The right preparation can turn an interview into an opportunity to showcase your expertise. This guide to Ambulatory Medicine interview questions is your ultimate resource, providing key insights and tips to help you ace your responses and stand out as a top candidate.
Questions Asked in Ambulatory Medicine Interview
Q 1. Describe your experience managing chronic conditions in an ambulatory setting.
Managing chronic conditions in an ambulatory setting requires a proactive and holistic approach. It’s not just about treating acute exacerbations; it’s about empowering patients to manage their conditions effectively on a day-to-day basis. This involves a strong emphasis on patient education, regular monitoring, and close collaboration with other healthcare providers.
My experience includes developing and implementing individualized care plans for patients with conditions such as diabetes, hypertension, heart failure, and asthma. These plans incorporate regular monitoring of vital signs, lab work, and medication adherence, along with adjustments to treatment based on patient progress. For example, a patient with poorly controlled diabetes might require adjustments to their insulin regimen, dietary counseling, and increased frequency of blood glucose monitoring. We use tools like patient portals and telehealth to facilitate communication and monitor progress between appointments.
Furthermore, I actively involve patients in their care by discussing their treatment goals, addressing concerns, and helping them understand how to self-manage their conditions. Regular follow-ups and proactive interventions are key to preventing complications and hospitalizations. For instance, a patient with heart failure might benefit from regular weight monitoring, sodium restriction education, and timely intervention if signs of worsening heart failure appear.
Q 2. Explain your approach to patient education in ambulatory care.
Patient education is a cornerstone of effective ambulatory care. My approach is centered on patient-centered communication and shared decision-making. It’s not enough to simply tell a patient what to do; I strive to ensure they understand *why* they need to do it and how it will improve their health. I tailor my educational approach to each patient’s individual learning style and health literacy level.
I use a variety of methods to facilitate learning, including verbal explanations, written materials (brochures, handouts), visual aids (diagrams, charts), and interactive tools (educational videos, online resources). I also encourage patients to ask questions and actively participate in the discussion. For example, when explaining medication regimens, I not only explain the dosage and timing but also the purpose of the medication, common side effects, and how to manage them. I always check for understanding and use teach-back methods to ensure information is retained. Furthermore, I leverage the patient portal to provide access to educational resources, appointment reminders, and secure messaging for ongoing communication and support.
For patients with multiple chronic conditions, I create a structured, organized educational plan that prioritizes the most urgent needs first. I break down complex information into smaller, manageable chunks, ensuring that they have a clear understanding of each aspect of their care. We establish realistic goals, gradually building their knowledge and self-management skills over time.
Q 3. How do you prioritize patients with multiple health concerns in an ambulatory setting?
Prioritizing patients with multiple health concerns requires a systematic approach. I utilize a framework that considers urgency, potential for complications, and impact on quality of life. A prioritized list helps to ensure all concerns are addressed, but in an efficient order. I start with a comprehensive assessment of the patient’s overall health status, identifying the most pressing issues.
- Urgency: Conditions requiring immediate attention, such as acute infections or uncontrolled pain, take precedence.
- Potential for complications: Conditions with a high risk of serious complications, such as uncontrolled diabetes or severe hypertension, are also prioritized.
- Impact on quality of life: Conditions significantly impacting a patient’s daily activities and well-being are given due consideration.
For instance, a patient with uncontrolled diabetes, hypertension, and osteoarthritis might have their diabetes management prioritized due to the immediate risk of complications like diabetic ketoacidosis. However, the management plan needs to address the other conditions to improve the patient’s overall health and quality of life. I utilize tools like problem lists and care plans in the EHR to track progress and ensure all aspects are addressed comprehensively.
Q 4. Describe your experience with electronic health records (EHRs) in ambulatory care.
Electronic Health Records (EHRs) are indispensable in ambulatory care. My experience with EHRs spans several systems, including Epic and Cerner. I am proficient in using EHRs for various functions, including patient registration, chart documentation, medication reconciliation, order entry, result review, and communication with other healthcare providers. Efficient EHR utilization is a crucial skill for streamlining workflow and improving patient care.
I use the EHR’s functionality for proactive care, such as generating preventive health reminders, tracking patient progress on chronic disease management plans, identifying patients due for preventive screenings, and monitoring lab results for potential abnormalities. For example, automated alerts in the EHR system can help identify patients with uncontrolled hypertension who require urgent attention. The EHR also allows for efficient communication with specialists, ensuring seamless coordination of care.
