The thought of an interview can be nerve-wracking, but the right preparation can make all the difference. Explore this comprehensive guide to Prostate Surgery interview questions and gain the confidence you need to showcase your abilities and secure the role.
Questions Asked in Prostate Surgery Interview
Q 1. Describe the different surgical approaches for prostate cancer (e.g., radical prostatectomy, brachytherapy, HIFU).
Prostate cancer treatment involves several surgical approaches, each with its own set of advantages and disadvantages. The primary options include radical prostatectomy, brachytherapy, and high-intensity focused ultrasound (HIFU).
Radical Prostatectomy: This involves the complete surgical removal of the prostate gland, seminal vesicles, and sometimes a portion of the surrounding tissue. It’s a definitive treatment aiming for a cure.
Brachytherapy: This is a form of radiation therapy where radioactive seeds or implants are placed directly into the prostate gland. It’s less invasive than radical prostatectomy but requires precise placement of the radioactive seeds.
High-Intensity Focused Ultrasound (HIFU): This uses focused ultrasound waves to destroy cancerous tissue within the prostate. It’s a minimally invasive procedure, but its effectiveness might be less compared to radical prostatectomy or brachytherapy, especially in advanced stages.
Q 2. Explain the indications and contraindications for each approach.
The choice of surgical approach depends heavily on individual factors like the patient’s overall health, the stage and grade of the cancer, and the patient’s preferences.
Radical Prostatectomy Indications: Localized prostate cancer, good overall health, patient preference for definitive surgery.
Contraindications: Significant comorbidities (heart, lung disease), inability to tolerate surgery, advanced metastatic disease.
Brachytherapy Indications: Localized prostate cancer, low to intermediate risk, patient preference for minimally invasive treatment.
Contraindications: Prior pelvic radiation, significant comorbidities preventing effective treatment, highly aggressive cancers.
HIFU Indications: Localized prostate cancer, low risk, patients who are poor surgical candidates, preference for minimally invasive therapy.
Contraindications: Extensive extracapsular extension, seminal vesicle invasion, significant comorbidities, large prostate size.
Q 3. Compare and contrast open, laparoscopic, and robotic-assisted radical prostatectomy.
Radical prostatectomy can be performed through three main approaches: open, laparoscopic, and robotic-assisted.
Open Radical Prostatectomy: This traditional approach involves a larger incision in the abdomen. It allows for excellent visualization and manipulation of tissues, resulting in potentially better nerve-sparing and cancer control. However, it’s associated with longer recovery times and larger scars.
Laparoscopic Radical Prostatectomy: This minimally invasive technique uses smaller incisions and specialized instruments to perform the surgery. It leads to less pain, shorter hospital stays, and smaller scars compared to open surgery. However, the learning curve is steeper, and the 3D visualization can be less intuitive than open surgery.
Robotic-Assisted Radical Prostatectomy (RARP): This combines laparoscopy with robotic technology. The surgeon controls robotic arms, allowing for greater precision, dexterity, and magnified visualization. RARP offers many of the advantages of laparoscopy, with potentially better outcomes in experienced hands. It may require more advanced training and specialized equipment.
Essentially, the choice depends on surgeon expertise, available resources, and patient suitability. Many surgeons find robotic surgery to offer the best combination of minimally invasive features and precision, especially for nerve-sparing procedures.
Q 4. What are the potential complications associated with radical prostatectomy?
Radical prostatectomy, while effective, carries potential complications. These include:
- Bleeding: This can range from minor to life-threatening. Careful surgical technique and meticulous haemostasis are essential.
- Infection: Wound infections, urinary tract infections, and sepsis are possibilities. Prophylactic antibiotics are often used.
- Urinary Incontinence: Damage to the urinary sphincter can lead to temporary or permanent incontinence. This is a major concern, and nerve-sparing techniques aim to minimize this risk.
- Erectile Dysfunction: Damage to the nerves responsible for erectile function can cause ED. Nerve-sparing techniques are crucial here too.
- Lymphocele: A collection of lymph fluid near the surgical site. This can be managed conservatively or may require drainage.
- Rectal Injury: Although rare, injury to the rectum is a serious complication.
- DVT/PE: Deep vein thrombosis (DVT) and pulmonary embolism (PE) are possibilities, and preventative measures are implemented.
Q 5. How do you manage postoperative complications like bleeding, infection, or incontinence?
Postoperative complications require prompt and effective management. Strategies include:
Bleeding: Close monitoring of vital signs, blood transfusions if necessary, and occasionally surgical intervention to control bleeding points.
