Cracking a skill-specific interview, like one for Statistical and Epidemiological Analysis, requires understanding the nuances of the role. In this blog, we present the questions you’re most likely to encounter, along with insights into how to answer them effectively. Let’s ensure you’re ready to make a strong impression.
Questions Asked in Statistical and Epidemiological Analysis Interview
Q 1. Explain the difference between correlation and causation.
Correlation and causation are often confused, but they represent distinct relationships between variables. Correlation simply indicates a statistical association between two or more variables – when one changes, the other tends to change as well. This association can be positive (both increase together), negative (one increases as the other decreases), or zero (no relationship). Causation, on the other hand, implies that one variable directly influences or causes a change in another. Just because two things are correlated doesn’t mean one causes the other.
Example: Ice cream sales and crime rates are often positively correlated. This doesn’t mean that eating ice cream causes crime! Both are likely influenced by a third variable: hot weather. Hot weather increases ice cream sales and also increases the likelihood of people being outside, potentially leading to more crime opportunities. The correlation is spurious; there’s no causal link between ice cream and crime.
To establish causation, we need stronger evidence, often involving controlled experiments or rigorous observational studies with careful control of confounding variables (factors that influence both the presumed cause and effect). Techniques like regression analysis can help quantify the association, but they cannot prove causation on their own.
Q 2. Describe different types of sampling methods and their biases.
Sampling methods are crucial in statistical and epidemiological studies, as it’s usually impractical to study the entire population. Different methods introduce different biases.
- Simple Random Sampling: Each member of the population has an equal chance of being selected. Bias is minimized if the sampling frame (list of population members) is accurate and complete. However, it can be inefficient for large, geographically dispersed populations.
- Stratified Sampling: The population is divided into strata (e.g., age groups, genders) and a random sample is taken from each stratum. This ensures representation from all subgroups and reduces sampling error compared to simple random sampling, but requires prior knowledge of the population’s characteristics.
- Cluster Sampling: The population is divided into clusters (e.g., schools, neighborhoods), and some clusters are randomly selected, with all members within the selected clusters being studied. This is cost-effective but can lead to clustering bias if the clusters are not representative of the overall population.
- Convenience Sampling: Participants are selected based on their availability or ease of access. This introduces significant bias, as the sample is unlikely to represent the population accurately. For example, surveying only your friends about political preferences could not represent the population’s entire perspective.
- Systematic Sampling: Every kth member of a list is selected. While seemingly simple, it can lead to bias if the list has a hidden pattern or periodicity that aligns with the sampling interval.
Bias in sampling occurs when the sample doesn’t accurately reflect the population. This can lead to misleading conclusions in the analysis.
Q 3. What are the assumptions of linear regression?
Linear regression models the relationship between a dependent variable (outcome) and one or more independent variables (predictors) assuming a linear relationship. Several key assumptions must be met for valid results:
- Linearity: The relationship between the dependent and independent variables is linear. Scatter plots and residual plots can assess this assumption.
- Independence: Observations are independent of each other. This is violated in time series data or clustered data where observations are related. Proper modeling techniques like mixed-effects models should be used in such cases.
- Homoscedasticity: The variance of the errors (residuals) is constant across all levels of the independent variables. Funnel-shaped residual plots indicate heteroscedasticity, potentially requiring transformations or alternative models.
- Normality: The errors are normally distributed. Histograms and Q-Q plots can assess this assumption. Moderate deviations from normality are often acceptable, especially with larger sample sizes.
- No multicollinearity: Independent variables are not highly correlated with each other. High multicollinearity makes it difficult to estimate the individual effects of predictors. Variance inflation factors (VIFs) can detect multicollinearity.
- No autocorrelation: In time-series data, errors are not correlated over time. Durbin-Watson test is used to detect autocorrelation. This can occur if there is a temporal dependency.
Violation of these assumptions can lead to biased and inefficient estimates of regression coefficients.
Q 4. How do you handle missing data in a dataset?
Missing data is a common problem in datasets. The approach to handling it depends on the type of missingness (missing completely at random (MCAR), missing at random (MAR), or missing not at random (MNAR)) and the extent of missing data. Inappropriate handling can bias results.
- Deletion Methods: Listwise deletion removes any observation with missing data; pairwise deletion uses available data for each analysis. These methods are simple but can lead to significant loss of information and bias if data isn’t MCAR.
- Imputation Methods: These methods fill in missing values with predicted values. Common techniques include mean/median/mode imputation (simple but can distort the distribution), regression imputation (predicts missing values based on other variables), multiple imputation (creates multiple plausible imputed datasets, which is more robust and accounts for uncertainty), and k-nearest neighbor imputation. Careful consideration is needed as imputation also assumes a mechanism for the missing data and can introduce bias if the model isn’t correct.
- Model-Based Approaches: Some statistical methods, like maximum likelihood estimation (MLE) for certain models, can incorporate missing data directly without imputation.
The best approach often involves a combination of methods and careful consideration of the missing data mechanism and the potential impact on the analysis.
Q 5. Explain the concept of confounding and how to control for it.
Confounding occurs when a third variable influences both the exposure (independent variable) and the outcome (dependent variable), creating a spurious association between them. For example, if we observe a positive correlation between coffee consumption and heart disease, it may not be because coffee causes heart disease. It could be that smoking (confounder) is associated with both coffee consumption (smokers might be more likely to drink coffee) and heart disease (smoking increases heart disease risk).
To control for confounding:
- Randomization: In randomized controlled trials, randomly assigning participants to treatment and control groups helps to balance confounders across groups.