However, EHRs also present challenges, such as documentation burden and potential for system downtime. I use efficient charting techniques, such as templating and dictation, to minimize documentation time while ensuring completeness and accuracy. I also stay informed on updates and new functionalities to optimize my use of the system.
Q 5. How do you handle difficult or challenging patients in an ambulatory setting?
Handling difficult or challenging patients requires empathy, patience, and effective communication skills. It’s crucial to remember that challenging behaviors often stem from underlying medical, psychological, or social issues. My approach involves active listening, validating the patient’s feelings, and attempting to understand their perspective.
I employ strategies such as motivational interviewing to help patients explore their concerns and identify solutions. Clear, concise communication is paramount, avoiding medical jargon and ensuring the patient understands the information provided. If a patient is consistently disruptive or non-compliant, I may involve social workers, behavioral health specialists, or other members of the care team to develop a collaborative approach to addressing the underlying issues. Setting clear boundaries while maintaining respect is important. If necessary, I may refer the patient to other healthcare professionals better equipped to address their specific needs. For example, if a patient exhibits signs of significant depression or anxiety, I would recommend referral to a psychiatrist or therapist.
Documentation is critical in these situations, accurately recording interactions and any interventions undertaken. This documentation helps ensure continuity of care and protects both the patient and the healthcare provider.
Q 6. What is your experience with coordinating care between specialists and other healthcare providers?
Coordinating care between specialists and other healthcare providers is essential for optimal patient outcomes. I use several strategies to ensure seamless communication and collaboration. This often involves facilitating efficient communication through the EHR, making referrals, and actively participating in care conferences.
The EHR facilitates communication through secure messaging, allowing for prompt exchange of information with specialists. I use this feature to transmit relevant patient data, including test results, imaging reports, and clinical notes, to expedite the referral process. Before referring a patient, I clearly articulate the patient’s needs and clinical questions, ensuring that the specialist receives all necessary information. I also actively follow-up on specialist appointments, reviewing reports and ensuring timely integration of recommendations into the patient’s care plan. I actively participate in care conferences when appropriate, facilitating discussion among providers, ensuring a coordinated approach to the patient’s overall care. Finally, a well-written referral summary ensures clarity and efficiency in the transition of care.
Effective communication ensures that everyone is on the same page and working towards the same goal. This multidisciplinary approach improves the quality of care and reduces the potential for medical errors or conflicting recommendations.
Q 7. Describe a time you had to make a quick clinical decision in an ambulatory setting.
One instance involved a patient presenting with sudden-onset chest pain. While initially assessing as stable, their electrocardiogram (ECG) revealed significant ST-segment elevation in the inferior leads, suggestive of an acute myocardial infarction (heart attack). The ambulatory setting doesn’t typically have the immediate resources of a hospital emergency room.
My quick clinical decision involved immediately activating the emergency medical services (EMS). I ensured the patient received oxygen therapy, while simultaneously contacting the local emergency department to alert them about the impending arrival and ensure readiness for immediate intervention. The rapid response and coordination with the EMS and hospital team likely saved the patient’s life. The incident underscored the importance of rapid assessment and timely decision-making in recognizing and managing potentially life-threatening situations, even within the limitations of an ambulatory care setting. Regular review of ECG interpretation and cardiac emergency protocols is crucial for maintaining clinical competency in this area.
Q 8. How do you stay current with the latest advancements in ambulatory care?
Staying current in ambulatory care requires a multifaceted approach. It’s not just about reading journals; it’s about active engagement with the medical community.
- Professional Organizations: I actively participate in organizations like the American Academy of Family Physicians (AAFP) or the American College of Physicians (ACP), attending conferences and webinars to learn about the latest research and best practices. These events often feature presentations from leading experts and offer valuable networking opportunities.
- Peer-Reviewed Journals: I regularly review journals such as JAMA, Annals of Internal Medicine, and specialty-specific publications to stay abreast of new research findings and clinical guidelines. I focus on articles related to my areas of expertise and those addressing emerging trends in ambulatory care.
- Continuing Medical Education (CME): I diligently complete required CME credits through online courses, workshops, and conferences. This ensures my knowledge base remains up-to-date and aligned with current standards of care. I prioritize CME focusing on areas where I see a need to enhance my skills, such as managing chronic disease or utilizing new diagnostic technologies.
- Professional Networks: I maintain a strong professional network, engaging in discussions with colleagues, attending local medical society meetings, and participating in online forums to share experiences and learn from others.
