Interviews are opportunities to demonstrate your expertise, and this guide is here to help you shine. Explore the essential Hospital Medicine interview questions that employers frequently ask, paired with strategies for crafting responses that set you apart from the competition.
Questions Asked in Hospital Medicine Interview
Q 1. Describe your approach to managing a patient with acute decompensated heart failure.
Managing acute decompensated heart failure (ADHF) requires a rapid and systematic approach focusing on hemodynamic stabilization and addressing the underlying cause. Think of it like fixing a leaky pipe – we need to stop the leak (reduce fluid overload) and address the cause of the leak (underlying heart problem).
- Immediate Assessment: I begin with a thorough assessment including vital signs (especially blood pressure, heart rate, and respiratory rate), oxygen saturation, and auscultation for lung sounds (rales indicating fluid overload) and heart sounds (murmurs suggesting valvular issues). I’ll also check for jugular venous distension (JVD) and peripheral edema.
- Oxygen Therapy: Supplemental oxygen is crucial to improve tissue oxygenation. I’ll aim for an SpO2 above 90%.
- Diuretics: Loop diuretics like furosemide are the cornerstone of treatment, helping to reduce fluid overload and alleviate pulmonary edema. I carefully titrate the dose based on the patient’s response and renal function. For example, a patient with severe pulmonary edema might initially receive a bolus of furosemide, followed by continuous infusion.
- Vasodilators: In patients with elevated filling pressures, vasodilators like nitroglycerin can help reduce preload and afterload, improving cardiac output. These are carefully monitored for hypotension.
- Inotropes: If the patient remains hypotensive despite fluid management and vasodilators, inotropes like dobutamine may be necessary to support cardiac contractility. These drugs require close hemodynamic monitoring.
- Further Investigations: I’ll order blood tests (including BNP/NT-proBNP, electrolytes, creatinine), chest X-ray (to assess pulmonary edema), and potentially an echocardiogram to assess left ventricular function and ejection fraction. These help determine the underlying cause of the heart failure.
- Long-Term Management: Discharge planning is crucial. This includes medication optimization (ACE inhibitors, beta-blockers, aldosterone antagonists), dietary recommendations (sodium restriction), patient education, and follow-up appointments to prevent future episodes.
For instance, I recently managed a patient with ADHF who presented with severe shortness of breath and pulmonary edema. After initial stabilization with oxygen and diuretics, we found they had severe mitral regurgitation requiring valve repair. Post-surgical recovery and long-term management significantly improved their quality of life.
Q 2. Explain your understanding of sepsis protocols and early goal-directed therapy.
Sepsis protocols and early goal-directed therapy (EGDT) are essential for improving outcomes in patients with sepsis. Sepsis, a life-threatening organ dysfunction caused by a dysregulated host response to infection, demands immediate intervention. EGDT focuses on rapid resuscitation to restore tissue perfusion and organ function.
- Early Recognition: Sepsis is often identified using the quick SOFA (qSOFA) score, assessing respiratory rate, altered mentation, and systolic blood pressure. A high score warrants immediate investigation and treatment.
- Rapid Resuscitation: EGDT aims to achieve early goals such as central venous oxygen saturation (ScvO2) above 70% and mean arterial pressure (MAP) above 65 mmHg. This often involves fluid resuscitation with crystalloids, followed by vasopressors (e.g., norepinephrine) if hypotension persists.
- Antibiotics: Broad-spectrum antibiotics should be administered as early as possible, ideally within the first hour of suspected sepsis. Antibiotic selection is guided by clinical suspicion and local antibiograms.
- Source Control: Identifying and treating the source of infection (e.g., pneumonia, urinary tract infection) is crucial. This might involve drainage of abscesses, surgical debridement, or other interventions.
- Monitoring: Continuous monitoring of vital signs, lactate levels (a marker of tissue hypoxia), and organ function (e.g., urine output, mental status) is essential to guide treatment.
- Other Therapies: Other supportive therapies include mechanical ventilation, renal replacement therapy (if needed), and management of other organ dysfunction.
Imagine a patient presenting with fever, hypotension, and altered mental status. Using EGDT, we’d rapidly administer fluids, antibiotics, and vasopressors while simultaneously searching for the source of infection (e.g., through blood cultures and imaging). Close monitoring allows for adjustments in therapy based on the patient’s response.
Q 3. How do you differentiate between pneumonia and acute bronchitis in a hospitalized patient?
Differentiating between pneumonia and acute bronchitis in hospitalized patients requires a careful clinical evaluation, integrating history, physical examination, and imaging studies. Both involve inflammation of the airways, but pneumonia involves alveolar involvement, leading to more severe illness.
- History: Pneumonia is often associated with more severe symptoms such as high fever, productive cough (with purulent sputum), pleuritic chest pain, and shortness of breath. Bronchitis typically presents with a less severe cough, often without fever or pleuritic pain.
- Physical Examination: Pneumonia may present with findings such as crackles (rales) or wheezes on auscultation of the lungs, and possibly signs of consolidation. Bronchitis typically exhibits wheezes and/or rhonchi without consolidation.
- Imaging: Chest X-ray is crucial. Pneumonia will show characteristic infiltrates or consolidation. A normal or near-normal chest X-ray strongly suggests bronchitis.
- Laboratory Tests: Blood tests (complete blood count and inflammatory markers like CRP) may show increased white blood cell counts in pneumonia but are often less helpful in distinguishing between the two conditions. Sputum culture and analysis can help identify the causative organism in pneumonia.
For instance, a patient with a productive cough, high fever, and crackles on lung auscultation along with a chest X-ray showing consolidation will be diagnosed with pneumonia. A patient presenting with a non-productive cough and wheezes, a normal chest x-ray, and normal inflammatory markers likely has bronchitis.
Q 4. What is your approach to managing a patient with acute coronary syndrome?
Managing acute coronary syndrome (ACS), encompassing unstable angina, non-ST-segment elevation myocardial infarction (NSTEMI), and ST-segment elevation myocardial infarction (STEMI), is a time-critical process. The goal is to rapidly reperfuse the ischemic myocardium to limit infarct size and improve survival.
