annotation Tools (ANNOVAR, SIFT, PolyPhen-2): I leverage these tools to predict the functional impact of identified variants, helping prioritize those most likely to be disease-causing.
- Custom Scripts and R Packages (ggplot2, plotly): To create custom visualizations tailored to specific research questions or clinical needs, I utilize scripting languages like Python and R along with visualization packages such as ggplot2 for static plots and plotly for interactive ones.
- Interactive Dashboards: For complex datasets, interactive dashboards enable users to explore data dynamically, filter results, and access detailed information on individual variants.
- Clinical Reports: Final reports are meticulously prepared, following clinical guidelines and incorporating only validated and relevant findings, in a format easily understandable by clinicians.
My goal is to generate reports that are not only visually appealing but also provide actionable insights to aid clinical decision-making.
Q 26. Describe your experience with working in a clinical diagnostic laboratory setting (if applicable).
While I haven’t directly worked in a clinical diagnostic laboratory setting, my experience closely aligns with the requirements. My research has consistently focused on translating exome sequencing data into clinically relevant insights. I understand the stringent quality control measures, data validation procedures, and regulatory compliance necessary for a clinical diagnostic laboratory. I am familiar with relevant guidelines such as CAP and CLIA regulations. My collaborations with clinical researchers and my meticulous approach to data analysis ensures the accuracy and reliability of my findings. I am confident in my ability to adapt to a clinical laboratory setting and contribute effectively to a team focused on delivering accurate and timely diagnostic results.
Q 27. What are your future career aspirations in the field of exome sequencing?
My future aspirations involve leveraging my expertise in exome sequencing to advance personalized medicine. I envision contributing to the development of improved analytical methods for identifying and interpreting rare genetic variants, focusing on the development of AI-powered tools to enhance variant interpretation and improve diagnostic accuracy. I’m also interested in applying exome sequencing to identify novel therapeutic targets for complex diseases and developing strategies to incorporate these findings into clinical practice.
Ultimately, I aim to play a key role in bridging the gap between genomic research and clinical applications, ultimately improving patient care through the power of genomic information.
Key Topics to Learn for Exome Sequencing Interview
- Target Enrichment Strategies: Understand the various methods used for exome capture, including their strengths and weaknesses (e.g., solution-based hybridization, array-based capture). Consider the impact of target design on data quality.
- Next-Generation Sequencing (NGS) Technologies: Become familiar with the different NGS platforms used for exome sequencing (Illumina, PacBio, etc.) and their respective advantages and limitations. Be prepared to discuss read length, sequencing depth, and error rates.