Infection: Broad-spectrum antibiotics are administered, along with wound care and potentially surgical debridement.
Incontinence: This can be managed with pelvic floor exercises, medication (e.g., alpha-blockers), and in some cases, surgical procedures such as artificial urinary sphincter placement.
A multidisciplinary approach, involving urologists, nurses, physiotherapists, and other specialists, is crucial for optimal management of postoperative complications. Close follow-up is essential to identify and address any problems promptly.
Q 6. Discuss the nerve-sparing techniques used during radical prostatectomy.
Nerve-sparing techniques during radical prostatectomy aim to preserve the neurovascular bundles responsible for erectile function. These bundles lie on either side of the prostate. The surgeon carefully dissects around these bundles, attempting to remove the prostate while leaving the nerves intact. The extent of nerve-sparing depends on several factors, including the location and extent of the cancer, the surgeon’s experience and the patient’s preference.
There are variations in nerve-sparing approaches. Some surgeons perform unilateral nerve sparing (preserving nerves on one side only), while others attempt bilateral nerve sparing (preserving nerves on both sides). The decision is highly individualized.
Q 7. What are the different methods for assessing nerve sparing success?
Assessing nerve-sparing success involves a combination of methods:
Early Postoperative Assessment: This involves regular monitoring of erectile function through questionnaires and clinical examinations. However, early recovery may not reflect the long-term outcome.
Long-Term Follow-up: The patient’s erectile function is routinely evaluated using validated questionnaires (e.g., the International Index of Erectile Function, IIEF) over several years. This provides a more accurate assessment of long-term success.
Electrophysiological Studies: These can be performed intraoperatively or postoperatively to assess the integrity of the nerves. These are less commonly used in routine practice.
It’s important to acknowledge that nerve-sparing success is not guaranteed, and the recovery time can vary significantly. Factors such as patient age, pre-operative erectile function, and the extent of surgery influence the outcome.
Q 8. Explain your approach to pre-operative patient counseling and risk assessment.
Pre-operative counseling for prostate cancer surgery is crucial. It’s a collaborative process where I thoroughly discuss the patient’s diagnosis, treatment options, potential benefits, and risks, ensuring they’re fully informed to make an educated decision. This involves a detailed review of their medical history, including any comorbidities like heart disease or diabetes, which could influence surgical planning and recovery. We also discuss the specifics of the procedure, including the potential for complications like incontinence or erectile dysfunction. Risk assessment is integral; I use validated risk calculators to estimate the likelihood of these complications, based on factors like age, PSA level, Gleason score, and the extent of the cancer. We then personalize this information, taking into account the patient’s individual goals and preferences. For instance, a younger patient may prioritize preserving sexual function more than an older patient. The conversation also extends to alternative treatments like active surveillance or radiation therapy, ensuring the patient understands the full range of choices.
For example, I recently counseled a 60-year-old patient with a relatively low-risk prostate cancer. While robotic surgery was an option, we discussed the potential for complications and the fact that active surveillance could be a viable alternative given his specific circumstances. Ultimately, he opted for robotic surgery after understanding the pros and cons of both approaches.
Q 9. Describe your experience with robotic surgery for prostate cancer.
I have extensive experience with robotic-assisted radical prostatectomy (RARP). I’ve performed hundreds of these procedures, consistently achieving excellent oncological and functional outcomes. Robotic surgery offers enhanced precision, dexterity, and visualization compared to open surgery, translating to potentially improved surgical outcomes. The minimally invasive nature of the procedure leads to less blood loss, shorter hospital stays, and faster recovery times. My experience includes managing various complexities, such as extensive extracapsular extension, seminal vesicle involvement, and positive surgical margins. I continuously update my skills by participating in advanced training and workshops focusing on robotic surgical techniques and technological advancements.
Q 10. How do you select appropriate patients for robotic-assisted procedures?
Patient selection for RARP is crucial. While it’s a minimally invasive technique, it’s not suitable for all patients. Ideal candidates are generally those with localized prostate cancer, a relatively healthy overall condition, and a realistic understanding of the procedure’s potential risks and benefits. Factors considered include age, overall health, BMI, co-morbidities like diabetes or heart disease, PSA level, Gleason score, tumor stage and size, and patient preference. Patients with significant comorbidities or those who are not suitable for general anesthesia may be better suited for alternative treatments like radiation therapy. I always involve the patient in this decision-making process to ensure their comfort and compliance with the treatment plan.