- Immediate Assessment: This includes a thorough history focusing on chest pain characteristics, risk factors, and associated symptoms (e.g., shortness of breath, diaphoresis). A 12-lead ECG is essential to identify ST-segment elevation (indicating STEMI) or other ECG changes suggesting myocardial ischemia.
- STEMI Management: Patients with STEMI require immediate reperfusion therapy – either percutaneous coronary intervention (PCI) or fibrinolytic therapy (if PCI is unavailable). Time is muscle in STEMI; the faster the reperfusion, the better the outcome.
- NSTEMI/Unstable Angina Management: These patients require early risk stratification using risk scores and cardiac biomarkers (troponin). Management includes antiplatelet therapy (aspirin, P2Y12 inhibitors), anticoagulation (heparin), and nitrates for pain relief. Patients at high risk may undergo coronary angiography and PCI.
- Medical Management: All ACS patients receive oxygen, beta-blockers (to reduce myocardial oxygen demand), statins (to reduce cholesterol), and ACE inhibitors (to reduce blood pressure and afterload).
- Monitoring: Continuous monitoring of vital signs, ECG, and cardiac biomarkers is crucial to assess response to treatment and detect any complications.
For example, a patient presenting with crushing chest pain and ST-segment elevation would immediately undergo PCI, while a patient with unstable angina and negative troponin might receive medical therapy and undergo coronary angiography later based on risk stratification.
Q 5. How would you manage a patient experiencing a hypertensive crisis?
Managing a hypertensive crisis, defined as severely elevated blood pressure with evidence of end-organ damage, requires a prompt and cautious approach. The goal is to reduce blood pressure gradually to avoid potentially harmful consequences.
- Assessment: Determine the severity of hypertension and identify evidence of end-organ damage (e.g., stroke, encephalopathy, renal failure, acute heart failure). This involves a thorough neurological exam, checking urine output, and evaluating for signs of heart failure.
- Initial Management: For hypertensive emergencies (e.g., malignant hypertension, hypertensive encephalopathy, acute aortic dissection), intravenous medications are usually necessary. Sodium nitroprusside, nicardipine, labetalol, or esmolol are commonly used, titrated to lower blood pressure gradually.
- Hypertensive Urgencies: In hypertensive urgencies (severe hypertension without end-organ damage), oral medications can be used. Usually a combination of a fast-acting medication (e.g., clonidine, captopril) with a longer-acting agent (e.g., beta-blocker, thiazide diuretic).
- Gradual Reduction: The goal is to lower blood pressure by approximately 25% within the first hour, and to a target level over the next 24 hours, taking into account the individual patient’s tolerance and underlying conditions.
- Monitoring: Continuous monitoring of blood pressure, heart rate, urine output, and neurological status is essential. Any signs of hypotension or organ dysfunction must be addressed promptly.
For example, a patient presenting with severe headache, visual changes, and elevated blood pressure might be diagnosed with hypertensive encephalopathy and require intravenous sodium nitroprusside to gradually lower blood pressure while closely monitoring neurological status.
Q 6. Discuss your experience with ventilator management.
My experience with ventilator management encompasses all aspects, from initial patient assessment and ventilator selection to weaning strategies and managing complications. It’s a complex process demanding close monitoring and expertise.
- Patient Assessment: Before initiating ventilation, a detailed assessment is crucial. This includes evaluating the patient’s respiratory status (respiratory rate, work of breathing, oxygenation), hemodynamic stability, and neurological status. Underlying conditions like COPD or neuromuscular disease profoundly impact ventilator management.
- Ventilator Settings: Appropriate ventilator settings are crucial. These settings are individualized based on the patient’s specific needs and goals. Factors like tidal volume, respiratory rate, FiO2 (fraction of inspired oxygen), PEEP (positive end-expiratory pressure), and ventilator mode (e.g., volume control, pressure control) are carefully selected and adjusted.
- Monitoring: Continuous monitoring of ventilator parameters, arterial blood gases, and hemodynamic parameters is crucial. This ensures the patient’s oxygenation, ventilation, and acid-base balance are adequately maintained.
- Weaning Strategies: Weaning from mechanical ventilation involves a gradual reduction in ventilator support to allow the patient to breathe spontaneously. This is a stepwise process, often involving a trial of spontaneous breathing with decreasing ventilator support. Several weaning parameters (e.g., respiratory rate, tidal volume, vital capacity) are monitored.
- Complication Management: Ventilator-associated complications like ventilator-associated pneumonia (VAP), barotrauma, and volutrauma require prompt recognition and management. Prophylactic measures (e.g., oral care, elevation of the head of the bed) are crucial.
For instance, I recently managed a patient with severe ARDS requiring prolonged mechanical ventilation. Careful attention to ventilator settings, frequent blood gas monitoring, and a gradual weaning strategy led to successful extubation.
Q 7. Outline your strategy for managing a patient with diabetic ketoacidosis.
Diabetic ketoacidosis (DKA) is a life-threatening complication of diabetes characterized by hyperglycemia, ketosis, and acidosis. Management requires a multi-faceted approach aimed at correcting fluid and electrolyte imbalances, resolving acidosis, and addressing the underlying hyperglycemia.
- Fluid Resuscitation: Initial management focuses on fluid resuscitation with isotonic saline to correct dehydration. The rate and volume of fluid administration are adjusted based on the patient’s hemodynamic status and urine output.
- Insulin Infusion: A continuous intravenous insulin infusion is the cornerstone of DKA management. The dose is carefully titrated to lower blood glucose gradually, while closely monitoring potassium levels.
- Potassium Replacement: Potassium is often depleted in DKA due to osmotic diuresis. Careful monitoring and replacement are essential. Even if serum potassium appears normal, significant intracellular potassium deficiency exists, needing replacement along with insulin.
- Bicarbonate Administration: Bicarbonate administration is generally avoided unless the pH is critically low (below 6.9) as it can potentially worsen potassium imbalance and hinder the action of insulin.