- Bioinformatics Analysis: Master the fundamental bioinformatics tools and pipelines used for exome sequencing data analysis, including read alignment (BWA, Bowtie2), variant calling (GATK, Freebayes), and variant annotation (ANNOVAR, SIFT). Understand the concept of variant filtering and prioritization.
- Variant Interpretation: Develop a strong understanding of how to interpret genetic variants identified through exome sequencing, considering factors like allele frequency, predicted impact on protein function, and inheritance patterns. Be able to discuss different variant classification schemas (e.g., ClinVar).
- Clinical Applications of Exome Sequencing: Explore the diverse applications of exome sequencing in various clinical settings, including diagnostics (rare diseases, cancer), pharmacogenomics, and reproductive health. Be prepared to discuss ethical considerations.
- Data Quality Control and Troubleshooting: Understand common issues encountered in exome sequencing data analysis, such as low coverage regions, alignment artifacts, and contamination. Be prepared to discuss strategies for troubleshooting and quality control.
- Ethical Considerations and Data Privacy: Familiarize yourself with the ethical implications of exome sequencing, including data privacy, informed consent, and potential biases in interpretation.
Next Steps
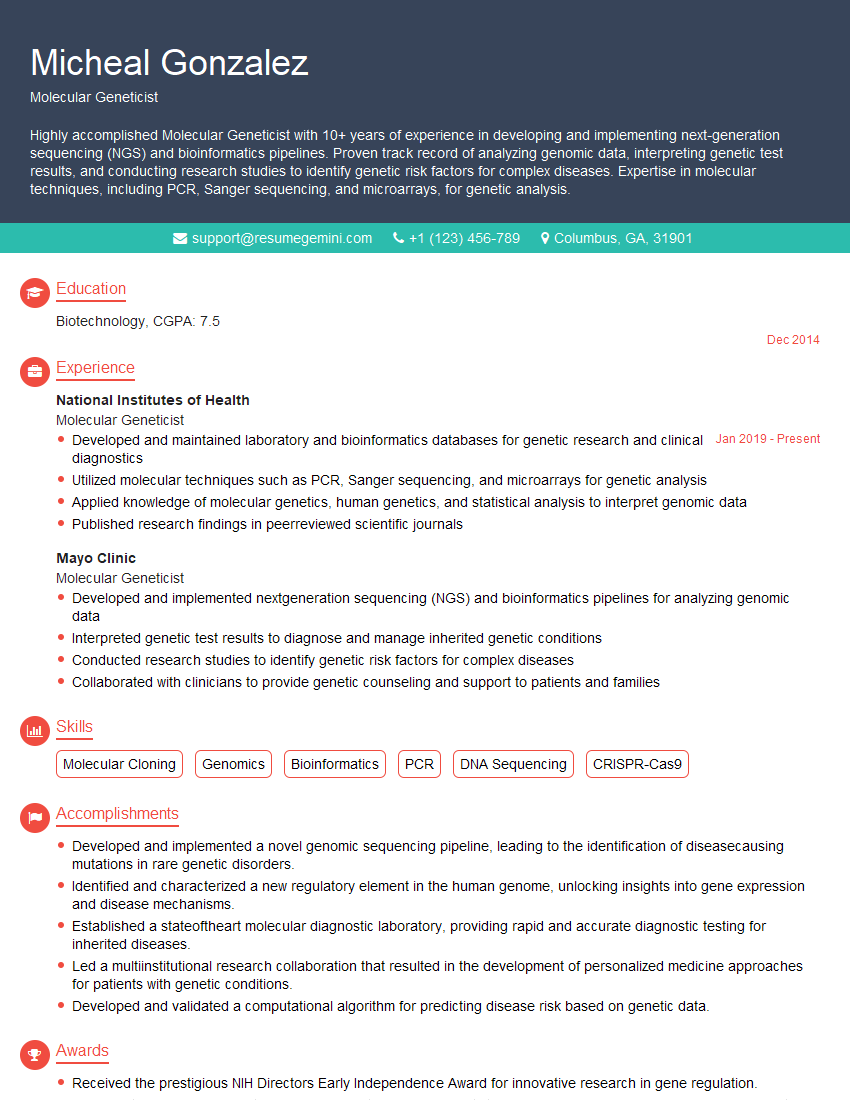
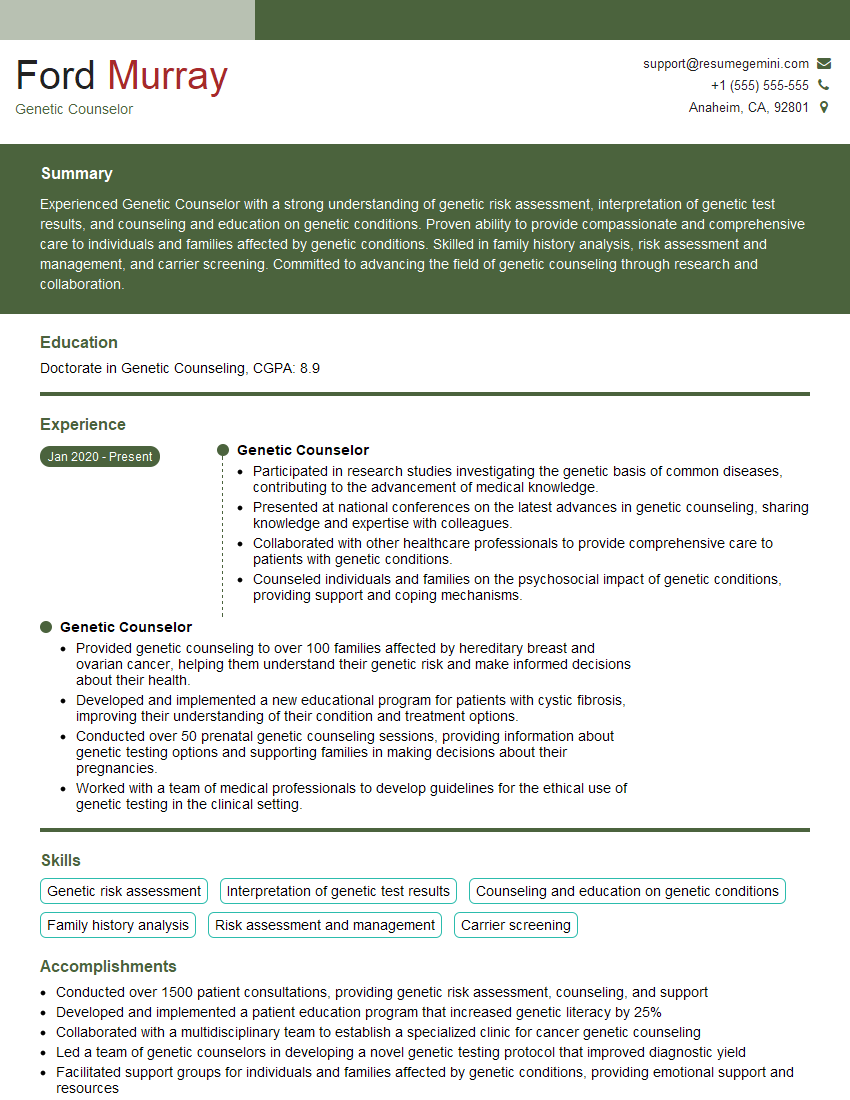
Mastering exome sequencing opens doors to exciting career opportunities in genomics, diagnostics, and personalized medicine. To maximize your job prospects, it’s crucial to present your skills effectively. Creating an ATS-friendly resume is key to getting your application noticed. ResumeGemini is a valuable resource to help you build a professional resume that highlights your expertise in exome sequencing. They provide examples of resumes tailored to this field, ensuring your qualifications shine.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
hello,
Our consultant firm based in the USA and our client are interested in your products.
Could you provide your company brochure and respond from your official email id (if different from the current in use), so i can send you the client’s requirement.
Payment before production.
I await your answer.
Regards,
MrSmith
hello,
Our consultant firm based in the USA and our client are interested in your products.
Could you provide your company brochure and respond from your official email id (if different from the current in use), so i can send you the client’s requirement.
Payment before production.
I await your answer.
Regards,
MrSmith
These apartments are so amazing, posting them online would break the algorithm.
https://bit.ly/Lovely2BedsApartmentHudsonYards
Reach out at [email protected] and let’s get started!
Take a look at this stunning 2-bedroom apartment perfectly situated NYC’s coveted Hudson Yards!
https://bit.ly/Lovely2BedsApartmentHudsonYards
Live Rent Free!
https://bit.ly/LiveRentFREE
Interesting Article, I liked the depth of knowledge you’ve shared.
Helpful, thanks for sharing.
Hi, I represent a social media marketing agency and liked your blog
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?