For example, patients with a very high BMI might have challenges with positioning during robotic surgery. Similarly, those with significant cardiovascular problems might face higher surgical risks. Careful evaluation ensures we tailor the approach to individual needs.
Q 11. Explain your surgical technique for robotic-assisted radical prostatectomy.
My surgical technique for RARP involves a meticulous, step-wise approach. Beginning with a small incision, I use the da Vinci surgical system to carefully dissect the prostate from surrounding tissues. Nerve-sparing techniques are employed whenever feasible, aiming to preserve sexual function. Lymphadenectomy (removal of lymph nodes) is performed if clinically indicated. Precise dissection minimizes bleeding and injury to adjacent structures. The specimen is carefully removed, and meticulous hemostasis (control of bleeding) is crucial. The bladder neck and urethra are reconstructed to ensure urinary continence. The entire procedure is guided by real-time visualization and enhanced dexterity provided by the robotic arms.
Post-operative management includes careful monitoring of vital signs, pain control, and bladder catheter management. Early mobilization and physiotherapy aid in a swift recovery.
Q 12. What are the advantages and disadvantages of using robotic surgery for prostate cancer?
Robotic surgery for prostate cancer offers several advantages. These include smaller incisions, less pain, less blood loss, shorter hospital stays, faster recovery, and potentially better cosmetic results compared to open surgery. The enhanced visualization and precision of the robotic system may also lead to improved nerve-sparing and better oncological outcomes in experienced hands. However, there are also disadvantages. The procedure is more expensive than open surgery. It requires specialized equipment and highly trained surgeons. While complications are less frequent than with open surgery, they can still occur, including urinary incontinence, erectile dysfunction, and infection. The learning curve for robotic surgery is steep, requiring significant training and experience for optimal results.
Q 13. How do you manage patients with positive surgical margins after radical prostatectomy?
Positive surgical margins (PSM) after radical prostatectomy indicate that cancer cells remain at the edge of the resected tissue. This requires careful management. The first step involves a thorough pathology review to confirm the extent of PSM involvement. We then discuss the patient’s overall health and preferences to determine the best course of action. Options include active surveillance (close monitoring), adjuvant radiation therapy (radiation therapy after surgery), or salvage surgery (a second operation). The decision is personalized based on factors like patient age, overall health, PSM extent, Gleason score, and the presence of other risk factors. The goal is to minimize the risk of recurrence while preserving quality of life.
For instance, a patient with a small, low-risk PSM might be best managed with active surveillance, while a patient with a larger, high-risk PSM might benefit from adjuvant radiation therapy.
Q 14. Discuss the role of adjuvant radiation therapy in prostate cancer treatment.
Adjuvant radiation therapy plays a significant role in managing prostate cancer after surgery, particularly in cases of high-risk disease or positive surgical margins. It aims to eradicate any remaining microscopic cancer cells, reducing the risk of recurrence and improving long-term survival rates. The type and dosage of radiation therapy are carefully tailored based on the individual patient’s characteristics, including the stage of cancer, Gleason score, and presence of risk factors. Adjuvant radiation therapy can be delivered using external beam radiation therapy (EBRT) or brachytherapy (internal radiation therapy). The decision to use adjuvant radiation therapy is made on a case-by-case basis, considering factors like patient age, overall health, and potential side effects of radiation. The benefits of improved survival rates must be weighed against the potential side effects, such as bowel or bladder problems.
Q 15. What are the different types of radiation therapy used for prostate cancer?
Radiation therapy plays a crucial role in prostate cancer treatment, and several types are available, each with its own strengths and weaknesses. The choice depends on factors like tumor stage, overall health, and patient preferences.
- External Beam Radiation Therapy (EBRT): This is the most common type, using a machine outside the body to deliver high-energy radiation beams to the prostate. It’s often administered in daily fractions over several weeks. Intensity-modulated radiation therapy (IMRT) and volumetric modulated arc therapy (VMAT) are advanced forms of EBRT that allow for more precise targeting of the tumor, minimizing damage to surrounding healthy tissues.
- Brachytherapy: This involves placing radioactive seeds or implants directly into the prostate gland. This delivers a high dose of radiation directly to the tumor while sparing surrounding tissues. There are two main types: low-dose rate (LDR) brachytherapy, which uses lower-intensity seeds over a longer period, and high-dose rate (HDR) brachytherapy, which uses higher-intensity sources for shorter periods.
- Proton Beam Therapy: This advanced form of radiation therapy uses protons instead of photons, offering greater precision and potentially reduced side effects. It’s particularly beneficial for patients with tumors close to critical organs like the rectum and bladder.