- Stratification: Analyze the association separately within strata of the confounder (e.g., analyze the coffee-heart disease relationship separately for smokers and non-smokers).
- Regression Analysis: Include the confounder as a covariate in a regression model to adjust for its effect. This statistically controls for the confounder’s influence on both exposure and outcome.
- Matching: Select control participants who are similar to the exposed participants on the confounder, minimizing confounding’s influence.
Failing to control for confounding can lead to inaccurate conclusions about the true relationship between exposure and outcome.
Q 6. What are different types of bias in epidemiological studies?
Epidemiological studies are susceptible to various biases, which can distort the results and lead to incorrect conclusions. Some key biases include:
- Selection bias: Systematic error in selecting participants for the study, such as non-response bias (people who don’t participate differ from those who do), healthy worker effect (workers tend to be healthier than the general population), or referral bias (patients referred to specialists are different than those not referred).
- Information bias: Systematic error in measuring exposure or outcome, such as recall bias (participants have inaccurate memories of past exposures), interviewer bias (interviewer influences responses), or misclassification bias (incorrect categorization of exposure or outcome).
- Confounding bias: As explained earlier, this occurs when a third variable influences both the exposure and the outcome, creating a spurious association.
- Publication bias: Studies with positive or significant results are more likely to be published, leading to an overestimation of the effect size in published literature.
Careful study design, data collection methods, and statistical analysis are crucial for minimizing these biases.
Q 7. Explain the difference between incidence and prevalence.
Incidence and prevalence are both measures of disease frequency, but they represent different aspects:
- Incidence: The rate of new cases of a disease occurring in a population during a specific time period. It is expressed as the number of new cases per person-time at risk (e.g., cases per 1000 person-years). It measures the risk of developing the disease. Imagine the number of people newly diagnosed with a disease over the next 5 years.
- Prevalence: The proportion of a population that has a disease at a specific point in time (point prevalence) or during a specified time period (period prevalence). It is expressed as a percentage or proportion (e.g., 10% of the population has the disease). It reflects the burden of the disease in the population. This represents the number of people currently living with the disease at a particular time.
Example: Imagine 100 people in a town. In one year, 10 people develop a new flu (incidence rate: 10 new cases per 100 people or 10%). At the end of the year, 20 people have the flu (including some from the previous year). Prevalence rate: 20 cases out of 100 people or 20%.
Both incidence and prevalence are important measures for understanding disease patterns and planning public health interventions.
Q 8. Describe different measures of central tendency and their uses.
Measures of central tendency describe the typical or central value of a dataset. The most common are the mean, median, and mode.
Mean: This is the average, calculated by summing all values and dividing by the number of values. It’s sensitive to outliers (extreme values). For example, the mean income in a neighborhood might be skewed upward by a few very high earners.
Median: This is the middle value when the data is ordered. It’s less sensitive to outliers than the mean. Imagine calculating the median house price – this is more representative than the mean if there are a few exceptionally expensive mansions.
Mode: This is the most frequent value. It’s useful for categorical data. For example, the mode color of cars in a parking lot might be blue.
The choice of measure depends on the data distribution and the research question. If the data is normally distributed (bell-shaped curve), the mean is often appropriate. However, if the data is skewed or has outliers, the median might be a better representation of the central tendency.
Q 9. What is a p-value, and how is it interpreted?
The p-value is the probability of obtaining results as extreme as, or more extreme than, the observed results, assuming the null hypothesis is true. The null hypothesis is a statement of no effect or no difference. A small p-value (typically less than 0.05) suggests that the observed results are unlikely to have occurred by chance alone, providing evidence against the null hypothesis. We might reject the null hypothesis in favor of the alternative hypothesis (which suggests an effect or difference).
Interpretation:
p < 0.05: Statistically significant. The results are unlikely due to chance. We reject the null hypothesis.
p ≥ 0.05: Not statistically significant. The results could be due to chance. We fail to reject the null hypothesis. (This does *not* mean we accept the null hypothesis).
It’s crucial to remember that a statistically significant result doesn’t necessarily imply practical significance. A small p-value might be obtained with a very large sample size, even if the effect size is tiny and irrelevant in practice.
Q 10. Explain Type I and Type II errors.
Type I and Type II errors are errors in hypothesis testing. They are related to the decision of whether to reject the null hypothesis.
Type I Error (False Positive): This occurs when we reject the null hypothesis when it is actually true. We conclude there’s an effect when there isn’t one. The probability of committing a Type I error is denoted by α (alpha), often set at 0.05. Think of this as a false alarm; a medical test indicating a disease when the person is actually healthy.
Type II Error (False Negative): This occurs when we fail to reject the null hypothesis when it is actually false. We conclude there’s no effect when there actually is one. The probability of committing a Type II error is denoted by β (beta). The power of a test (1-β) represents the probability of correctly rejecting a false null hypothesis. A missed diagnosis in medical testing is a classic example.
The balance between these errors is important. Reducing the risk of one type of error often increases the risk of the other.
Q 11. What is a confidence interval, and how is it calculated?
A confidence interval (CI) is a range of values that is likely to contain the true population parameter with a certain level of confidence. For example, a 95% confidence interval for the average height of women means that if we were to repeat the study many times, 95% of the calculated confidence intervals would contain the true average height.
Calculation: The calculation varies depending on the parameter being estimated. A common example is the confidence interval for the population mean. For a large sample size, the formula is approximately:
CI = sample mean ± (critical value) * (standard error)
where:
The sample mean is the average of the sample data.