- Monitoring: Continuous monitoring of blood glucose, electrolytes (particularly potassium), pH, and arterial blood gases is crucial. Patients are also monitored for any signs of dehydration, cardiovascular instability, and cerebral edema.
- Underlying Cause: Identifying and addressing the underlying cause of DKA, such as infection, is crucial for preventing recurrence.
For example, a patient presenting with hyperglycemia, ketonemia, and severe acidosis would receive intravenous fluids, insulin, and potassium while monitoring electrolytes and blood gases. Careful titration of insulin ensures gradual correction of hyperglycemia and avoids hypoglycemia.
Q 8. How do you assess and manage pain in hospitalized patients?
Pain assessment and management in hospitalized patients is a crucial aspect of holistic care. It involves a multifaceted approach focusing on understanding the patient’s experience, identifying the source of pain, and implementing effective interventions. We begin with a thorough history, including location, onset, character, radiation, severity (often using a validated pain scale like the numeric rating scale or the visual analog scale), timing, exacerbating and relieving factors. A physical exam follows, focusing on the area of reported pain and looking for any signs of underlying pathology.
Next, we consider non-pharmacological interventions such as repositioning, splinting, heat/cold therapy, and relaxation techniques. These are often the first line of defense and should always be considered. Pharmacological management utilizes a tiered approach. Mild to moderate pain might be managed with analgesics such as acetaminophen or NSAIDs. Moderate to severe pain often requires opioids, carefully titrated to the patient’s response and closely monitored for side effects such as respiratory depression and constipation. We also carefully consider the patient’s comorbidities and potential drug interactions when selecting and dosing medications. Regular reassessment of pain levels is essential, and adjustments to the pain management plan are made as needed to achieve adequate pain control. For instance, if a patient reports persistent pain despite initial treatment, we would revisit the assessment, explore other potential causes, and consider alternative analgesics or interventional pain management techniques.
A critical element is to involve the patient in their pain management plan. Patient education about different pain management options and the importance of reporting any changes in pain level or side effects is vital. We actively solicit their feedback and preferences to ensure we create a plan that works for them.
Q 9. Explain your approach to managing a patient with acute kidney injury.
Managing acute kidney injury (AKI) requires a systematic approach focused on identifying the cause, supporting renal function, and preventing complications. The initial steps involve a thorough history and physical examination, supplemented by laboratory investigations including serum creatinine, BUN, electrolytes, urine analysis, and imaging studies (e.g., ultrasound) if indicated. The etiology of AKI is categorized as pre-renal (hypovolemia, hypotension), intra-renal (nephrotoxic drugs, acute tubular necrosis), or post-renal (obstruction). Determining the underlying cause is paramount for effective treatment.
Treatment strategies vary depending on the cause. Pre-renal AKI requires fluid resuscitation to restore intravascular volume and improve renal perfusion. Intra-renal AKI may require specific interventions targeting the underlying cause, such as stopping nephrotoxic medications or managing sepsis. Post-renal AKI requires addressing the obstruction through procedures such as catheterization or stenting. In all cases, close monitoring of fluid balance, electrolytes, and renal function is crucial. Dialysis may be necessary in cases of severe AKI or if there is a significant accumulation of toxins or fluid overload.
For example, if a patient presents with AKI after taking an NSAID and exhibiting signs of dehydration, I would initiate fluid resuscitation with intravenous fluids, discontinue the NSAID, and closely monitor renal function parameters. If the AKI fails to improve, I would then consider additional interventions or consult a nephrologist. Early identification and appropriate management of AKI are vital to minimizing long-term complications and improving patient outcomes.
Q 10. What is your experience with central line insertion and management?
I have extensive experience with central line insertion and management, having performed and supervised numerous procedures. My experience encompasses both internal jugular and subclavian approaches, along with femoral access in selected cases. I am proficient in using ultrasound guidance for central line placement, which significantly reduces the risk of complications like pneumothorax and arterial puncture. Pre-procedure checklist adherence, including proper skin antisepsis, sterile technique, and patient positioning, is a routine part of my practice.
Post-insertion, I meticulously follow protocols for line care and management. This includes regular assessment of the insertion site for signs of infection or infiltration, adherence to sterile technique during dressing changes, and the implementation of appropriate flushing protocols. I am adept at troubleshooting common complications, such as catheter occlusion or infection, using appropriate interventions like thrombolytic agents or antibiotic therapy. Regular blood cultures are taken when there is any suspicion of infection. I also ensure all documentation, including insertion site details, catheter type, and maintenance procedures, is meticulously recorded in the patient’s medical record.
I strongly believe in continuous learning and have kept abreast of the latest guidelines and best practices in central line insertion and management to ensure patient safety and reduce the risk of complications.
Q 11. Discuss your understanding of the importance of medication reconciliation.
Medication reconciliation is a crucial process that involves comparing a patient’s current medication list with their previous medication list to identify any discrepancies. It’s a cornerstone of safe and effective patient care, particularly important upon hospital admission, transfer between units, and discharge. Errors in medication reconciliation can lead to adverse drug events, including medication errors, interactions, and duplications, ultimately impacting patient safety and outcomes.
My approach begins with a comprehensive review of the patient’s medication history, which includes prescription medications, over-the-counter medications, herbal supplements, and any other substances the patient may be using. This information is gathered from various sources, such as the patient themselves, their family members, and their previous medical records (if available). Then we compare this information to the medication orders entered upon admission. Any discrepancies, omissions, or potential interactions are identified, and appropriate actions are taken to resolve these issues. This often involves consulting with pharmacists and specialists to ensure that the patient’s medications are safe and effective.
A real-world example would be a patient transferred from another hospital with a list of medications that did not accurately reflect the current prescribed medications. Medication reconciliation revealed a significant discrepancy, and we were able to prevent a potential drug interaction. Medication reconciliation is a vital part of preventing medication-related errors and improving patient safety, thus contributing to better clinical outcomes.
Q 12. Describe your experience with code blue management.
