Preparation is the key to success in any interview. In this post, we’ll explore crucial Adolescent Mental Health interview questions and equip you with strategies to craft impactful answers. Whether you’re a beginner or a pro, these tips will elevate your preparation.
Questions Asked in Adolescent Mental Health Interview
Q 1. Describe your experience working with adolescents experiencing anxiety disorders.
My experience working with adolescents experiencing anxiety disorders centers around a holistic approach combining therapeutic interventions with collaborative family support. I’ve worked extensively with teens presenting with generalized anxiety disorder, social anxiety disorder, panic disorder, and separation anxiety. A crucial element is building a strong therapeutic alliance, creating a safe space where they feel comfortable sharing their fears and worries.
For example, I recently worked with a 15-year-old girl struggling with intense social anxiety. We started with Cognitive Behavioral Therapy (CBT), focusing on identifying and challenging her negative automatic thoughts about social situations. Simultaneously, we incorporated relaxation techniques like deep breathing and progressive muscle relaxation to manage her physical symptoms of anxiety. We also involved her parents in sessions to better understand the family dynamics and provide consistent support at home.
Beyond CBT, I find incorporating mindfulness and exposure therapy, gradually introducing her to feared social situations, to be particularly effective. The progress was slow but steady; we celebrated small victories, building her confidence and self-efficacy. This approach highlights the importance of individualizing treatment and focusing on sustainable coping mechanisms rather than quick fixes.
Q 2. Explain your approach to treating adolescent depression.
My approach to treating adolescent depression is multifaceted and emphasizes a collaborative, person-centered approach. It’s critical to understand the context of their depression—academic pressures, social issues, family conflicts, or potential underlying medical conditions—to tailor an effective treatment plan.
This often involves a combination of evidence-based therapies such as Cognitive Behavioral Therapy (CBT) to help identify and change negative thinking patterns and behavioral activation to increase engagement in enjoyable activities. I also integrate interpersonal psychotherapy (IPT) which focuses on improving relationships, as relational issues are frequently intertwined with depression in adolescents.
For instance, I worked with a 17-year-old boy who was withdrawn and experiencing significant depressive symptoms after a breakup. We used CBT to address his negative self-talk and IPT to help him navigate the challenges of his relationship loss and develop healthier communication skills. We also explored his interests and encouraged him to re-engage in activities he once enjoyed, a key element of behavioral activation. Medication might be considered in severe cases, always in conjunction with therapy and with careful monitoring of side effects.
Q 3. How do you assess suicidal ideation in adolescent patients?
Assessing suicidal ideation in adolescents requires a sensitive and direct approach. It’s crucial to create a safe and trusting environment where the adolescent feels comfortable sharing their thoughts and feelings without judgment. The assessment isn’t just about asking if they have thoughts of suicide, but also exploring the intensity, frequency, and plans associated with those thoughts.
I use a combination of methods, including direct questioning (“Have you been having thoughts of hurting or killing yourself?”), standardized assessment tools (like the Suicide Risk Assessment Scale), and open-ended questions to understand the underlying reasons for their suicidal ideation, including hopelessness, impulsivity, and access to lethal means. I also assess their support systems, coping mechanisms, and history of previous suicide attempts.
It’s vital to remember that any expression of suicidal ideation, regardless of severity, requires immediate attention and a thorough safety plan. This might involve hospitalization, involving family members, and developing strategies to manage triggers and improve their overall well-being. Collaboration with a multidisciplinary team, involving psychiatrists, school counselors and family is often essential.
Q 4. What are the key developmental considerations when treating adolescents?
Developmental considerations are paramount when treating adolescents. Their brains are still developing, particularly the prefrontal cortex responsible for executive functioning, emotional regulation, and decision-making. This impacts their ability to understand and process information, manage emotions, and engage in therapeutic interventions.
Therefore, my approach considers their developmental stage, including their cognitive abilities, emotional maturity, and social context. For example, I might use different therapeutic techniques with a 13-year-old compared to a 17-year-old, adapting the language, explanations, and level of engagement to their developmental needs.
Furthermore, I acknowledge the influence of their peer relationships, family dynamics, and school environment. Addressing these contextual factors is crucial for effective treatment. This might involve family therapy, school liaison work or community support services.
Q 5. Describe your experience with evidence-based therapies for adolescents.
My work extensively utilizes evidence-based therapies proven effective for adolescents. These include:
- Cognitive Behavioral Therapy (CBT): This therapy helps adolescents identify and modify negative thoughts and behaviors contributing to their mental health challenges. It’s highly effective for anxiety, depression, and other mood disorders.
- Dialectical Behavior Therapy (DBT): DBT is particularly helpful for adolescents with emotional dysregulation, self-harm behaviors, and borderline personality traits. It emphasizes mindfulness, distress tolerance, and interpersonal effectiveness skills.
- Acceptance and Commitment Therapy (ACT): ACT focuses on accepting difficult emotions and thoughts, and committing to actions aligned with their values. This approach is useful for adolescents struggling with anxiety, depression, and trauma.