The critical value is obtained from a standard normal distribution (z-distribution) or a t-distribution (for smaller sample sizes) based on the desired confidence level (e.g., 1.96 for a 95% CI using a z-distribution).
The standard error is the standard deviation of the sample mean, calculated as the sample standard deviation divided by the square root of the sample size.
The width of the confidence interval reflects the precision of the estimate. A narrower interval indicates a more precise estimate.
Q 12. How do you assess the goodness of fit of a statistical model?
Assessing the goodness of fit determines how well a statistical model fits a dataset. Several methods exist, depending on the type of model.
For regression models: R-squared, adjusted R-squared, and residual plots are commonly used. R-squared measures the proportion of variance in the dependent variable explained by the model. Adjusted R-squared penalizes the inclusion of unnecessary predictors. Residual plots help identify patterns or heteroscedasticity (unequal variance of residuals) suggesting a poor fit.
For categorical data models (e.g., chi-squared test): The chi-squared statistic assesses the difference between observed and expected frequencies. A large chi-squared value indicates a poor fit.
For probability distributions: Goodness-of-fit tests like the Kolmogorov-Smirnov test or the Anderson-Darling test compare the observed data distribution to a theoretical distribution (e.g., normal distribution).
In all cases, a good model fit implies that the model accurately captures the underlying data-generating process. Poor fit suggests the need for model refinement or selection of a different model.
Q 13. Explain different methods for hypothesis testing.
Hypothesis testing involves evaluating evidence from data to determine whether to reject a null hypothesis. Several methods exist, depending on the data type and research question.
t-test: Compares the means of two groups. There are different types, including independent samples t-test (comparing means of two independent groups) and paired samples t-test (comparing means of the same group at two different time points).
ANOVA (Analysis of Variance): Compares the means of three or more groups. It determines if there are significant differences between the group means.
Chi-squared test: Analyzes the association between categorical variables. It compares observed frequencies with expected frequencies under the null hypothesis of no association.
Non-parametric tests: These tests are used when the data doesn’t meet the assumptions of parametric tests (e.g., normality, equal variances). Examples include the Mann-Whitney U test (analogous to the independent samples t-test) and the Wilcoxon signed-rank test (analogous to the paired samples t-test).
The choice of method depends on the research question, the type of data, and the assumptions about the data distribution.
Q 14. What is logistic regression and when is it used?
Logistic regression is a statistical method used to model the probability of a binary outcome (0 or 1, success or failure) based on one or more predictor variables. Unlike linear regression which predicts a continuous outcome, logistic regression predicts the probability of an event occurring.
When it’s used:
Predicting the probability of disease: Predicting the likelihood of developing heart disease based on risk factors like age, smoking status, and cholesterol levels.
Credit risk assessment: Assessing the probability of loan default based on credit history, income, and other factors.
Marketing analysis: Predicting the probability of a customer making a purchase based on demographics and past behavior.
The model uses a logistic function to transform the linear combination of predictor variables into a probability score between 0 and 1. The output is interpreted as the probability of the event occurring.
Q 15. Explain the concept of odds ratio and relative risk.
Both odds ratio (OR) and relative risk (RR) are measures of association between an exposure and an outcome, often used in epidemiological studies. However, they differ in their calculation and interpretation.
Odds Ratio (OR): The OR represents the odds of an event occurring in one group compared to the odds of it occurring in another group. It’s calculated from a 2×2 contingency table:
OR = (a/b) / (c/d) = ad/bc
where:a = number of exposed individuals with the outcomeb = number of exposed individuals without the outcomec = number of unexposed individuals with the outcomed = number of unexposed individuals without the outcome
The OR is particularly useful in case-control studies, where the prevalence of the outcome is not known. An OR of 2, for example, suggests that the odds of the outcome are twice as high in the exposed group compared to the unexposed group.
Relative Risk (RR): The RR represents the risk of an event occurring in one group compared to the risk of it occurring in another group. It’s calculated as:
RR = (a/(a+b)) / (c/(c+d))
where the variables are the same as in the OR calculation.
The RR is used primarily in cohort studies, where the incidence of the outcome can be calculated. An RR of 2 indicates that the risk of the outcome is twice as high in the exposed group compared to the unexposed group.
Key Difference: The OR estimates the ratio of *odds*, while the RR estimates the ratio of *probabilities* or *risks*. In situations with a low probability of the outcome, the OR and RR will provide similar results. However, with higher outcome probabilities, the OR can overestimate the RR.
Example: Imagine a study comparing smoking and lung cancer. The OR might tell us that smokers have, say, 10 times the *odds* of developing lung cancer compared to non-smokers. The RR might tell us that smokers have, say, 8 times the *risk* of developing lung cancer. While both suggest a strong association, the interpretation differs slightly due to the inherent differences in the calculations.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Describe different survival analysis techniques.
Survival analysis techniques are statistical methods used to analyze the time until an event occurs. In medical research, this event is often death, but it could also be disease recurrence, recovery, or any other time-to-event endpoint. Several techniques exist:
- Kaplan-Meier method: This is a non-parametric method that estimates the survival function by calculating the probability of surviving past a certain time point. It accounts for censoring, where the event of interest hasn’t occurred for some individuals by the end of the study. It’s widely used for its simplicity and interpretability, producing a Kaplan-Meier curve.
- Cox proportional hazards model: This is a semi-parametric regression model used to investigate the relationship between multiple covariates and survival time. It assumes that the hazard ratio – the instantaneous risk of the event – is constant over time for each covariate. This is a powerful method for understanding how different factors influence survival.