My experience with code blue management is extensive and involves a structured approach based on advanced cardiac life support (ACLS) protocols. My role encompasses the immediate assessment of the patient’s condition, initiation of basic life support (BLS) measures such as chest compressions and airway management, and effective communication with the resuscitation team. The importance of a calm and coordinated approach is paramount during such high-pressure situations.
My responsibilities include leading or actively participating in the team effort to establish and maintain an airway, provide adequate ventilation and oxygenation, perform defibrillation when necessary, administer medications as per ACLS guidelines (e.g., epinephrine, amiodarone), and monitoring vital signs, cardiac rhythm, and response to treatment. Post-resuscitation care is equally critical; this involves stabilization of the patient, documentation of the events, and ongoing monitoring for any complications or secondary effects.
Effective communication among team members is essential. I’ve found clear, concise communication, assigning roles promptly, and debriefing after the event to be important factors contributing to efficient and effective resuscitation efforts. Regular training and participation in simulations help maintain proficiency and prepare us for these critical situations.
Q 13. How would you manage a patient with a suspected pulmonary embolism?
Suspected pulmonary embolism (PE) requires prompt evaluation and management due to its potentially life-threatening nature. My approach begins with a comprehensive assessment of the patient’s history, including risk factors such as recent surgery, prolonged immobility, malignancy, and pregnancy, along with the clinical presentation, which may include dyspnea, chest pain, tachycardia, and hypoxia. A thorough physical examination is conducted to look for signs of deep vein thrombosis (DVT).
Diagnostic testing is crucial, and I would typically order a d-dimer test as an initial screening tool. A high probability clinical scenario coupled with an elevated d-dimer level generally prompts further investigation with computed tomography pulmonary angiography (CTPA), the gold standard for diagnosing PE. If CTPA is contraindicated or unavailable, a ventilation-perfusion (V/Q) scan might be considered, although this is less sensitive and specific than CTPA. Treatment is guided by the clinical severity and the results of diagnostic imaging.
Treatment options include anticoagulation therapy with heparin (either unfractionated or low molecular weight) followed by a longer-term oral anticoagulant such as warfarin, apixaban, rivaroxaban, or dabigatran. The choice of anticoagulant depends on factors such as renal function, other medical conditions, and patient-specific preferences. In cases of massive PE with hemodynamic instability, thrombolytic therapy might be considered, but this is a high-risk procedure that necessitates careful risk-benefit assessment. Close monitoring of vital signs, oxygen saturation, and anticoagulation parameters is crucial throughout the treatment course.
Q 14. Explain your approach to managing a patient with a gastrointestinal bleed.
Management of a gastrointestinal bleed (GIB) necessitates a rapid and systematic approach to stabilize the patient and identify the source of bleeding. Initial assessment involves evaluating the patient’s hemodynamic status, looking for signs of hypovolemia such as hypotension, tachycardia, and pallor. A thorough history, including recent medication use, known bleeding disorders, and alcohol consumption, is essential. Physical examination focuses on identifying the site and severity of bleeding (e.g., hematemesis, melena, hematochezia).
Laboratory investigations include complete blood count (CBC) to assess hemoglobin and hematocrit, coagulation studies (PT, PTT, INR), blood type and crossmatch, and electrolyte levels. Endoscopy (upper or lower) is often the procedure of choice to determine the source of the bleed and potentially cauterize or clip the bleeding vessel. Other imaging techniques, such as angiography, might be necessary in certain cases.
Treatment strategies are tailored to the cause and severity of the bleed. Fluid resuscitation with intravenous fluids is critical to maintain hemodynamic stability. Blood transfusions might be required to correct anemia. Pharmacologic interventions include medications to reduce gastric acid secretion (proton pump inhibitors or H2 blockers) and vasoconstrictors to stop bleeding. Surgical intervention may be necessary if endoscopic management fails or in cases of severe ongoing bleeding. Post-bleed care involves close monitoring of hemodynamic parameters, repeat endoscopy as needed, and ongoing management of any complications.
Q 15. What are the key elements of a thorough inpatient admission note?
A thorough inpatient admission note is the cornerstone of effective hospital care. It serves as a comprehensive record of the patient’s presentation, ensuring continuity of care and facilitating clear communication among the healthcare team. Key elements include:
- Identifying Information: Patient’s name, date of birth, medical record number, etc.
- Reason for Admission (RFA): A concise statement summarizing the primary reason for hospitalization. For example, ‘Acute exacerbation of COPD’ or ‘Chest pain suggestive of myocardial infarction’.
- History of Present Illness (HPI): A detailed chronological account of the patient’s symptoms leading to admission, including onset, duration, character, location, aggravating and relieving factors. This section should be detailed and use specific medical terminology when appropriate, while remaining understandable to other members of the healthcare team. For example, describing a chest pain as ‘sharp, stabbing pain radiating to the left arm’ is more informative than ‘chest pain’.
- Past Medical History (PMH): A complete list of past illnesses, surgeries, allergies, and significant medical events.
- Medications: A current list of all medications, including dosages and frequencies, both prescription and over-the-counter.
- Allergies: A comprehensive list of known drug allergies and reactions.
- Family History (FH): Significant family history of diseases, particularly those relevant to the patient’s current condition.
- Social History (SH): Relevant details about the patient’s lifestyle, including smoking, alcohol use, drug use, occupation, and support system.
- Review of Systems (ROS): A systematic inquiry into each body system to identify additional symptoms or concerns.
- Physical Examination (PE): A detailed description of the patient’s physical findings, including vital signs, heart and lung sounds, abdominal examination, etc. This section should include both objective and subjective findings.
- Assessment and Plan (A&P): This is arguably the most important part; it summarizes the clinician’s interpretation of the patient’s condition, including differential diagnoses, working diagnoses, and a detailed plan of care, including diagnostic tests, treatments, and consults.
A well-written admission note minimizes errors, ensures efficient care, and supports legal defensibility.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you assess and manage delirium in hospitalized patients?