For example, recently I attended a webinar on the latest guidelines for managing hypertension, which significantly impacted my approach to patient care. This proactive approach ensures I’m always prepared to provide the highest quality of care.
Q 9. Explain your understanding of preventative care in an ambulatory setting.
Preventative care in an ambulatory setting is crucial for improving patient outcomes and reducing healthcare costs. It involves proactive measures aimed at preventing disease or detecting it early when treatment is most effective.
- Routine Check-ups: Regular physical exams, including screenings based on age and risk factors (e.g., blood pressure, cholesterol, cancer screenings), are fundamental. These allow for early detection of potential problems and offer opportunities for health education and lifestyle counseling.
- Immunizations: Providing and promoting age-appropriate vaccinations against preventable diseases like influenza, pneumonia, and shingles is a vital aspect of preventative care. I emphasize the importance of vaccination to patients and address any concerns they may have regarding vaccine safety.
- Lifestyle Counseling: This involves addressing modifiable risk factors like smoking, unhealthy diet, lack of exercise, and excessive alcohol consumption. I work with patients to set realistic goals for behavior change, providing support and resources as needed. For instance, I might refer a patient to a smoking cessation program or a registered dietitian.
- Chronic Disease Management: For patients with conditions like diabetes or hypertension, preventative care focuses on managing their conditions to prevent complications. This involves regular monitoring, medication management, and education to empower patients to actively participate in their care.
Imagine a patient with a family history of heart disease. Through regular check-ups, we can monitor their cholesterol levels and blood pressure, and implement lifestyle changes or medications to minimize their risk of a cardiac event. This proactive approach significantly reduces long-term health complications.
Q 10. How do you handle emergencies or urgent situations in an ambulatory setting?
Handling emergencies or urgent situations in an ambulatory setting requires a calm, efficient, and systematic approach.
- Rapid Assessment: The first step is to quickly assess the patient’s condition to determine the severity of the situation. This involves evaluating vital signs, identifying symptoms, and determining the potential life-threatening nature of the emergency.
- Immediate Intervention: Depending on the assessment, immediate intervention may involve administering oxygen, controlling bleeding, or initiating cardiopulmonary resuscitation (CPR).
- Activation of Emergency Medical Services (EMS): If the situation necessitates immediate advanced medical care, I promptly activate EMS and provide them with all necessary information about the patient’s condition. This includes clearly communicating symptoms, vital signs, and any interventions already undertaken.
- Stabilization and Transfer: Before EMS arrives, I focus on stabilizing the patient to the best of my ability, ensuring their safety and minimizing further complications. This often involves close monitoring of vital signs and addressing immediate threats.
- Post-Emergency Documentation: Meticulous documentation of the entire event, including the assessment, interventions, and the EMS response, is critical for legal and medical record-keeping purposes.
For example, if a patient experiences a sudden loss of consciousness, I would immediately assess their airway, breathing, and circulation, initiating CPR if necessary while simultaneously calling for emergency assistance. This rapid response and coordination with EMS are essential to ensure the patient receives timely and appropriate care.
Q 11. What is your approach to managing medication reconciliation in ambulatory care?
Medication reconciliation is a crucial process in ambulatory care, ensuring that patients receive the correct medications at the right dose, while minimizing the risk of adverse drug events. This involves a systematic process to compare the patient’s current medication list with their prescribed medications and identify any discrepancies.
- Comprehensive Medication List: I begin by obtaining a complete and accurate medication list from the patient, including over-the-counter medications, supplements, and herbal remedies. This often involves asking patients to bring all their medications to the appointment.
- Comparison and Verification: The patient’s self-reported list is then compared with their medical records and any information available from other healthcare providers involved in their care. This step ensures accuracy and identifies any potential discrepancies.
- Discrepancy Resolution: Any discrepancies, such as missing medications, incorrect dosages, or potential drug interactions, are carefully investigated. This might involve contacting other healthcare providers or reviewing prior medical records to clarify information.
- Patient Education: I clearly explain the purpose and dosage of each medication, along with potential side effects and interactions. Patients are encouraged to ask questions and express any concerns they may have.
- Documentation: All aspects of the medication reconciliation process are meticulously documented in the patient’s medical record, including the medications identified, any discrepancies, and the actions taken to resolve them.
Let’s say a patient reports taking a medication not listed in their chart. I would carefully investigate to determine if it’s a new prescription, if the information in the chart is outdated, or if the medication was obtained from another provider. Once the information is verified, I ensure the chart reflects the current medication regimen and discuss potential drug interactions with the patient.