- Accelerated failure time (AFT) models: These models assume that covariates affect the survival time multiplicatively. They are useful when the proportional hazards assumption of the Cox model is violated.
- Parametric survival models: These models assume a specific distribution for the survival time, such as exponential, Weibull, or log-normal. They can be more efficient than non-parametric methods if the assumed distribution is appropriate. However, incorrect distributional assumptions can lead to biased results.
The choice of method depends on the research question, the nature of the data (including censoring), and the assumptions one is willing to make. For instance, Kaplan-Meier is excellent for descriptive survival analysis, while Cox proportional hazards is better suited for exploring the impact of multiple factors.
Q 17. What are the key characteristics of a randomized controlled trial (RCT)?
A randomized controlled trial (RCT) is the gold standard in experimental research, particularly in evaluating the effectiveness of interventions. Its key characteristics include:
- Randomization: Participants are randomly assigned to either an intervention group (receiving the treatment) or a control group (receiving a placebo or standard care). This minimizes bias and helps ensure that any observed differences between groups are due to the intervention and not pre-existing differences.
- Control group: A comparison group is essential to assess the effectiveness of the intervention. The control group receives either a placebo, standard care, or no intervention.
- Blinding (masking): Ideally, both the participants and the researchers assessing the outcomes should be unaware of the treatment assignment. This prevents bias in both treatment adherence and outcome assessment. Single-blinding (participants unaware) and double-blinding (both participants and researchers unaware) are possible.
- Predefined outcomes: Specific, measurable outcomes are defined in advance, ensuring objectivity and reducing the risk of bias during analysis.
- Sample size calculation: The study should be adequately powered to detect a clinically meaningful difference between the intervention and control groups. A sample size calculation determines the minimum number of participants needed to achieve sufficient statistical power.
The strict design of an RCT minimizes confounding factors, thereby increasing the internal validity and strengthening causal inferences. However, RCTs can be expensive, time-consuming, and sometimes not feasible for ethical or practical reasons.
Q 18. How do you interpret a Kaplan-Meier curve?
A Kaplan-Meier curve is a graphical representation of the survival function, showing the probability of surviving beyond a certain time point. The x-axis represents time, and the y-axis represents the proportion of individuals who survived.
Interpretation:
- Step-wise decline: The curve typically decreases in a step-wise fashion. Each step down represents an event (e.g., death) occurring at that time point.
- Censoring: The curve does not necessarily reach zero. Horizontal lines indicate censored observations (individuals who are still alive or have been lost to follow-up at the end of the study). Censored data is incorporated into the calculation but not counted as an event.
- Comparison of groups: Multiple Kaplan-Meier curves can be plotted on the same graph to compare survival experiences between different groups (e.g., treatment vs. control). A curve that remains higher at any given time point indicates better survival for that group.
- Log-rank test: A statistical test, like the log-rank test, is commonly used to formally compare the survival curves between groups, determining if the difference is statistically significant.
Example: A Kaplan-Meier curve could show the survival probability of cancer patients after a particular treatment. If the treatment group’s curve stays above the control group’s curve throughout the study period, it suggests that the treatment improves survival.
Q 19. Explain the difference between prospective and retrospective studies.
Prospective and retrospective studies differ primarily in their timing relative to the event of interest.
Prospective studies: These studies follow participants forward in time from a defined starting point to observe the occurrence of the outcome. The exposure status is determined at the beginning of the study and the outcome is observed later. They are generally considered stronger in terms of establishing causality because they reduce the risk of recall bias and minimize confounding. An example would be following a group of smokers and non-smokers over 20 years to see who develops lung cancer.
Retrospective studies: These studies examine past events. Data on both exposure and outcome are collected from the past, often using existing records (e.g., medical records, databases). They are typically quicker and less expensive than prospective studies but are more susceptible to bias, particularly recall bias (participants may not accurately recall past exposures) and selection bias (the sample may not be representative of the population of interest). An example would be reviewing hospital records to see if there is a relationship between prior antibiotic use and the development of a specific infection.
In Summary:
- Prospective: Forward-looking, stronger evidence for causality, more expensive and time-consuming.
- Retrospective: Backward-looking, cheaper and faster, higher risk of bias.
Q 20. What are the ethical considerations in epidemiological research?
Ethical considerations in epidemiological research are paramount. Key aspects include:
- Informed consent: Participants must be fully informed about the study’s purpose, procedures, potential risks and benefits, and their right to withdraw at any time. Consent must be voluntary and obtained before participation.
- Confidentiality and privacy: Researchers must protect the privacy and confidentiality of participants’ data. Data should be anonymized or de-identified whenever possible, and appropriate security measures should be in place.
- Beneficence and non-maleficence: The research should maximize benefits and minimize harms to participants. Risks should be carefully assessed and mitigated.
- Justice and equity: The benefits and burdens of the research should be fairly distributed. Vulnerable populations should be protected from exploitation.
- Institutional review board (IRB) approval: All research involving human subjects must be reviewed and approved by an IRB to ensure ethical conduct.
- Data integrity and transparency: Researchers have an ethical obligation to ensure the accuracy and integrity of their data and to report their findings honestly and transparently, including limitations.
Ethical breaches can have serious consequences, potentially harming participants and eroding public trust in research. Adherence to ethical guidelines is crucial for conducting responsible and meaningful epidemiological studies.
Q 21. How do you handle outliers in your data?
Outliers – data points that significantly deviate from the rest of the data – can unduly influence the results of statistical analyses. Handling outliers requires careful consideration and depends on the nature of the data and the cause of the outlier.