I regularly review the latest research and adjust my therapeutic strategies based on emerging evidence and the unique needs of each adolescent. The selection of therapy is always carefully considered based on the individual’s specific diagnosis, presenting problems, and personal preferences.
Q 6. How do you handle confidentiality issues with adolescent patients?
Confidentiality is crucial when working with adolescents. However, there are exceptions to confidentiality, primarily when there is a risk of harm to themselves or others.
I explain this carefully to adolescents and their parents at the outset of therapy, clarifying the limits of confidentiality. I emphasize that I will maintain confidentiality to the greatest extent possible while also explaining the circumstances under which I might be legally obligated to break confidentiality (e.g., if they disclose plans to harm themselves or others, or if there is evidence of abuse or neglect).
For example, if an adolescent discloses plans for self-harm, I will take immediate action, which may involve informing their parents, seeking consultation with colleagues, or recommending hospitalization. Transparency and open communication are crucial to building trust and ensuring the adolescent feels safe and supported throughout the process.
Q 7. Explain your approach to working with families of adolescent patients.
My approach to working with families involves collaboration and a systemic perspective. I believe that understanding the family system, including the adolescent’s relationships with parents, siblings, and other family members, is essential for effective treatment. I don’t view the adolescent as isolated from their family environment but rather as part of a complex interconnected system.
My approach emphasizes empowering families to understand and address the issues contributing to the adolescent’s difficulties. This might involve family therapy sessions, where we discuss communication patterns, family roles, and coping strategies. I work to foster a collaborative relationship between the adolescent and their family, promoting open communication and mutual support.
For example, if a family struggles with conflict resolution, I might teach them problem-solving skills or conflict-resolution techniques. In situations where parental conflict significantly impacts the adolescent, I might encourage individual sessions for parents alongside adolescent therapy to address these issues. This multi-pronged strategy leads to lasting, sustainable change.
Q 8. How do you identify and address trauma in adolescents?
Identifying and addressing trauma in adolescents requires a sensitive and multifaceted approach. It begins with careful assessment, looking beyond the immediate presenting problem. We use a variety of methods, including trauma-informed questionnaires like the Child Trauma Questionnaire (CTQ), and open-ended conversations. It’s crucial to create a safe and trusting therapeutic environment where the adolescent feels comfortable disclosing their experiences. The key is to listen without judgment and validate their feelings.
Once trauma is suspected, we might use evidence-based therapies like Trauma-Focused Cognitive Behavioral Therapy (TF-CBT) or Eye Movement Desensitization and Reprocessing (EMDR). TF-CBT helps adolescents understand the connection between their thoughts, feelings, and behaviors, while EMDR uses bilateral stimulation to process traumatic memories. The treatment plan is always individualized, considering the adolescent’s age, developmental stage, and the specific type and severity of trauma. For example, a teenager who experienced a car accident might benefit from TF-CBT to manage anxiety and PTSD symptoms, while another who experienced chronic neglect might need a longer-term approach incorporating attachment-based therapies.
It’s vital to collaborate with the adolescent’s family, school, and other relevant systems whenever possible and appropriate, ensuring a holistic approach to support their healing and recovery. A critical aspect is addressing the potential impact of trauma on various areas of their life, such as their relationships, academic performance, and physical health.
Q 9. What are some common risk factors for mental health issues in adolescents?
Several factors can increase the risk of mental health issues in adolescents. These can be broadly categorized into individual, family, peer, and societal factors. Individual risk factors include genetic predisposition, temperament, and pre-existing medical conditions. For instance, a family history of depression significantly increases an adolescent’s risk of developing depression. Similarly, a difficult temperament or a pre-existing condition like ADHD can impact mental well-being.
- Family Factors: These include family conflict, parental mental illness, substance abuse within the family, and insecure attachment patterns. A home environment characterized by constant fighting or parental substance abuse can create significant stress and contribute to mental health challenges.
- Peer Factors: Bullying, peer pressure, social isolation, and lack of social support are important considerations. Being bullied or excluded can significantly impact an adolescent’s self-esteem and mental health.
- Societal Factors: Poverty, discrimination, violence exposure, and lack of access to healthcare all play a role. Living in poverty or experiencing discrimination can significantly increase stress and vulnerability.
It’s important to remember that these risk factors often interact and are not isolated entities. For example, a genetically predisposed individual living in poverty and experiencing bullying is at a much higher risk of developing mental health problems than someone without these risk factors.
Q 10. How do you differentiate between normal adolescent behavior and clinical symptoms?
Differentiating between typical adolescent behavior and clinical symptoms requires careful observation and consideration of several factors. Adolescence is a period of significant developmental change marked by mood swings, risk-taking behaviors, and identity exploration. These are normal developmental processes.
However, when these behaviors become persistent, severe, or significantly impair the adolescent’s functioning in daily life (school, relationships, self-care), it may indicate a clinical problem. For example, occasional sadness is normal; persistent, overwhelming sadness that interferes with daily activities may suggest depression. Similarly, occasional rebellious behavior is common, but consistent defiance and disregard for rules and consequences could be indicative of a conduct disorder.