Delirium, an acute confusional state, is a common and serious problem in hospitalized patients, often leading to increased morbidity and mortality. Assessment involves recognizing the characteristic features: acute onset of fluctuating cognitive impairment, inattention, disorganized thinking, and altered level of consciousness. The Confusion Assessment Method (CAM) is a validated tool to assist in diagnosis.
Management hinges on identifying and addressing underlying causes. This necessitates a thorough workup, including:
- Medication Review: Polypharmacy and certain medications (e.g., opioids, benzodiazepines) are significant risk factors.
- Infection Screen: Urinary tract infections, pneumonia, and sepsis are frequently associated with delirium.
- Metabolic Panel: Assessment for electrolyte imbalances, hypoglycemia, or other metabolic derangements.
- Brain Imaging: Considered if stroke, hemorrhage, or other neurological conditions are suspected.
Once underlying causes are addressed, supportive measures are crucial:
- Environmental Modifications: A calm, well-lit environment with minimal distractions can significantly improve the patient’s cognitive state.
- Reorientation: Regularly orienting the patient to time, place, and person.
- Sleep Hygiene: Promoting adequate sleep through a regular sleep-wake cycle.
- Mobilization: Early mobilization, if tolerated, helps prevent further complications.
- Nonpharmacological Interventions: Family involvement, communication techniques, and cognitive stimulation.
- Pharmacological Interventions: Antipsychotics (e.g., haloperidol) may be used for severe agitation or psychosis, but should be used cautiously and only when necessary, given the potential for adverse effects.
For example, a patient with a urinary tract infection and on multiple medications might experience delirium. Treating the infection and reviewing the medication list are crucial steps toward management. Providing a calm environment and involving family members are also essential for effective care.
Q 17. Describe your understanding of hospital-acquired infections and prevention strategies.
Hospital-acquired infections (HAIs) are infections that patients acquire during their stay in a hospital or other healthcare facility. These infections can range from minor skin infections to life-threatening sepsis and significantly increase morbidity, mortality, and healthcare costs. Common HAIs include catheter-associated urinary tract infections (CAUTIs), central line-associated bloodstream infections (CLABSIs), ventilator-associated pneumonia (VAP), and surgical site infections (SSIs).
Prevention strategies are multi-faceted and involve a combination of interventions:
- Hand Hygiene: The most crucial step, emphasizing meticulous handwashing with soap and water or alcohol-based hand rub before and after patient contact.
- Infection Control Protocols: Adherence to established guidelines for the use of personal protective equipment (PPE), such as gloves, gowns, and masks, when appropriate.
- Sterile Techniques: Proper sterilization of equipment and meticulous aseptic technique during procedures to minimize the risk of contamination.
- Antibiotic Stewardship: Judicious use of antibiotics, guided by culture and sensitivity results, to prevent the development of antibiotic resistance and minimize collateral damage to the patient’s microbiome.
- Environmental Cleaning: Regular and thorough cleaning and disinfection of patient rooms and equipment.
- Isolation Precautions: Implementing appropriate isolation precautions for patients with known or suspected infections to prevent transmission to other patients and healthcare workers.
- Vaccination: Promoting vaccination against influenza and pneumococcal pneumonia, reducing the overall risk of infection.
- Surveillance: Active surveillance programs to identify and track HAIs, enabling prompt intervention and prevention strategies.
A practical example: Implementing a bundle of measures to prevent CLABSIs, including hand hygiene, chlorhexidine skin disinfection, and optimal catheter insertion techniques, can dramatically reduce the incidence of these infections.
Q 18. What is your experience with critical care transitions?
Critical care transitions, the movement of patients from the intensive care unit (ICU) back to the general ward, require meticulous planning and coordination. My experience involves ensuring a smooth and safe transfer, minimizing complications, and facilitating ongoing optimal management. This includes:
- Comprehensive Communication: A detailed handover report from the ICU team, including a summary of the patient’s condition, treatment received, and ongoing needs. This often involves detailed discussions with the ICU physician and nursing staff.
- Assessment of the Patient’s Status: A thorough reassessment of the patient’s hemodynamic stability, respiratory function, and neurological status upon arrival on the general ward.
- Medication Reconciliation: Careful review and reconciliation of the patient’s medication regimen to ensure accuracy and minimize errors during the transition.
- Monitoring and Support: Close monitoring for early signs of deterioration, providing prompt escalation of care if necessary.
- Patient and Family Education: Educating patients and families about the ongoing treatment plan and potential challenges.
- Collaboration with Allied Health Professionals: Involving physical and occupational therapists, respiratory therapists, and other relevant professionals to ensure optimal rehabilitation and recovery.
One example: I recently managed the transition of a patient from the ICU after a cardiac arrest. Through close collaboration with the ICU team, careful monitoring, and prompt attention to subtle changes in the patient’s condition, we prevented readmission to the ICU and facilitated a successful discharge.
Q 19. How do you handle difficult conversations with patients and families?
Difficult conversations with patients and families are an inevitable aspect of hospital medicine. My approach emphasizes empathy, active listening, and clear communication. I use a structured approach, such as the ‘SPIKES’ protocol (Setting, Perception, Invitation, Knowledge, Emotions, Strategy), to deliver difficult news or discuss complex treatment options. This ensures that information is conveyed in a sensitive and respectful manner.
Key elements include:
- Active Listening: Allowing patients and families to express their concerns and emotions without interruption.
- Empathy: Showing understanding and compassion for their situation.
- Clear and Concise Communication: Using plain language, avoiding medical jargon, and checking for understanding.
- Shared Decision-Making: Involving patients and families in the decision-making process as much as possible, respecting their autonomy and preferences.
- Addressing Emotional Needs: Recognizing and addressing the emotional impact of the illness and treatment decisions.
- Providing Support: Connecting patients and families to appropriate support resources, such as social workers, chaplains, or support groups.
For example, when delivering a diagnosis of a serious illness, I begin by creating a comfortable environment, then carefully assess the patient’s understanding of the situation before delivering the news. I always allow time for questions and provide ongoing support.
Q 20. Describe your experience with quality improvement initiatives in hospital medicine.