- Combined Modality Therapy: Often, radiation therapy is combined with other treatments like hormone therapy or surgery to optimize outcomes. For instance, combining EBRT with hormone therapy is a standard approach for locally advanced prostate cancer.
Choosing the appropriate radiation therapy method requires careful consideration of the patient’s individual circumstances and a multidisciplinary approach involving the urologist, radiation oncologist, and other specialists.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Explain your approach to managing urinary incontinence after radical prostatectomy.
Managing urinary incontinence after radical prostatectomy is a critical aspect of post-operative care. It’s important to remember that this is a common side effect, and many effective strategies exist to minimize and manage it.
My approach begins with a thorough assessment of the patient’s urinary function before and after surgery, including bladder scans and voiding diaries. We discuss realistic expectations, explaining that recovery takes time and the level of incontinence varies.
- Conservative Management: Initially, we focus on conservative measures such as pelvic floor muscle exercises (Kegels), bladder training, and lifestyle modifications (avoiding caffeine and alcohol).
- Pharmacological Interventions: Medications like anticholinergics can help manage urinary urgency and frequency.
- Absorbent Products: Patients may temporarily require absorbent pads or protective underwear to manage incontinence.
- Surgical Intervention: In cases of persistent or severe incontinence that don’t respond to conservative treatments, surgical procedures like a sling procedure or artificial urinary sphincter may be considered.
Regular follow-up appointments are crucial to monitor progress and adjust management strategies as needed. Open communication and patient education are key components of effective post-operative care.
For example, I recently had a patient who experienced moderate incontinence after surgery. Through a combination of Kegel exercises, bladder training, and medication, he significantly improved within three months, and he no longer required pads after six months. Every patient’s journey is unique, but with the right approach, most experience significant improvement.
Q 17. Discuss the methods used to manage erectile dysfunction after radical prostatectomy.
Erectile dysfunction (ED) is another common side effect after radical prostatectomy due to nerve damage near the prostate. However, various options exist to help men regain sexual function.
My approach is multifaceted and begins with open and honest communication about the potential for ED and the management options available. This helps manage expectations and encourages proactive engagement in treatment.
- Watchful Waiting: For some men, sexual function may spontaneously return over time. We often recommend a period of watchful waiting before considering other interventions.
- Phosphodiesterase-5 Inhibitors (PDE5i): Medications like sildenafil (Viagra), tadalafil (Cialis), and vardenafil (Levitra) are often the first-line treatment. These help improve blood flow to the penis.
- Alprostadil: This medication can be injected directly into the penis or administered as a urethral suppository to induce an erection.
- Vacuum Erection Devices (VEDs): These devices create a vacuum around the penis to draw blood into it and achieve an erection.
- Penile Implants: In cases where other treatments fail, a penile implant may be considered as a last resort. This is a surgical procedure that involves inserting inflatable or malleable implants into the penis.
- Testosterone Replacement Therapy: Low testosterone levels can contribute to ED. In appropriate cases, testosterone replacement may be beneficial.
We encourage patients to discuss their sexual health concerns openly and involve their partners in the decision-making process. The goal is to find a management strategy that improves their quality of life.
Q 18. How do you assess and manage patients with advanced prostate cancer?
Managing advanced prostate cancer requires a comprehensive and multidisciplinary approach. The treatment strategy depends on various factors, including the stage of the cancer, the patient’s overall health, and their preferences.
Assessment involves a thorough review of the patient’s medical history, physical examination, imaging studies (CT scan, bone scan, MRI), and biopsy results. Blood tests, such as PSA levels, help monitor disease progression.
- Hormone Therapy (Androgen Deprivation Therapy or ADT): This is a cornerstone of advanced prostate cancer treatment, aiming to reduce testosterone levels, which fuel the growth of prostate cancer cells. It can be administered through medication or surgery (orchiectomy).
- Chemotherapy: Chemotherapy drugs are used to kill cancer cells and may be employed when hormone therapy is no longer effective.
- Targeted Therapy: These newer medications target specific molecules involved in cancer cell growth and survival. They may be used in combination with other treatments.
- Immunotherapy: Immunotherapy harnesses the body’s immune system to fight cancer cells. It’s becoming increasingly important in advanced prostate cancer management.
- Radiation Therapy: Radiation therapy may be used to relieve symptoms, reduce tumor size, or improve quality of life in specific situations.
Regular monitoring of PSA levels and imaging studies is crucial to track the effectiveness of treatment and detect any disease progression. Palliative care is also essential to manage symptoms and improve quality of life throughout the treatment process.