A comprehensive assessment, including interviews with the adolescent and their family, and psychological testing, helps distinguish between normal developmental fluctuations and clinically significant symptoms. Considering the duration, intensity, and impact of the symptoms on the adolescent’s life is crucial. Clinicians often use standardized diagnostic criteria, like those outlined in the DSM-5, to guide this process.
Q 11. Describe your experience with medication management for adolescent patients.
Medication management for adolescent patients is a complex process requiring careful consideration of developmental factors, potential side effects, and the adolescent’s individual needs. I always prioritize a collaborative approach, involving the adolescent, their parents (when appropriate and with the adolescent’s consent), and other healthcare professionals. The decision to prescribe medication should never be taken lightly and is made only after thorough assessment and consideration of non-pharmacological interventions.
For example, if an adolescent presents with symptoms of depression, we might first explore evidence-based psychotherapies like CBT or interpersonal therapy. If these interventions are not sufficient, we might consider adding medication, carefully selecting the type and dosage based on their age, weight, medical history, and response to treatment. Regular monitoring for side effects and treatment efficacy is essential. Open communication and shared decision-making with the adolescent and their family are crucial throughout this process.
Close collaboration with a psychiatrist specializing in adolescent mental health is essential, particularly given the potential for different medication responses and side effects in adolescents compared to adults.
Q 12. How do you work with adolescents who are resistant to treatment?
Working with adolescents resistant to treatment requires a nuanced and patient approach. The first step involves understanding the reasons behind their resistance. Is it due to fear, mistrust, lack of understanding of the benefits of treatment, or a preference for alternative coping mechanisms? Open and honest communication is crucial; creating a safe and non-judgmental space for them to express their concerns and reservations is vital.
Motivational interviewing techniques can be extremely effective. This involves exploring their ambivalence towards change and helping them identify their own reasons for wanting to improve. Engaging them in the decision-making process about their treatment plan and empowering them to take ownership of their care is crucial. Collaborative goal setting allows them to feel in control rather than feeling imposed upon. For example, rather than dictating a treatment plan, I might work with them to establish smaller, achievable goals, gradually building their confidence and motivation to engage more fully in therapy.
Flexibility in treatment approach is also key. If one approach is not effective, we explore alternative strategies. This might involve adjusting the therapeutic approach, incorporating family therapy, peer support groups, or creative interventions that resonate more effectively with the adolescent.
Q 13. What is your experience with crisis intervention for adolescents?
Crisis intervention for adolescents requires immediate and decisive action to ensure their safety and well-being. My experience involves assessing the level of risk, providing immediate support, and developing a safety plan. This often involves collaborating with emergency services, hospital staff, and family members. The initial focus is on stabilizing the situation, addressing immediate safety concerns, and providing emotional support.
For example, if an adolescent is experiencing suicidal ideation, a thorough risk assessment is crucial, exploring factors such as lethality of their plan, access to means, and level of hopelessness. If there’s an immediate risk of harm, hospitalization might be necessary. If not, we work collaboratively to develop a safety plan that includes strategies for managing distressing thoughts and feelings, identifying support systems, and developing coping mechanisms. Ongoing follow-up is crucial to prevent relapse and promote long-term mental wellness. Collaboration with schools, families, and other stakeholders is important to ensure a supportive environment following the crisis.
Q 14. How do you build rapport with adolescent patients?
Building rapport with adolescent patients is essential for effective treatment. It requires empathy, active listening, and a genuine interest in their lives. I begin by creating a safe and judgment-free space where they feel comfortable sharing their thoughts and feelings. I avoid using jargon, ensuring that communication is clear and easily understandable. I try to understand their perspective and validate their experiences, even if I don’t necessarily agree with their viewpoints.
I actively listen to their concerns and make an effort to understand their unique challenges. Finding common ground, such as shared interests or experiences, can help build connections. Being genuine and showing a sincere interest in their well-being helps foster trust. Using open-ended questions and encouraging them to express themselves in their own way allows for deeper engagement. The use of humor, appropriate to the situation, can also help to ease tension and build trust. It’s essential to respect their boundaries and allow them to lead the conversation at their own pace, remembering that they are navigating a complex stage of development.
Q 15. Describe your knowledge of the DSM-5 criteria for adolescent mental disorders.
The DSM-5 (Diagnostic and Statistical Manual of Mental Disorders, 5th Edition) provides a standardized classification system for mental disorders. Understanding its criteria for adolescents is crucial for accurate diagnosis and treatment planning. It’s important to remember that adolescence is a period of significant developmental change, and the manifestation of mental disorders can differ from adults. The DSM-5 doesn’t have a separate section for ‘adolescent disorders,’ but rather applies diagnostic criteria across the lifespan, considering developmental appropriateness. For example, while depression in an adult might manifest as persistent sadness and loss of interest, in an adolescent it might present as irritability, social withdrawal, or academic decline. Specific disorders relevant to adolescents include:
- Depressive Disorders: Major Depressive Disorder, Persistent Depressive Disorder (Dysthymia). Criteria focus on symptoms like depressed mood, loss of interest, changes in weight or sleep, fatigue, and feelings of worthlessness.