I have been actively involved in several quality improvement (QI) initiatives in hospital medicine. My experience encompasses various methodologies, from implementing evidence-based guidelines to utilizing data analysis for process improvement.
Examples of my involvement include:
- Reducing CLABSIs: Participating in a multidisciplinary team focused on reducing central line-associated bloodstream infections through the implementation of a standardized bundle of interventions. This involved data collection, process mapping, and ongoing monitoring of infection rates. This resulted in a significant reduction of CLABSIs within our institution. We saw a 40% reduction in CLABSIs after implementation of the bundle.
- Improving Medication Reconciliation: Leading an initiative to improve medication reconciliation processes on admission and discharge. This involved developing a new standardized protocol, implementing training programs for staff, and monitoring compliance rates. We saw a 25% reduction in medication discrepancies after implementing the new protocol.
- Streamlining Discharge Processes: Participating in a project to streamline discharge processes, reducing delays and improving patient satisfaction. This involved identifying bottlenecks in the process and implementing solutions, such as early discharge planning and improved communication with patients and families. This led to a 15% decrease in average length of stay for those meeting criteria for early discharge.
My approach to QI emphasizes a data-driven methodology, utilizing Plan-Do-Study-Act (PDSA) cycles to iteratively improve processes and achieve sustainable change. I firmly believe that collaborative efforts across disciplines are essential for successful QI initiatives.
Q 21. Explain your approach to managing a patient with acute pancreatitis.
Acute pancreatitis is a serious inflammatory condition of the pancreas, requiring prompt and effective management. My approach involves a systematic approach focusing on supportive care and addressing underlying etiologies.
Initial management focuses on:
- Fluid Resuscitation: Aggressive intravenous fluid resuscitation to maintain adequate intravascular volume and organ perfusion. Close monitoring of hemodynamics and fluid balance is crucial.
- Pain Management: Effective pain control, often utilizing intravenous opioids, is paramount. I usually tailor the analgesia to each individual’s needs and pain level.
- NPO Status (Nothing by Mouth): Initially maintaining NPO status to reduce pancreatic stimulation and allow the inflammation to subside. Nutritional support may be initiated via parenteral nutrition once the patient stabilizes.
- Laboratory Investigations: Comprehensive blood tests to assess pancreatic enzymes (amylase and lipase), complete blood count (CBC), metabolic panel, and liver function tests.
- Imaging: Abdominal imaging, usually CT scan, to assess the severity of pancreatitis and identify complications, such as necrosis or pseudocysts.
Depending on severity, further management may include:
- Antibiotics: For patients with infected necrosis or suspected infection.
- Nutritional Support: Enteral or parenteral nutrition based on the patient’s tolerance and condition.
- Surgical Intervention: In cases of severe necrotizing pancreatitis or complications requiring intervention.
For example, a patient presenting with severe abdominal pain, elevated amylase and lipase, and evidence of pancreatic necrosis on CT scan would require immediate fluid resuscitation, pain control, and possibly surgical debridement or other intervention based on the severity and patient presentation. Continuous monitoring is essential throughout the patient’s stay.
Q 22. How do you utilize diagnostic imaging in your clinical decision-making?
Diagnostic imaging plays a crucial role in guiding my clinical decision-making in hospital medicine. I use it to confirm diagnoses, assess disease severity, and monitor treatment response. My approach is tailored to the specific clinical scenario, always considering the potential risks and benefits of each modality.
- Chest X-ray: A common initial step for patients with respiratory complaints, evaluating for pneumonia, pulmonary edema, or pneumothorax. For example, a patient presenting with shortness of breath might have a chest x-ray revealing a large pleural effusion, prompting further investigation with a CT scan and consideration of thoracentesis.
- CT Scan: Essential for evaluating trauma, strokes (both ischemic and hemorrhagic), abdominal pain, and infections. For instance, a patient with sudden-onset weakness on one side of their body would undergo a CT head without contrast to rule out a hemorrhagic stroke before receiving thrombolytic therapy.
- Ultrasound: A point-of-care tool useful for assessing fluid collections, evaluating vascular access, and guiding procedures like paracentesis or thoracentesis. For example, bedside ultrasound can quickly confirm the presence of a large pericardial effusion in a patient with cardiac tamponade, enabling rapid intervention.
- MRI: Provides superior soft tissue detail, particularly useful for neurological conditions, musculoskeletal injuries, and certain abdominal pathologies. I use MRI for evaluating patients with suspected multiple sclerosis or complex spinal injuries, for example.
I always correlate imaging findings with the patient’s clinical presentation, laboratory data, and other diagnostic tests to formulate a comprehensive diagnosis and treatment plan. Over-reliance on imaging alone is avoided, emphasizing a holistic approach to patient care.
Q 23. Discuss your experience with electronic health records (EHRs).
My experience with electronic health records (EHRs) is extensive. I’m proficient in using multiple EHR systems and utilize them for documentation, order entry, results review, and communication. I understand the importance of accurate and timely documentation to ensure optimal patient care and continuity of care between providers.
I utilize EHR features such as:
- Order entry: Prescribing medications, ordering laboratory tests and diagnostic imaging, and requesting consultations all efficiently through the system.
- Result review: Efficiently reviewing lab results, imaging reports, and other data to promptly assess changes in the patient’s condition and make appropriate adjustments to the treatment plan.
- Progress notes: Creating comprehensive and detailed notes that clearly communicate the patient’s condition, treatment plan, and response to interventions. This ensures clear communication with other members of the healthcare team.
- Secure messaging: Communicating with colleagues, consultants, and other healthcare providers in a secure and HIPAA-compliant manner.
While EHRs offer significant advantages, I also recognize their limitations, such as potential for documentation errors and time constraints that may impact direct patient interaction. I actively strive to mitigate these challenges by implementing strategies such as template use and efficient note writing techniques. Ultimately, I believe in using the EHR as a tool to enhance, not hinder, quality patient care.
Q 24. What is your approach to managing a patient with an acute stroke?