Q 19. Discuss your familiarity with prostate cancer staging and grading.
Prostate cancer staging and grading are essential for determining the extent and aggressiveness of the disease, guiding treatment decisions, and predicting prognosis.
Staging describes the size and spread of the cancer. The TNM system (Tumor, Node, Metastasis) is commonly used, with T indicating tumor size and invasiveness, N representing lymph node involvement, and M denoting the presence of distant metastases. For example, T2bN0M0 means a moderately sized tumor, no lymph node involvement, and no distant metastases.
Grading assesses the aggressiveness of the cancer cells under a microscope. The Gleason grading system is frequently used, assigning a score based on the appearance of the cancer cells. A higher Gleason score indicates more aggressive cancer.
Understanding both staging and grading allows for accurate risk stratification and tailored treatment plans. For instance, a patient with a high-stage and high-grade prostate cancer may require a more aggressive approach compared to a patient with a low-stage and low-grade cancer.
Q 20. What is your experience with different imaging modalities used in prostate cancer diagnosis (e.g., MRI, biopsy)?
Imaging modalities play a critical role in prostate cancer diagnosis and management. My experience encompasses a range of techniques.
- Transrectal Ultrasound (TRUS): This is routinely used to guide prostate biopsies. A probe is inserted into the rectum to visualize the prostate and obtain tissue samples.
- Magnetic Resonance Imaging (MRI): MRI provides detailed images of the prostate, helping to identify suspicious areas and guide targeted biopsies. Multiparametric MRI (mpMRI), incorporating different imaging sequences, is particularly useful in detecting clinically significant cancer.
- Computed Tomography (CT) Scan: CT scans are used to assess the extent of the disease, particularly to evaluate for lymph node involvement or distant metastases.
- Bone Scan: A bone scan is used to detect metastasis to the bones, a common site of spread for advanced prostate cancer.
The choice of imaging technique depends on the clinical scenario. For example, mpMRI is increasingly used to guide targeted biopsies, reducing the number of biopsies required and improving diagnostic accuracy. CT scans and bone scans are typically used in staging advanced disease.
Q 21. Explain your understanding of the role of PSA in prostate cancer management.
Prostate-specific antigen (PSA) is a protein produced by the prostate gland. While PSA levels can be elevated in prostate cancer, it’s important to remember that elevated PSA can also be caused by benign prostatic hyperplasia (BPH) or other prostate conditions. Therefore, PSA alone is not definitive for diagnosing prostate cancer.
In prostate cancer management, PSA levels are primarily used for:
- Screening: PSA testing, along with a digital rectal exam, is used as part of screening for prostate cancer in men, typically starting at age 50 or earlier for high-risk individuals. However, the benefits and harms of PSA screening are still debated.
- Diagnosis: An elevated PSA level might prompt further investigation, such as a prostate biopsy.
- Monitoring: After treatment, PSA levels are monitored to assess the effectiveness of treatment and detect any recurrence of the cancer. A rising PSA level after treatment usually indicates cancer recurrence.
It’s crucial to interpret PSA levels in conjunction with other clinical findings and imaging results. It is just one piece of the puzzle in the complex process of managing prostate cancer.
Q 22. Describe your approach to managing patients with prostate cancer recurrence.
Managing prostate cancer recurrence requires a systematic approach tailored to the individual patient and the specifics of their recurrence. This begins with a thorough evaluation, including PSA levels, imaging studies (bone scan, CT, MRI), and potentially a biopsy to confirm the location and extent of the recurrence. The management strategy depends heavily on several factors: the time since initial treatment, the location of the recurrence (local, regional lymph nodes, or distant metastasis), and the patient’s overall health and preferences.
For example, a patient with a localized recurrence after radical prostatectomy might be a candidate for salvage radiation therapy, or even a secondary surgical procedure if feasible. If the recurrence involves regional lymph nodes, consideration might be given to androgen deprivation therapy (ADT) alone or in combination with radiation. For patients with distant metastases, systemic therapies such as hormone therapy (ADT), chemotherapy, or novel targeted agents become the primary treatment options. Regular monitoring with PSA testing and imaging is crucial to assess treatment response and guide further management decisions. It’s a dynamic process, and treatment strategies may need to be adjusted based on the patient’s response over time.
Q 23. How do you utilize multidisciplinary approaches to manage complex prostate cancer cases?