- Anxiety Disorders: Generalized Anxiety Disorder, Panic Disorder, Social Anxiety Disorder, Specific Phobias. These involve excessive fear and worry, impacting daily functioning.
- Attention-Deficit/Hyperactivity Disorder (ADHD): Characterized by inattention, hyperactivity, and impulsivity.
- Oppositional Defiant Disorder (ODD): A pattern of angry/irritable mood, argumentative/defiant behavior, or vindictiveness.
- Conduct Disorder (CD): A repetitive and persistent pattern of behavior that violates the basic rights of others or age-appropriate societal norms.
- Substance Use Disorders: Involve problematic patterns of substance use leading to clinically significant impairment or distress.
- Eating Disorders: Anorexia Nervosa, Bulimia Nervosa, Binge Eating Disorder. These are characterized by disturbances in eating behavior and body image.
Clinicians must carefully assess symptoms, rule out other conditions, and consider developmental context to make accurate diagnoses using the DSM-5 criteria. It’s vital to remember that these are just guidelines and clinical judgment plays a significant role.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you incorporate culturally sensitive practices into your therapy with adolescents?
Cultural sensitivity is paramount in adolescent mental health. Ignoring cultural factors can lead to misdiagnosis and ineffective treatment. My approach involves several key strategies:
- Cultural Humility: I acknowledge that I don’t possess all the knowledge about a client’s culture and commit to ongoing learning and self-reflection.
- Assessment: I begin by understanding the adolescent’s cultural background, family structure, values, beliefs, and spiritual practices. This includes asking open-ended questions about their life experiences and how their culture shapes their perspectives.
- Language and Communication: I ensure communication is clear and accessible, using interpreters if needed. I am mindful of nonverbal communication and adjust my style to be respectful and comfortable for the individual.
- Family Involvement: I actively involve the family, respecting their role and cultural norms regarding family dynamics. I adapt my therapeutic approach to be compatible with the family’s values and expectations.
- Treatment Adaptation: I consider culturally relevant factors when selecting and implementing interventions. For example, incorporating traditional healing practices if appropriate and ethically sound.
- Collaboration: I collaborate with other professionals who have expertise in the adolescent’s cultural background to ensure the best possible care.
For example, I had a client from a collectivist culture where family harmony was highly valued. Her depression was initially masked by her reluctance to express negative emotions openly. By understanding this cultural context, I adapted my approach to involve family therapy and focus on strengthening family relationships to support her recovery.
Q 17. What is your approach to working with adolescents from diverse backgrounds?
Working with adolescents from diverse backgrounds requires a multifaceted approach rooted in cultural competency. This involves understanding the intersectionality of various identities – race, ethnicity, gender, sexual orientation, socioeconomic status, religion, and disability – and how these factors can influence mental health experiences and help-seeking behaviors.
- Building Rapport: Establishing trust and rapport are crucial. This requires demonstrating genuine interest and respect for their experiences and perspectives. It often involves adapting my communication style to fit their comfort levels and preferences.
- Addressing Systemic Barriers: I acknowledge and address the systemic inequities that may contribute to mental health disparities within diverse communities. This includes recognizing and mitigating the impacts of racism, discrimination, and lack of access to resources.
- Culturally Adapted Interventions: Interventions should be tailored to meet the specific needs and preferences of each adolescent. This may involve modifying therapeutic techniques or incorporating elements of their culture to make therapy more relevant and engaging.
- Understanding Trauma: Many adolescents from marginalized communities have experienced historical and ongoing trauma. It’s important to create a safe and supportive therapeutic environment that acknowledges these experiences and fosters healing.
- Advocacy: I act as an advocate for my clients, working to remove barriers that impede their access to care and successful treatment outcomes.
For example, working with a refugee adolescent, I would need to understand their experiences of displacement and trauma, the cultural nuances of their communication style, and the potential impact of cultural loss on their mental well-being. This might involve collaborating with interpreters or organizations serving refugee populations.
Q 18. Explain your understanding of the impact of social media on adolescent mental health.
Social media’s impact on adolescent mental health is complex and multifaceted. While it can offer connection and support, it also presents significant risks.
- Cyberbullying: Exposure to cyberbullying can lead to anxiety, depression, and even suicidal ideation. The anonymity and widespread reach of online platforms amplify the harm.
- Social Comparison: Constant exposure to curated online profiles can fuel social comparison, leading to feelings of inadequacy, low self-esteem, and body image issues.
- Fear of Missing Out (FOMO): The pressure to be constantly connected and the perception of others’ seemingly perfect lives can trigger anxiety and depression.
- Addiction: Excessive social media use can become addictive, disrupting sleep, school performance, and relationships.
- Exposure to Harmful Content: Adolescents can be exposed to inappropriate content, including violence, hate speech, and pro-eating disorder or self-harm materials.