Q 12. Describe your experience with patient safety protocols in ambulatory care.
Patient safety protocols in ambulatory care are paramount. My approach incorporates several key elements:
- Hand Hygiene: I rigorously follow hand hygiene protocols before and after each patient interaction, using soap and water or an alcohol-based hand sanitizer. This simple yet effective practice significantly reduces the spread of infection.
- Infection Control: Strict adherence to infection control measures, including proper sterilization of equipment and use of personal protective equipment (PPE), is crucial in minimizing the risk of cross-contamination. This includes following guidelines for managing patients with suspected or confirmed infections.
- Medication Safety: Following the ‘five rights’ of medication administration (right patient, right drug, right dose, right route, right time) is essential. Double-checking medication orders and confirming patient allergies are integral parts of this process. I frequently review the patient’s medication list for potential interactions.
- Fall Prevention: Identifying and addressing fall risks among patients, especially those with mobility issues, is a priority. This could involve implementing strategies to improve their mobility and environmental modifications to their home.
- Error Reporting and Analysis: Reporting and analyzing near misses and medication errors is critical for identifying systemic weaknesses and implementing corrective actions. This proactive approach to error prevention is vital in creating a safe environment.
For instance, if I notice a patient has difficulty walking, I would assess their risk of falling and discuss appropriate modifications, such as using assistive devices or recommending physical therapy to improve their balance and stability.
Q 13. How do you utilize diagnostic testing results to inform patient care?
Diagnostic testing results are crucial for informing patient care. My approach involves a systematic process:
- Review and Interpretation: I carefully review the results, taking into account the patient’s clinical presentation and medical history. I ensure I understand the implications of the findings within the context of the patient’s overall health.
- Correlation with Clinical Findings: The test results are correlated with the patient’s symptoms, physical examination findings, and other diagnostic information. This holistic approach helps avoid misinterpretations.
- Differential Diagnosis: Based on the results, I refine my differential diagnosis, considering various possible explanations for the patient’s condition. The tests help narrow down the possibilities and guide further investigations.
- Treatment Plan Development: The results directly inform the development of a tailored treatment plan. This might involve initiating or adjusting medications, recommending further investigations, or referring the patient to a specialist.
- Patient Communication: I clearly and concisely communicate the results to the patient in a way that they understand, explaining the implications and answering any questions they may have. Complex findings are explained in simple terms, ensuring patient comprehension.
For example, if a patient has abnormal liver function tests, I would review the results, consider their history, and order further tests such as an ultrasound to determine the cause (e.g., liver disease, medication side effect). Based on the findings, I would then develop an appropriate treatment plan.
Q 14. What is your approach to communicating with patients and their families?
Effective communication with patients and their families is crucial in ambulatory care. My approach involves:
- Active Listening: I begin by actively listening to the patient’s concerns, allowing them to fully express their symptoms and worries in a non-judgmental environment. This builds trust and ensures I have a complete understanding of their perspective.
- Clear and Concise Explanations: I explain medical information in a clear, concise, and easy-to-understand manner, avoiding medical jargon. I make sure the patient comprehends the diagnosis, treatment plan, and potential prognosis.
- Shared Decision-Making: I involve the patient in the decision-making process, discussing treatment options and their potential benefits and risks. This collaborative approach empowers the patient and enhances their adherence to the treatment plan.
- Empathy and Compassion: I approach each interaction with empathy and compassion, acknowledging the patient’s emotional and psychological well-being. I recognize that illness can be stressful and strive to create a supportive environment.
- Family Involvement: When appropriate, I involve the patient’s family in discussions, particularly if they are playing a crucial role in the patient’s care. This fosters a collaborative approach to their healthcare.
For example, I might use visual aids like diagrams or flowcharts to explain complex concepts to patients. I always check for understanding and answer any questions until the patient feels comfortable with the information.
Q 15. Explain your understanding of healthcare regulations and compliance in ambulatory care.
Healthcare regulations and compliance in ambulatory care are paramount to ensuring patient safety, maintaining ethical standards, and avoiding legal repercussions. This involves a multifaceted understanding of numerous federal and state laws, as well as accrediting body standards.
- HIPAA (Health Insurance Portability and Accountability Act): This is foundational, dictating the privacy and security of protected health information (PHI). We must adhere strictly to protocols for data storage, access control, and patient authorization for information release.