Strategies for handling outliers:
- Identify outliers: Use visual methods (e.g., box plots, scatter plots) and statistical methods (e.g., Z-scores, interquartile range) to identify potential outliers. Consider both univariate and multivariate outliers.
- Investigate the cause: Before removing or transforming outliers, investigate why they exist. Are they errors in data entry? Do they represent a genuinely extreme value? Are they due to a different underlying population?
- Data correction: If the outlier is due to a data entry error or measurement error, correct the error if possible. If the outlier arises from a genuine biological or clinical phenomenon, consider other appropriate techniques.
- Robust statistical methods: Use robust statistical methods that are less sensitive to outliers. Robust methods include non-parametric methods (e.g., median, interquartile range instead of mean, standard deviation) or regression methods that are less sensitive to outlying values.
- Transformation: Log transformations or other data transformations can sometimes reduce the influence of outliers.
- Winsorizing or trimming: Replacing extreme values with less extreme values (Winsorizing) or removing a certain percentage of extreme values (trimming) can reduce the impact of outliers.
- Sensitivity analysis: Perform analyses both with and without the outliers to assess their impact on the results.
The decision of how to handle outliers should be justified and transparently reported. Arbitrary removal of outliers without investigation can lead to bias and misinterpretation of the results.
Q 22. What statistical software packages are you proficient in?
I’m proficient in several statistical software packages, each with its own strengths. R is my primary tool; its flexibility and extensive libraries (like ggplot2 for visualization and dplyr for data manipulation) are invaluable for complex analyses. I also have considerable experience with Python, particularly using libraries such as pandas, scikit-learn, and statsmodels. These offer excellent capabilities for data processing, machine learning, and statistical modeling. Finally, I’m familiar with SAS, a robust and widely used package particularly strong in clinical trials and large-scale data analysis. My choice of software depends on the specific project requirements and the nature of the data.
Q 23. Describe a time you had to explain complex statistical results to a non-technical audience.
During a project investigating the effectiveness of a new public health intervention, I needed to present the results to a community board with limited statistical backgrounds. The analysis involved logistic regression, yielding odds ratios and confidence intervals. Instead of focusing on the technical details, I used a clear analogy: imagine a coin flip. A fair coin has a 50/50 chance of heads or tails (odds ratio of 1). Our intervention shifted this, making the chance of a positive outcome (e.g., improved health status) more likely, like flipping a weighted coin. The odds ratio quantifies how much more likely the positive outcome is with the intervention. Confidence intervals illustrate how certain we are about this effect. Visual aids, such as bar charts displaying the percentage changes and clear explanations in plain language helped to ensure that everyone could understand the key findings and their implications.
Q 24. Explain your experience with data cleaning and preprocessing.
Data cleaning and preprocessing are crucial steps before any meaningful analysis can take place. My experience encompasses a range of techniques. I routinely check for missing data, employing various imputation methods like mean/median imputation or more sophisticated techniques like k-nearest neighbors, depending on the data’s characteristics and the amount of missing data. I carefully examine data for outliers, using methods like boxplots and scatter plots to identify and handle them – sometimes by removing them, other times by transforming the data (e.g., using logarithmic transformation). I also frequently check for inconsistencies in data entry (e.g., misspellings, incorrect data types) and correct them using string manipulation techniques or data validation rules. For example, in a recent study involving survey data, I identified and corrected inconsistencies in age reporting by cross-referencing with other available information. The overall goal is to produce a clean, consistent dataset that accurately reflects the underlying reality.
Q 25. What is your experience with meta-analysis?
I have extensive experience with meta-analysis, a powerful technique for combining results from multiple studies investigating the same research question. This allows for a more precise estimate of the overall effect size and increased statistical power. My experience includes conducting meta-analyses using both fixed-effects and random-effects models, selecting appropriate effect size measures (e.g., odds ratios, standardized mean differences), assessing heterogeneity among studies using I2 and Cochran’s Q test, and addressing publication bias using techniques like funnel plots and Egger’s test. I understand the importance of careful study selection and quality assessment, ensuring only relevant and high-quality studies are included in the analysis. For instance, in a recent project on the effectiveness of a particular medication, I synthesized results from several clinical trials, quantifying the overall effectiveness and identifying potential sources of heterogeneity in the results.
Q 26. Describe your understanding of Bayesian methods.
Bayesian methods offer a powerful alternative to frequentist approaches. Instead of estimating parameters based solely on observed data, Bayesian inference incorporates prior knowledge about the parameters through prior distributions. This allows for more informative inference, particularly when data are limited. I’m experienced in using Markov Chain Monte Carlo (MCMC) methods, such as Gibbs sampling and Metropolis-Hastings, to estimate posterior distributions. I understand the importance of choosing appropriate prior distributions and assessing convergence of MCMC chains. For example, in analyzing a rare disease outbreak, Bayesian methods allowed for incorporating prior information about disease prevalence from similar outbreaks, leading to more accurate estimates of the current outbreak’s parameters, even with a relatively small sample size.
Q 27. How do you choose an appropriate statistical test for a given research question?
Selecting the appropriate statistical test depends on several factors, including the type of data (continuous, categorical, ordinal), the research question (comparing means, assessing association, etc.), and the study design. My approach involves a systematic process: first, I clearly define the research question and the hypotheses. Then, I identify the type of data and the study design (e.g., independent samples t-test for comparing means between two independent groups, paired t-test for comparing means between two related groups, ANOVA for comparing means among three or more groups, chi-square test for assessing association between categorical variables, linear regression for examining the relationship between a continuous outcome and one or more predictors). Finally, I assess the assumptions of the chosen test (e.g., normality, homogeneity of variance) and select an alternative test if the assumptions are violated. For instance, if comparing the effectiveness of two different treatments, with continuous outcome data and meeting assumptions of normality and equal variance, an independent samples t-test would be appropriate.