Managing a patient with an acute stroke is a time-critical situation requiring immediate action. My approach follows established guidelines and prioritizes rapid assessment and intervention.
The steps involve:
- Rapid neurological assessment: Using the NIH Stroke Scale to quantify the severity of neurological deficits.
- Brain imaging: Ordering a non-contrast CT scan of the head to differentiate between ischemic and hemorrhagic stroke. This is crucial as treatment differs dramatically.
- Time is brain: If an ischemic stroke is suspected, I immediately initiate the process for thrombolysis (tissue plasminogen activator or tPA) if within the appropriate time window and eligibility criteria are met. This involves close monitoring of vital signs, neurological status and potential complications.
- Supportive care: Includes management of blood pressure, glucose control, and prevention of complications like aspiration pneumonia, deep vein thrombosis, and pressure ulcers.
- Neurological consultation: Consulting with a neurologist for ongoing management and consideration of other interventions like endovascular thrombectomy for large vessel occlusions.
- Rehabilitation: Early initiation of physical, occupational, and speech therapy is crucial for optimal patient recovery.
I carefully weigh the benefits and risks of each intervention, considering factors such as patient age, comorbidities, and the time elapsed since symptom onset. Effective communication with the patient and family is crucial throughout this process.
Q 25. How do you ensure appropriate escalation and consultation when needed?
Appropriate escalation and consultation are essential for optimal patient care. My approach is proactive, relying on clear communication and defined pathways for seeking expert opinion when necessary.
I escalate care when:
- Clinical deterioration: Significant changes in vital signs, mental status, or other concerning symptoms.
- Uncertain diagnosis: Difficulty in establishing a definitive diagnosis despite initial workup.
- Complex management: Cases requiring specialized expertise, such as cardiac arrest, severe sepsis, or complex surgical procedures.
- Therapeutic limitations: When the patient’s condition exceeds my scope of practice or expertise.
I use various methods to initiate consultations and escalations:
- Direct communication: Calling specialists directly to discuss the case and request their input.
- Electronic consult requests: Utilizing the EHR’s consult system for formal requests with clear documentation.
- Rapid Response Team: Activating the Rapid Response Team for patients exhibiting signs of clinical instability.
- Code Blue/Medical Emergency Response System: For life-threatening emergencies such as cardiac arrest or respiratory failure.
Throughout the escalation process, I ensure clear and concise communication regarding the patient’s condition, the reasons for escalation, and any immediate actions already taken.
Q 26. Describe your understanding of the principles of shared decision-making.
Shared decision-making is a cornerstone of my practice. It involves a collaborative approach where I partner with the patient and their family to make informed decisions about their healthcare. I believe that patients have the right to participate actively in the decision-making process, and their preferences, values, and beliefs should be respected.
My approach involves:
- Providing information: Clearly explaining the patient’s condition, diagnostic findings, treatment options, risks and benefits of each option, and likely outcomes in an understandable manner.
- Exploring preferences and values: Understanding the patient’s goals and priorities, as well as their concerns and preferences. This involves active listening and empathetic communication.
- Collaborative decision-making: Working together with the patient to weigh the pros and cons of different options and arrive at a plan that aligns with their individual needs and values.
- Shared responsibility: Sharing responsibility for the care plan, ensuring that the patient feels empowered and in control of their healthcare journey.
For example, I might discuss with a patient the risks and benefits of different treatment options for heart failure, considering their preferences for lifestyle changes, medication tolerance and quality of life expectations. This ensures the chosen treatment plan is not only medically sound but also aligns with the patient’s wishes and values.
Q 27. Explain your experience with managing a patient with severe hyperkalemia.
Managing severe hyperkalemia (high potassium levels in the blood) requires immediate attention as it can lead to life-threatening cardiac arrhythmias. My approach is based on rapid stabilization and correction of the electrolyte imbalance.
My approach involves:
- Assessment and stabilization: Immediately assessing the patient’s cardiac rhythm (ECG) for signs of hyperkalemia, such as peaked T waves, widened QRS complex, and cardiac arrest. I initiate continuous cardiac monitoring.
- Urgent treatment: Administering intravenous calcium gluconate to stabilize the myocardium, protecting against cardiac arrhythmias. This is often followed by insulin and glucose to shift potassium intracellularly. Sodium bicarbonate may also be considered in specific cases.
- Removing potassium: Using diuretics (like furosemide) to promote urinary potassium excretion; dialysis is employed in severe cases or when other measures are ineffective.
- Identifying the cause: A thorough investigation is conducted to find and address the underlying cause of hyperkalemia, such as acute kidney injury, medication side effects (ACE inhibitors, potassium-sparing diuretics), or rhabdomyolysis.
- Monitoring: Close monitoring of serum potassium levels, ECG, and other vital signs is crucial to ensure effective treatment and prevent recurrence.
It’s important to act swiftly and decisively as delays in treatment can have fatal consequences. I always work closely with other specialists, such as nephrology, if required to ensure the most comprehensive care.
Q 28. What is your approach to managing a patient with a suspected deep vein thrombosis?
Suspected deep vein thrombosis (DVT) requires prompt evaluation and management to prevent potentially life-threatening pulmonary embolism (PE). My approach is guided by clinical probability and diagnostic testing.
My steps include:
- Clinical assessment: Evaluating the patient’s risk factors for DVT (e.g., recent surgery, prolonged immobility, malignancy, inherited thrombophilia) and assessing for clinical signs and symptoms, including unilateral leg pain, swelling, warmth, and erythema.
- Diagnostic testing: Ordering a compression ultrasonography of the lower extremities to confirm or exclude DVT. D-dimer testing might be considered initially, but it’s not used as a definitive test to rule out DVT. It has a high negative predictive value in low-risk patients.
- Initiating anticoagulation: If a DVT is confirmed, I typically initiate anticoagulation therapy with heparin (unfractionated or low-molecular-weight heparin) followed by oral anticoagulants (e.g., warfarin, direct oral anticoagulants like rivaroxaban or apixaban) for a period of time determined based on the specific risk factors and treatment response.