Complex prostate cancer cases often require a multidisciplinary approach, bringing together the expertise of various specialists. This typically includes a urologic oncologist (myself), a radiation oncologist, a medical oncologist, a pathologist, and potentially other specialists like a radiologist or a nuclear medicine physician. This collaborative approach allows for a comprehensive evaluation of the patient’s condition and the development of a personalized treatment plan that considers all aspects of their disease. We use regular tumor boards to discuss complex cases, where each specialist contributes their perspective, facilitating a shared decision-making process between the team and the patient.
For instance, a patient with locally advanced prostate cancer might benefit from a combined approach involving radical prostatectomy followed by adjuvant radiation therapy. The radiation oncologist would help determine the optimal radiation technique and dose, while I would focus on the surgical aspects. Similarly, the medical oncologist plays a vital role in managing hormonal therapies before, during, and after surgery to reduce the risk of recurrence and improve survival rates. The pathologist provides essential information regarding tumor characteristics, which greatly influences treatment strategy.
Q 24. Discuss your understanding of current research trends in prostate cancer treatment.
Current research in prostate cancer treatment focuses on several exciting areas. One significant trend is the development of novel targeted therapies that specifically attack cancer cells while minimizing damage to healthy tissues. This includes therapies targeting specific genetic mutations or pathways involved in prostate cancer development. Another area of active research is in developing more precise and effective radiation techniques, such as proton therapy, which can deliver higher doses of radiation to the tumor while sparing surrounding healthy organs. Furthermore, significant progress is being made in identifying biomarkers that can help predict a patient’s risk of recurrence and guide treatment decisions. Research on liquid biopsies, which analyze circulating tumor DNA, offers the potential for early detection and monitoring of recurrence, reducing the need for invasive biopsies. Finally, advancements in robotic surgery and minimally invasive techniques are enhancing surgical precision and reducing patient morbidity.
Q 25. What are your professional development goals within the field of prostate surgery?
My professional development goals center around enhancing my expertise in minimally invasive surgical techniques for prostate cancer, specifically robotic-assisted laparoscopic prostatectomy (RALP) and its application in complex cases. I plan to continue expanding my knowledge of advanced imaging techniques and their integration into surgical planning. This includes focusing on techniques that improve patient outcomes, such as reducing complications, improving continence and potency rates, and minimizing hospital stays. Furthermore, I am dedicated to expanding my understanding of emerging targeted therapies and integrating them into my treatment strategies for patients with recurrent or metastatic disease. Staying abreast of the latest research and collaborating with other experts through participation in professional conferences and research studies are integral to my continuous learning and professional growth. Ultimately, my goal is to provide the most innovative and effective prostate cancer care to my patients.
Q 26. Describe your experience with managing prostate cancer in diverse patient populations.
My experience encompasses managing prostate cancer across diverse patient populations, considering factors such as age, ethnicity, socioeconomic status, and comorbidities. I recognize that these factors can significantly influence a patient’s ability to tolerate treatment, their adherence to treatment plans, and ultimately, their outcomes. For instance, older patients with multiple comorbidities might require a more conservative approach, whereas younger patients may tolerate more intensive treatments. Furthermore, cultural and socioeconomic factors can impact a patient’s understanding and engagement with their treatment plan, necessitating a sensitive and patient-centered approach to communication and education. I believe in providing culturally competent care, tailoring my communication style to each individual’s needs and preferences, and ensuring that all patients have access to the information and support they need to make informed decisions about their health.
Q 27. How do you stay current with advancements in prostate cancer surgical techniques and technology?
Staying current with advancements in prostate cancer surgical techniques and technology requires a multi-faceted approach. I actively participate in professional organizations such as the American Urological Association (AUA) and attend national and international conferences and workshops focused on prostate surgery. This allows me to directly engage with leading experts, learn about the newest techniques and technologies firsthand, and participate in discussions surrounding best practices. I also dedicate time to reviewing peer-reviewed medical literature, including journals such as the Journal of Urology and European Urology. Furthermore, I actively participate in continuing medical education courses and surgical simulation training to refine my skills and stay updated on technological advancements. Maintaining strong relationships with colleagues in the field and participating in collaborative research projects also contribute significantly to staying at the forefront of advancements.
Q 28. What is your approach to informed consent and patient autonomy in prostate cancer surgery?
Informed consent and patient autonomy are paramount in my approach to prostate cancer surgery. Before any surgical procedure, I dedicate significant time to educating patients about their diagnosis, the various treatment options, the risks and benefits associated with each option, including surgery, as well as potential complications. This includes discussions about potential side effects such as urinary incontinence, erectile dysfunction, and bowel dysfunction. I present the information in a clear, concise, and understandable manner, using visuals and analogies whenever necessary to ensure the patient fully grasps the information. I encourage patients to ask questions and actively involve their family members or support systems in the decision-making process. My goal is to empower patients to make fully informed decisions based on their individual values, preferences, and circumstances, ensuring their autonomy is respected throughout the entire process. This collaborative approach strengthens the physician-patient relationship and contributes to better patient outcomes and satisfaction.