Q 28. Explain your experience working with large datasets.
I have considerable experience working with large datasets, leveraging techniques to manage and analyze them efficiently. This includes employing database management systems (like SQL) to extract and manipulate large amounts of data, using parallel computing techniques to speed up analyses, and utilizing data reduction techniques (e.g., dimensionality reduction methods like principal component analysis) to handle high-dimensional data. I’m familiar with cloud computing platforms such as AWS and Google Cloud for storage and processing of massive datasets. For example, in a recent public health surveillance project, I worked with a dataset containing millions of records. I used SQL queries to extract relevant information, employed parallel processing to run complex models, and implemented data visualization techniques to efficiently summarize and present the results in a meaningful way.
Key Topics to Learn for Statistical and Epidemiological Analysis Interview
- Descriptive Statistics: Understanding measures of central tendency, variability, and distribution. Practical application: Summarizing and presenting key findings from epidemiological studies.
- Inferential Statistics: Hypothesis testing, confidence intervals, and p-values. Practical application: Determining the statistical significance of associations between risk factors and disease outcomes.
- Regression Analysis: Linear, logistic, and Poisson regression models. Practical application: Modeling the relationship between exposures and health outcomes, predicting disease risk.
- Study Design: Familiarization with different study designs (cohort, case-control, cross-sectional, randomized controlled trials). Practical application: Critically evaluating the strengths and limitations of epidemiological studies.
- Epidemiological Measures: Incidence, prevalence, mortality rates, relative risk, odds ratio. Practical application: Interpreting and calculating key epidemiological measures to assess disease burden and risk factors.
- Bias and Confounding: Identifying and mitigating biases in epidemiological studies. Practical application: Ensuring the validity and reliability of study results.
- Data Visualization: Creating clear and informative graphs and charts to communicate findings. Practical application: Effectively presenting complex data to both technical and non-technical audiences.
- Statistical Software: Proficiency in at least one statistical software package (e.g., R, SAS, STATA). Practical application: Conducting statistical analyses and generating reports.
- Causal Inference: Understanding concepts of causality and methods for assessing causal relationships. Practical application: Drawing meaningful conclusions from observational data.
- Survival Analysis: Analyzing time-to-event data. Practical application: Studying the progression of diseases and the effectiveness of interventions.
Next Steps
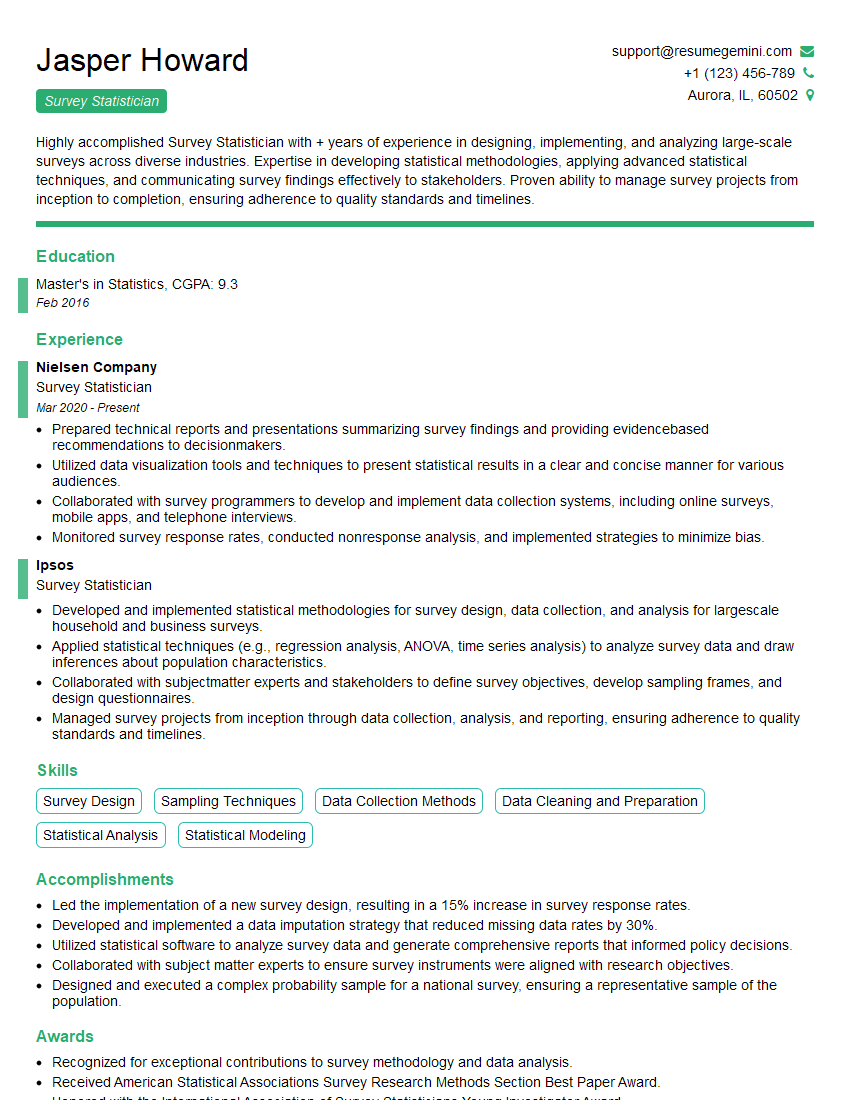
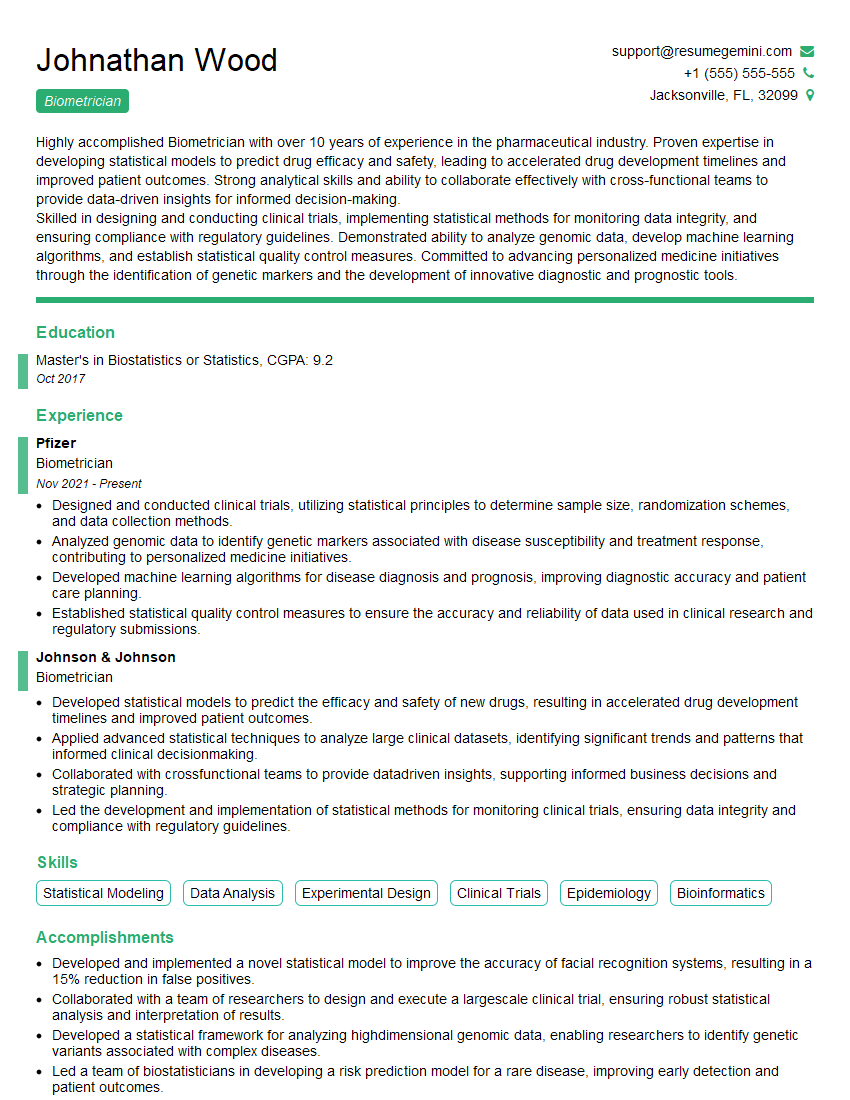
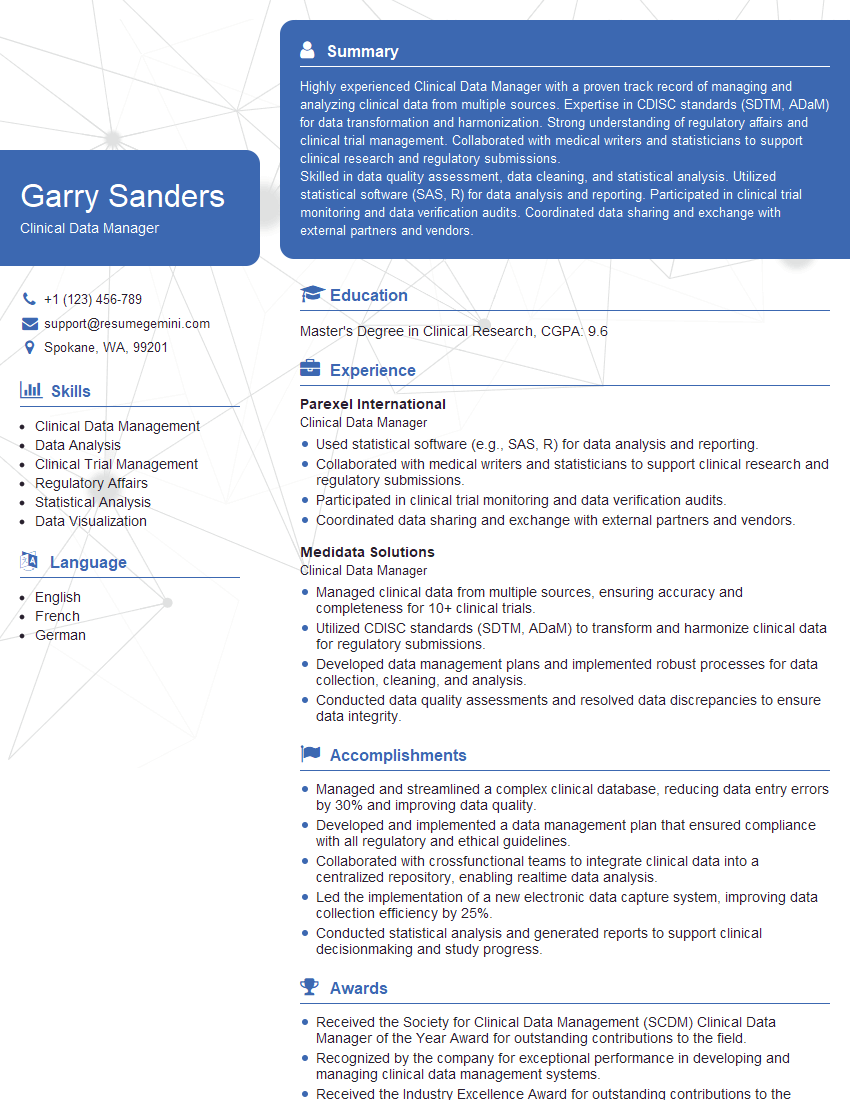
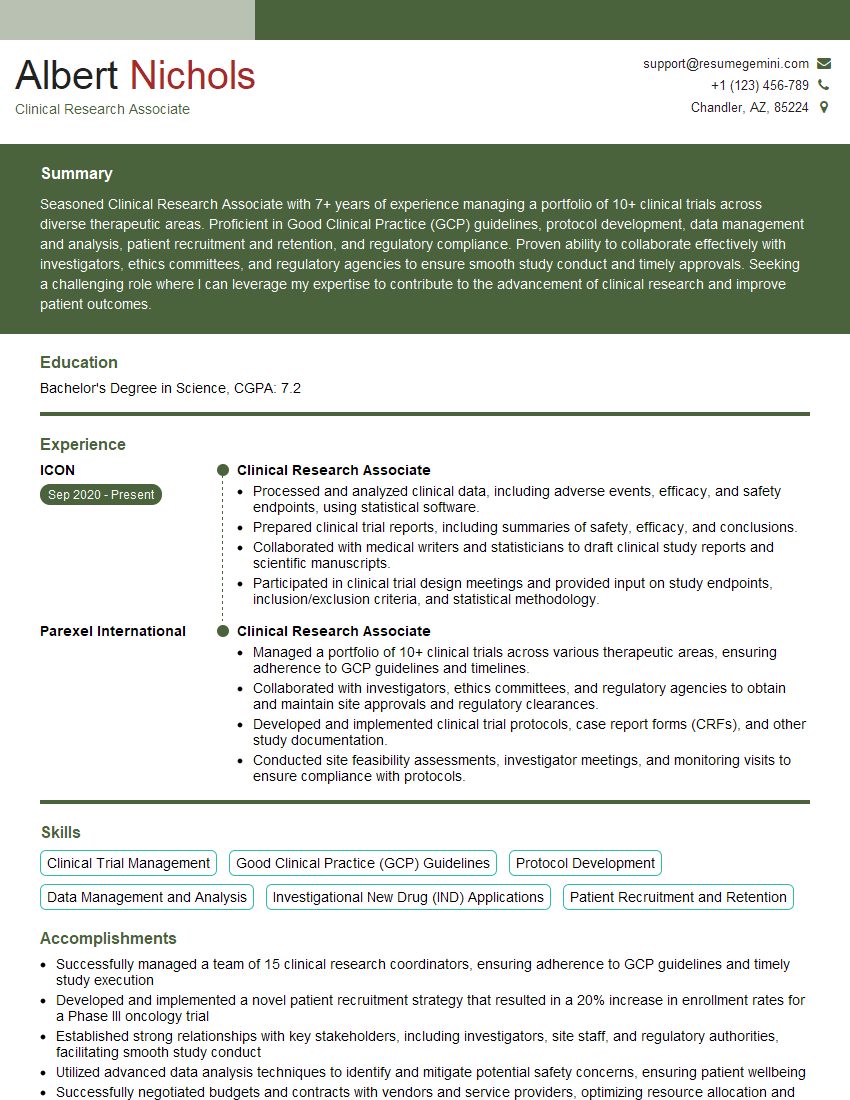