- Monitoring for complications: Closely monitoring for signs and symptoms of PE, bleeding complications, and other adverse events associated with anticoagulation therapy.
- Consultations: Involving hematology if necessary, particularly in patients with complex cases, recurrent DVT, or unusual risk factors.
The choice of anticoagulation regimen and duration is individualized based on patient-specific factors. The overarching goal is to prevent further clot formation and reduce the risk of PE while minimizing bleeding complications. I emphasize patient education about the importance of adherence to therapy and the recognition of warning signs.
Key Topics to Learn for Hospital Medicine Interview
- Acute and Chronic Disease Management: Understanding the complexities of managing both acute and chronic conditions concurrently, including prioritization of care and resource allocation.
- Evidence-Based Medicine & Critical Appraisal: Applying the latest research findings to patient care and critically evaluating the strength of evidence in medical literature. This includes understanding study designs and limitations.
- Teamwork & Communication: Demonstrating experience in effectively collaborating with multidisciplinary teams (nurses, pharmacists, social workers, specialists) and communicating complex medical information clearly and concisely to patients and families.
- Patient Safety & Quality Improvement: Discussing strategies for improving patient safety and actively participating in quality improvement initiatives within a hospital setting. Examples include fall prevention and medication reconciliation.
- Inpatient Procedures & Interventions: Understanding common procedures performed in the hospital setting and the rationale behind them. This includes knowledge of indications, contraindications, and potential complications.
- Code Management & Resuscitation: Experience and knowledge of managing cardiac and respiratory arrests, including participation in resuscitation efforts and post-resuscitation care.
- Ethical Considerations & Decision-Making: Demonstrating understanding of ethical principles in hospital medicine, particularly in situations involving end-of-life care, resource allocation, and informed consent.
- Pharmacology & Therapeutics: Comprehensive knowledge of commonly used medications, including their mechanisms of action, indications, adverse effects, and interactions.
- Hospital Resource Utilization & Cost-Effectiveness: Understanding the cost implications of different treatment strategies and ways to optimize resource utilization while maintaining high-quality patient care.
- Transitions of Care & Discharge Planning: Experience in planning for safe and effective transitions of care from the hospital to other settings (e.g., skilled nursing facilities, home health care). This includes coordinating post-discharge medications and follow-up appointments.
Next Steps
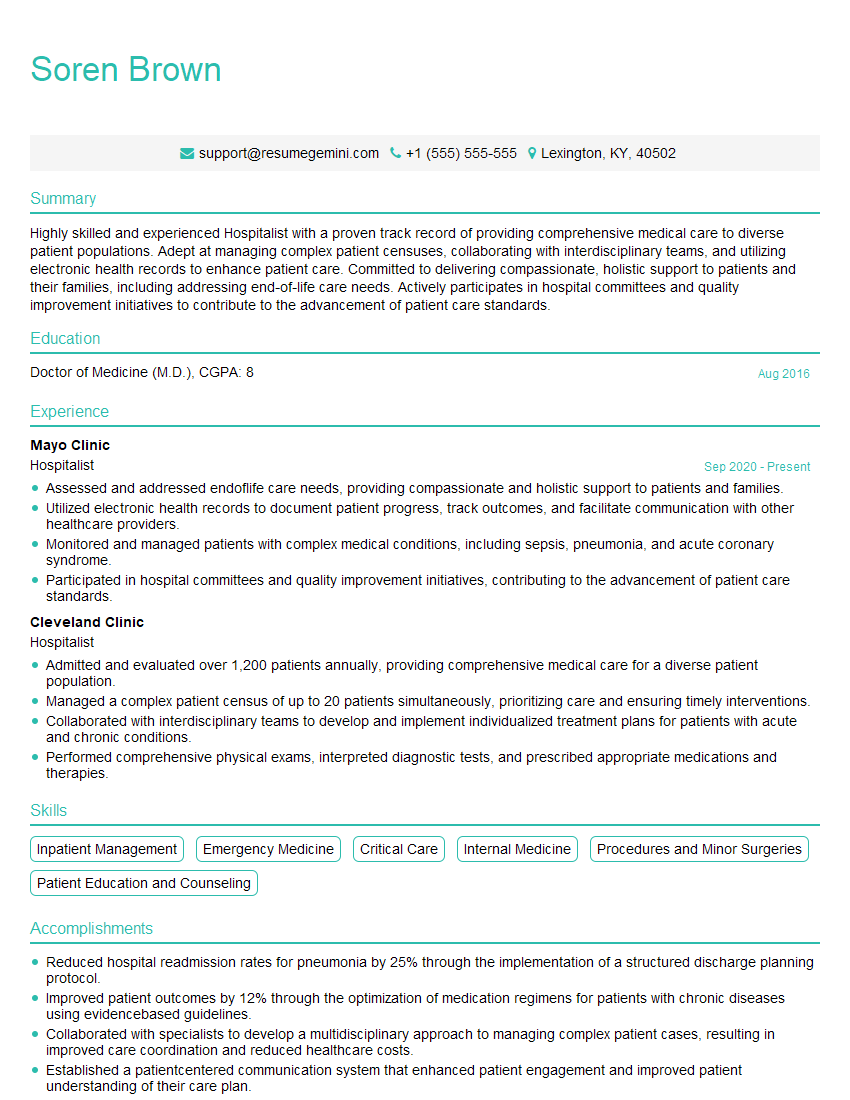
Mastering Hospital Medicine opens doors to a fulfilling and impactful career, offering diverse opportunities for specialization and leadership. A strong resume is crucial for showcasing your skills and experience to potential employers. To significantly increase your job prospects, create an ATS-friendly resume that highlights your achievements and qualifications effectively. ResumeGemini is a trusted resource that can help you build a professional and impactful resume tailored to the demands of the Hospital Medicine field. Examples of resumes specifically designed for Hospital Medicine positions are available through ResumeGemini to guide your preparation.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Interesting Article, I liked the depth of knowledge you’ve shared.
Helpful, thanks for sharing.
Hi, I represent a social media marketing agency and liked your blog
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?