Key Topics to Learn for Prostate Surgery Interview
- Anatomy and Physiology of the Prostate: Deep understanding of prostate anatomy, its relationship to surrounding structures, and the physiological processes involved in prostate function.
- Types of Prostate Surgery: Comprehensive knowledge of different surgical techniques (e.g., radical prostatectomy – open, laparoscopic, robotic; minimally invasive approaches; laser ablation) including their indications, contraindications, and comparative advantages/disadvantages.
- Surgical Planning and Preoperative Assessment: Mastering the process of patient selection, preoperative imaging interpretation (MRI, CT, ultrasound), biopsy analysis, and risk stratification.
- Intraoperative Techniques and Management: Detailed knowledge of surgical steps, handling complications (e.g., bleeding, nerve injury), and use of advanced surgical technologies (e.g., robotic systems, nerve-sparing techniques).
- Postoperative Care and Complications: Understanding potential complications (e.g., urinary incontinence, erectile dysfunction), postoperative pain management strategies, and long-term follow-up care.
- Oncological Principles in Prostate Cancer Surgery: Knowledge of cancer biology, staging systems, lymph node dissection techniques, and principles of oncologic surgery to achieve optimal cancer control.
- Evidence-Based Practice and Current Research: Staying abreast of the latest research, clinical trials, and guidelines influencing prostate surgery practice.