- Sleep Disturbances: The blue light emitted from screens can interfere with sleep patterns, further impacting mental well-being.
It’s crucial to have open conversations with adolescents about responsible social media use, promoting digital wellness and media literacy. Therapy can help adolescents manage their social media use, address negative comparisons, and build resilience to online pressures.
Q 19. How do you manage ethical dilemmas in adolescent mental health care?
Ethical dilemmas in adolescent mental health are common and require careful consideration. Key ethical principles include beneficence (acting in the client’s best interest), non-maleficence (avoiding harm), autonomy (respecting the client’s self-determination), and justice (fair and equitable treatment).
- Confidentiality: Balancing the adolescent’s right to confidentiality with the need to protect them from harm (e.g., suicidal ideation, self-harm, or abuse) is a constant challenge. I adhere to legal and ethical guidelines regarding mandatory reporting.
- Informed Consent: Obtaining informed consent from both the adolescent and their parent/guardian, while respecting the adolescent’s developmental capacity for decision-making, can be complex. I strive for a collaborative approach involving both parties.
- Dual Relationships: Avoiding potential conflicts of interest, such as social or business relationships with clients or their families, is critical.
- Boundaries: Maintaining clear professional boundaries is essential to ensuring ethical practice. This includes appropriate use of technology and personal interactions.
- Competence: Recognizing the limits of my expertise and referring adolescents to specialists when necessary is crucial.
When faced with a dilemma, I consult with supervisors, colleagues, and ethical guidelines to make informed and ethical decisions. Documentation is crucial in these situations.
Q 20. How do you collaborate with other professionals involved in the care of an adolescent patient?
Collaboration is essential in adolescent mental health. Effective care requires a multidisciplinary approach involving various professionals.
- Parents/Guardians: I actively involve parents or guardians in the treatment process, adapting my communication style to foster collaboration and shared decision-making. I recognize the importance of their perspective and support in the adolescent’s well-being.
- Educators: Communication with school personnel, such as teachers, counselors, and administrators, is important for understanding the adolescent’s academic performance, social interactions, and overall functioning at school. Collaboration helps create a supportive environment that promotes the adolescent’s success.
- Physicians: Consultation with a physician is important to rule out medical conditions that might contribute to mental health symptoms or to manage any co-occurring medical issues.
- Psychiatrists: Collaboration with psychiatrists is essential for medication management and the development of a comprehensive treatment plan.
- Social Workers: Social workers can provide valuable support with practical issues, such as accessing resources and navigating the social service system.
I utilize regular communication methods, such as case conferences, written reports, and phone calls, to maintain clear communication and coordination of care among all professionals involved. This team approach ensures a holistic and effective treatment plan for the adolescent.
Q 21. Describe your experience with adolescent substance abuse disorders.
Adolescent substance abuse disorders pose significant challenges, often requiring a comprehensive treatment approach. My experience involves working with adolescents struggling with various substances, from alcohol and marijuana to more potent drugs like opioids and stimulants.
- Assessment: A thorough assessment is crucial, including the type and frequency of substance use, the individual’s history, family dynamics, and any co-occurring mental health disorders (comorbidity). Tools like the Substance Abuse Subtle Screening Inventory (SASSI) can be valuable.
- Treatment Planning: Treatment plans are individualized, addressing the specific needs and circumstances of the adolescent. This often includes interventions such as motivational interviewing, cognitive-behavioral therapy (CBT) to address underlying issues contributing to substance use, and family therapy to address family dynamics and support systems.
- Medication Management: Collaboration with a psychiatrist may be necessary for medication management, especially if co-occurring mental health disorders are present.
- Relapse Prevention: A critical component of treatment is relapse prevention planning, which helps adolescents develop coping mechanisms and strategies to manage cravings and triggers.
- Aftercare Planning: Planning for aftercare is essential for continued support and to prevent relapse. This may involve ongoing therapy, support groups (such as Narcotics Anonymous or Alcoholics Anonymous), and participation in community-based programs.
I’ve found that a strengths-based approach, focusing on the adolescent’s resilience and positive attributes, is particularly effective in supporting their recovery. It’s vital to create a safe and non-judgmental environment where adolescents feel comfortable sharing their experiences and working toward recovery.
Q 22. What are some common challenges you encounter when working with adolescents?
Working with adolescents presents unique challenges. Their brains are still developing, leading to emotional volatility and impulsive behavior. Communication can be difficult, as they may struggle to articulate their feelings or may be resistant to help. Confidentiality concerns are paramount, requiring careful navigation of legal and ethical boundaries. Furthermore, navigating the complexities of family dynamics and societal pressures significantly impacts their mental well-being.
- Example 1: A teenager might present with seemingly unrelated somatic complaints (headaches, stomach aches) masking underlying anxiety or depression.
- Example 2: A young person struggling with identity issues might express anger and defiance as a way of coping with inner turmoil.
Addressing these challenges requires building rapport, utilizing developmentally appropriate communication techniques, and involving the family (with the adolescent’s consent) in a collaborative treatment approach. It also necessitates understanding the adolescent’s unique context and employing strategies that empower them to take control of their mental health.