Mastering Statistical and Epidemiological Analysis is crucial for career advancement in public health, research, and data science. A strong understanding of these methods opens doors to exciting opportunities and allows you to contribute meaningfully to improving population health. To maximize your job prospects, creating an ATS-friendly resume is vital. ResumeGemini is a trusted resource that can help you build a compelling and effective resume, highlighting your skills and experience. Examples of resumes tailored to Statistical and Epidemiological Analysis are available to guide you through the process.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
hello,
Our consultant firm based in the USA and our client are interested in your products.
Could you provide your company brochure and respond from your official email id (if different from the current in use), so i can send you the client’s requirement.
Payment before production.
I await your answer.
Regards,
MrSmith
hello,
Our consultant firm based in the USA and our client are interested in your products.
Could you provide your company brochure and respond from your official email id (if different from the current in use), so i can send you the client’s requirement.
Payment before production.
I await your answer.
Regards,
MrSmith
These apartments are so amazing, posting them online would break the algorithm.
https://bit.ly/Lovely2BedsApartmentHudsonYards
Reach out at [email protected] and let’s get started!
Take a look at this stunning 2-bedroom apartment perfectly situated NYC’s coveted Hudson Yards!
https://bit.ly/Lovely2BedsApartmentHudsonYards
Live Rent Free!
https://bit.ly/LiveRentFREE
Interesting Article, I liked the depth of knowledge you’ve shared.
Helpful, thanks for sharing.
Hi, I represent a social media marketing agency and liked your blog
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?