- Ethical Considerations and Informed Consent: Understanding the ethical implications of surgical decision-making and the importance of obtaining informed consent from patients.
Next Steps
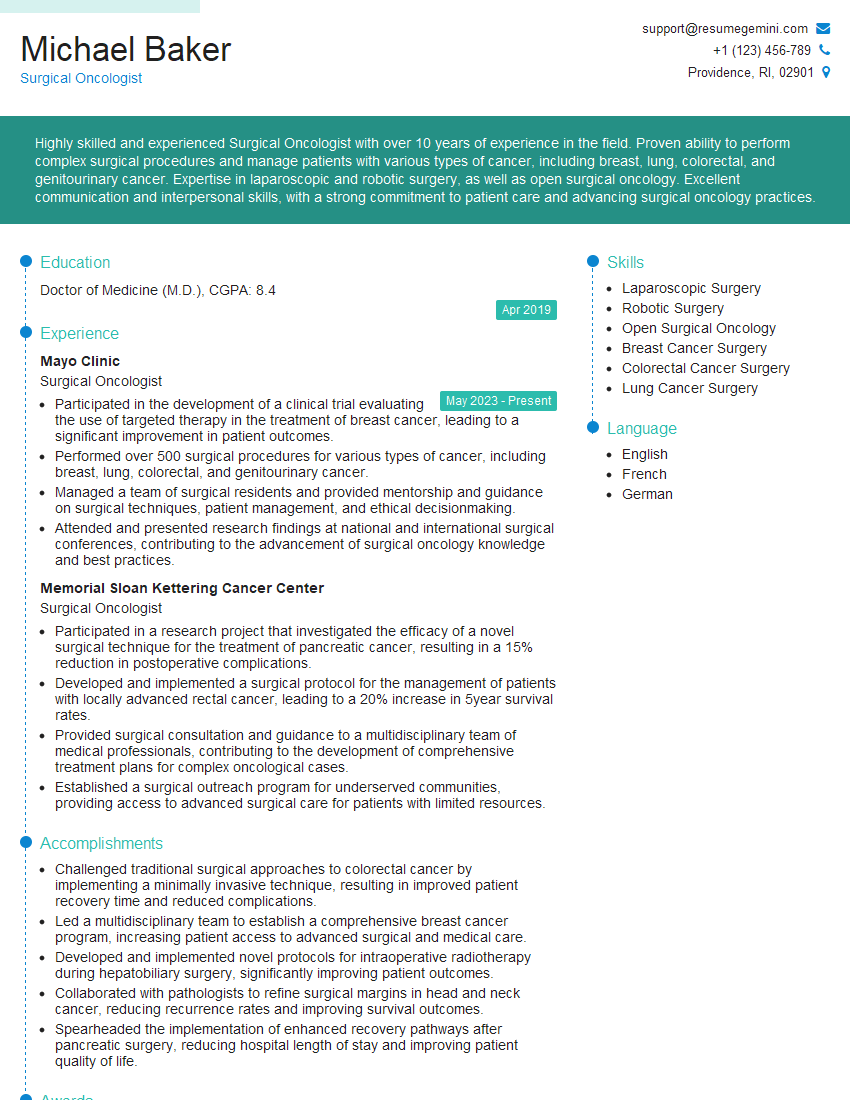
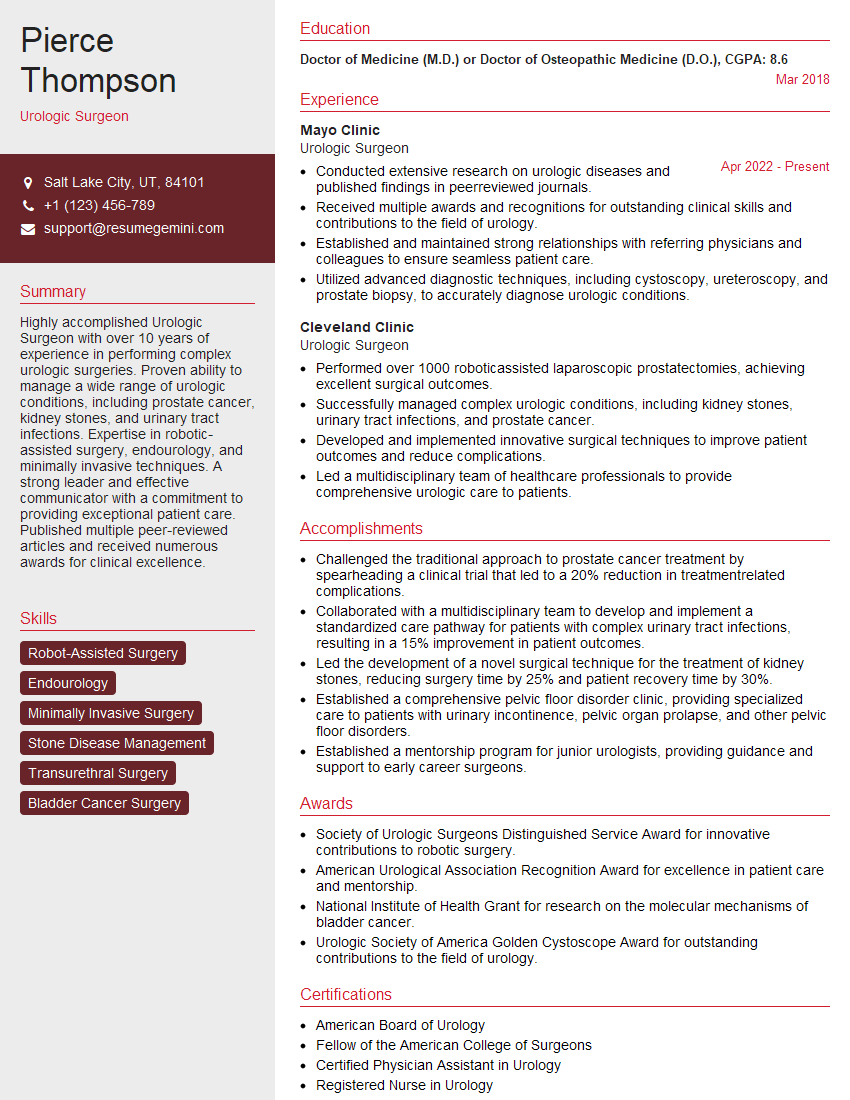
Mastering prostate surgery techniques and principles is crucial for career advancement in urology. A strong foundation in this area will significantly enhance your competitiveness in the job market. To maximize your job prospects, it’s vital to present your skills and experience effectively. Creating an ATS-friendly resume is essential in ensuring your application gets noticed by recruiters and hiring managers. ResumeGemini is a trusted resource to help you build a professional and impactful resume that showcases your expertise. Examples of resumes tailored specifically for Prostate Surgery specialists are available to guide you. Invest time in crafting a compelling resume to unlock your career potential.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Take a look at this stunning 2-bedroom apartment perfectly situated NYC’s coveted Hudson Yards!
https://bit.ly/Lovely2BedsApartmentHudsonYards
Live Rent Free!
https://bit.ly/LiveRentFREE
Interesting Article, I liked the depth of knowledge you’ve shared.
Helpful, thanks for sharing.
Hi, I represent a social media marketing agency and liked your blog
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?