Q 23. How do you maintain your own well-being while working in adolescent mental health?
Maintaining well-being as a professional in adolescent mental health is crucial to prevent burnout and compassion fatigue. It’s a demanding field, and prioritizing self-care is not a luxury but a necessity.
- Self-Reflection and Supervision: Regular supervision provides a safe space to process challenging cases and debrief with experienced colleagues. Self-reflection practices, like journaling or mindfulness, help maintain emotional balance.
- Setting Boundaries: Establishing clear boundaries between work and personal life is paramount. This includes limiting work hours, avoiding taking work home, and engaging in activities that foster relaxation and rejuvenation.
- Support Networks: Connecting with peers and professional organizations provides valuable support and a sense of community. Access to employee assistance programs or therapy can also be instrumental.
By consistently prioritizing my well-being, I can ensure I am best equipped to provide effective and empathetic care to my adolescent patients. Ignoring self-care is detrimental, not only to my health but to the quality of care I provide.
Q 24. What is your understanding of the role of peer influence on adolescent mental health?
Peer influence is a powerful force during adolescence. The desire for belonging and acceptance makes adolescents highly susceptible to the opinions and behaviors of their peers. This influence can be both positive and negative, significantly impacting their mental health.
- Positive Peer Influence: Supportive peer relationships can foster a sense of belonging, self-esteem, and resilience. Peers can encourage healthy coping mechanisms and provide emotional support.
- Negative Peer Influence: Peer pressure can lead to risky behaviors, such as substance abuse, self-harm, or eating disorders. Exposure to bullying, social exclusion, or online harassment can severely impact mental well-being.
Understanding the role of peer influence is critical in adolescent mental health treatment. Interventions might involve peer support groups, social skills training, or strategies to help adolescents navigate peer pressure and build healthy relationships.
Q 25. How do you ensure patient safety in adolescent mental health treatment?
Ensuring patient safety is paramount in adolescent mental health treatment. This involves a multi-faceted approach that incorporates risk assessment, safety planning, and ongoing monitoring.
- Risk Assessment: A thorough risk assessment is conducted at the outset and regularly updated to identify potential risks of self-harm, harm to others, or suicide. This involves careful consideration of the adolescent’s history, current symptoms, and environmental factors.
- Safety Planning: Collaboratively developing a safety plan with the adolescent and their family involves identifying warning signs, coping strategies, and support systems to utilize during times of crisis. This plan might include contact information for crisis lines, trusted adults, or mental health professionals.
- Monitoring: Regular monitoring of the adolescent’s mood, behavior, and adherence to the treatment plan is essential. This may involve frequent check-ins, involvement of family members, and close collaboration with other professionals involved in their care.
- Crisis Intervention: Having clear protocols in place for responding to crises, including procedures for immediate intervention and hospitalization if necessary, is vital.
The goal is to create a safe and supportive environment where adolescents feel comfortable seeking help and where appropriate interventions are readily available to prevent harm.
Q 26. Describe your experience with implementing and monitoring treatment plans for adolescents.
Implementing and monitoring treatment plans for adolescents is a collaborative process involving the adolescent, their family (when appropriate and with consent), and other relevant professionals.
- Collaborative Goal Setting: The initial step involves collaboratively identifying treatment goals that are realistic, measurable, achievable, relevant, and time-bound (SMART). These goals are tailored to the individual needs and preferences of the adolescent.
- Treatment Modalities: Treatment plans may incorporate various modalities, such as individual therapy, family therapy, group therapy, medication management (if indicated by a psychiatrist), and psychoeducational interventions.
- Regular Monitoring and Evaluation: Progress toward treatment goals is regularly monitored through sessions, self-report measures, and feedback from family members (if involved). The treatment plan is adjusted as needed to ensure its effectiveness and to address any emerging challenges.
- Documentation: Maintaining detailed and accurate records of sessions, assessments, and treatment progress is crucial for continuity of care and for legal and ethical compliance.
For example, a treatment plan for an adolescent experiencing anxiety might involve cognitive-behavioral therapy (CBT) to address negative thought patterns, relaxation techniques to manage physical symptoms, and family therapy to improve communication and support.
Q 27. Explain your knowledge of relevant legislation and regulations regarding adolescent mental health.
Knowledge of relevant legislation and regulations regarding adolescent mental health is crucial for ethical and legal practice. These vary by jurisdiction, but generally cover areas such as:
- Confidentiality: Understanding the limits of confidentiality, especially concerning issues such as self-harm, harm to others, and mandated reporting requirements, is essential.
- Consent: Obtaining informed consent from the adolescent and their parents/guardians (depending on age and legal jurisdiction) is crucial before initiating any treatment.
- Data Privacy: Adhering to regulations surrounding the collection, storage, and use of patient data is paramount to ensure privacy and security.
- Record Keeping: Maintaining accurate and complete records according to professional and legal standards is vital.
Staying updated on these regulations is an ongoing process. This often involves participation in professional development activities and consultation with legal advisors when needed. Failure to comply with relevant legislation can lead to serious consequences, both professionally and legally.
Q 28. How do you measure the effectiveness of your interventions with adolescent patients?
Measuring the effectiveness of interventions with adolescent patients involves multiple methods. There’s no single metric; rather, a multifaceted approach is necessary.
- Self-Report Measures: Standardized questionnaires and scales (e.g., depression, anxiety, self-esteem measures) assess symptom severity and track changes over time. These provide valuable quantitative data.
- Clinical Observation: Qualitative data from direct observation during therapy sessions helps to gauge the adolescent’s mood, behavior, and progress in achieving treatment goals.
- Feedback from Family and Other Professionals: Input from parents, teachers, and other involved professionals offers perspectives on the adolescent’s functioning in different settings.
- Functional Outcomes: Assessing improvement in daily functioning, such as school performance, social interactions, and engagement in activities, provides a broader measure of treatment success.
By combining these methods, a comprehensive picture of treatment effectiveness emerges. Regular reviews of this data enable adjustments to the treatment plan to maximize outcomes and ensure that interventions are truly making a positive impact on the adolescent’s life.
Key Topics to Learn for Adolescent Mental Health Interview
- Developmental Psychopathology: Understanding typical adolescent development and how deviations manifest as mental health challenges. Consider the impact of biological, psychological, and social factors.
- Common Adolescent Mental Health Disorders: Gain a strong understanding of anxiety disorders (generalized anxiety, social anxiety, panic disorder), depressive disorders, ADHD, eating disorders, substance use disorders, and self-harm behaviors. Be prepared to discuss diagnostic criteria and typical presentations.
- Assessment and Diagnosis: Familiarize yourself with various assessment methods used with adolescents, including clinical interviews, behavioral observations, and standardized psychological tests. Understand the ethical considerations involved in adolescent assessment.
- Evidence-Based Interventions: Explore effective therapeutic approaches such as Cognitive Behavioral Therapy (CBT), Dialectical Behavior Therapy (DBT), family therapy, and psychopharmacology in the context of adolescent mental health. Be prepared to discuss the rationale and limitations of each approach.
- Crisis Intervention and Risk Assessment: Learn to identify and respond to situations involving suicidal ideation, self-harm, and other crises. Understand the process of conducting a thorough risk assessment and developing safety plans.
- Ethical and Legal Considerations: Familiarize yourself with relevant ethical guidelines and legal frameworks related to confidentiality, informed consent, and mandatory reporting in adolescent mental health care.
- Cultural Competence and Diversity: Understand how cultural background, socioeconomic status, and other factors influence the presentation and treatment of adolescent mental health disorders. Be prepared to discuss culturally sensitive practices.
- Collaboration and Teamwork: Discuss the importance of collaboration with families, schools, and other professionals involved in the care of adolescents with mental health challenges.
- Case Management and Treatment Planning: Understand the process of developing and implementing comprehensive treatment plans for adolescents with mental health disorders, including coordination of care and ongoing monitoring of progress.
Next Steps
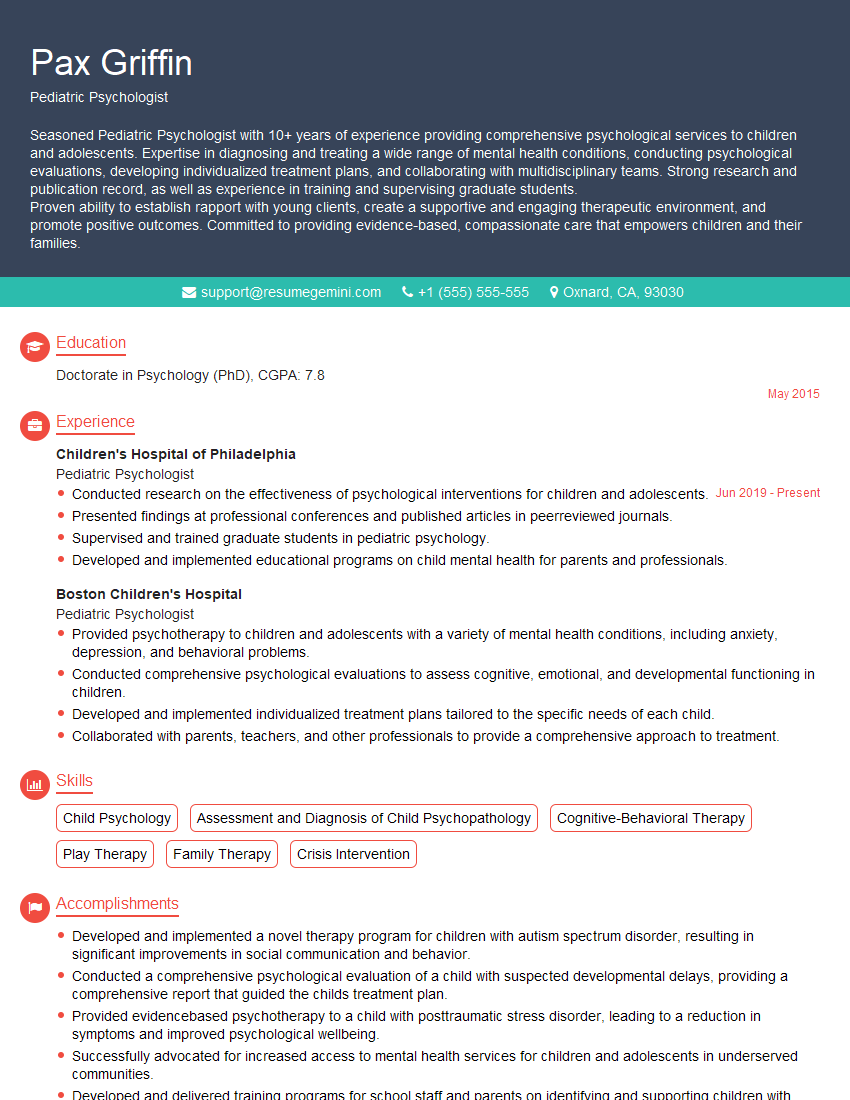
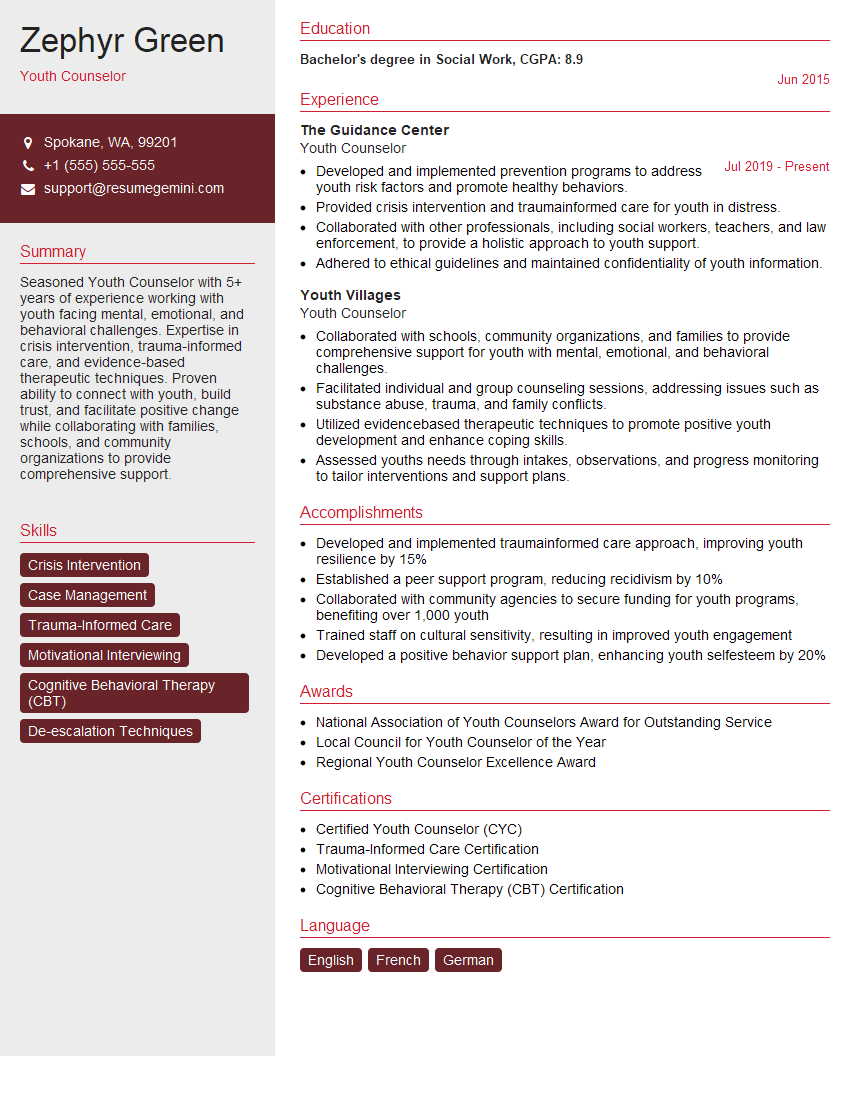
Mastering Adolescent Mental Health is crucial for a rewarding and impactful career. This specialized field offers significant growth opportunities and allows you to make a real difference in the lives of young people. To maximize your job prospects, it’s vital to present yourself effectively. Creating an ATS-friendly resume is paramount in getting your application noticed. ResumeGemini is a trusted resource to help you build a professional and impactful resume, optimized for Applicant Tracking Systems. Examples of resumes tailored to Adolescent Mental Health are available to help you craft a compelling application that showcases your skills and experience. Invest in your future; invest in your resume.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Live Rent Free!
https://bit.ly/LiveRentFREE
Interesting Article, I liked the depth of knowledge you’ve shared.
Helpful, thanks for sharing.
Hi, I represent a social media marketing agency and liked your blog
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?