- Medicare and Medicaid regulations: Ambulatory care centers often participate in these government programs, requiring meticulous documentation, coding, and billing practices to ensure accurate reimbursement and avoid fraud and abuse penalties. This involves understanding the specific requirements for each service provided.
- State licensing and certification: Each state has its own regulations for operating ambulatory care facilities, including requirements for staffing, equipment, and infection control. Compliance necessitates staying updated on any changes in state-specific regulations.
- CLIA (Clinical Laboratory Improvement Amendments): If the clinic performs laboratory tests, strict adherence to CLIA regulations is crucial. This covers quality control, proficiency testing, and personnel qualifications.
- Accreditation: Organizations like The Joint Commission (TJC) offer accreditation demonstrating compliance with nationally recognized standards. Accreditation is often a requirement for participation in Medicare and Medicaid programs and enhances the clinic’s reputation.
Non-compliance can lead to severe penalties, including fines, loss of licensing, and even legal action. Therefore, regular training, audits, and proactive measures to ensure up-to-date knowledge of regulations are essential.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you effectively manage your time and workload in a busy ambulatory setting?
Time management in a busy ambulatory setting is crucial. I utilize several strategies to effectively manage my workload.
- Prioritization: I use a system to prioritize tasks based on urgency and importance, focusing first on patients with the most critical needs or time-sensitive appointments.
- Time Blocking: I allocate specific time slots for different activities, such as patient appointments, chart reviews, documentation, and administrative tasks. This ensures I dedicate sufficient time to each.
- Delegation: Where appropriate, I delegate tasks to qualified staff members, such as medical assistants or nurses, to optimize workflow efficiency.
- Efficient Scheduling: Working closely with the scheduling team, we aim for an efficient appointment flow to minimize patient wait times and maximize clinic throughput. This may involve using a combination of appointment types (e.g., short visits for follow-ups, longer visits for complex cases).
- Technology: Leveraging electronic health records (EHRs) and other technologies streamlines administrative tasks, enabling quicker access to information and reducing paperwork.
For example, if a patient needs a referral, I’ll prioritize completing the referral request immediately to avoid delays in their care. I also block out specific times for documentation to prevent it from piling up and interfering with patient care. Regular review and adjustment of my time-management system ensures ongoing effectiveness.
Q 17. Describe your experience with interdisciplinary teamwork in an ambulatory setting.
Interdisciplinary teamwork is fundamental to successful ambulatory care. My experience has shown its value in providing holistic patient care and improving outcomes.
In my previous role, I worked closely with nurses, medical assistants, social workers, pharmacists, and physical therapists. We held regular team meetings to discuss patient cases, coordinate care plans, and address any challenges. For example, a diabetic patient with poor wound healing required collaboration among myself, the nurse, and the wound care specialist to optimize treatment. The nurse monitored blood sugars, I managed medication, and the specialist provided advanced wound care. Open communication was key. We used shared electronic health records to facilitate information sharing and maintain up-to-date progress notes, ensuring everyone was on the same page.
Effective teamwork led to better patient outcomes, improved patient satisfaction, and a more efficient workflow. It allowed us to leverage the expertise of each team member, creating a synergistic effect that improved the overall quality of care.
Q 18. How do you handle ethical dilemmas in ambulatory care?
Ethical dilemmas are unavoidable in ambulatory care. My approach involves careful consideration of relevant ethical principles, including patient autonomy, beneficence, non-maleficence, and justice.
- Clearly define the dilemma: Identify the key ethical conflict and involved parties.
- Gather information: Obtain all relevant facts, considering the patient’s perspective, medical records, and applicable regulations.
- Explore options: Consider alternative courses of action, weighing the potential benefits and risks to the patient and others involved.
- Consult colleagues and resources: Seek advice from trusted colleagues, ethical committees, or relevant professional guidelines.
- Document thoroughly: Maintain detailed records of the decision-making process, the chosen course of action, and the rationale.
For instance, a patient may refuse a recommended treatment despite the potential for serious health consequences. This necessitates respecting patient autonomy while simultaneously attempting to educate them about the risks and benefits. A careful and compassionate discussion, often involving family members if appropriate, is crucial to navigate this ethical challenge, with appropriate documentation ensuring transparency and protecting all involved.
Q 19. Describe a time you had to deal with a patient’s dissatisfaction in an ambulatory setting.
I once had a patient who was deeply dissatisfied with a perceived long wait time for an appointment and the subsequent brevity of the consultation.
My initial response was to actively listen to their concerns without interrupting. I acknowledged their frustration and apologized for the inconvenience. I then explained the factors contributing to the wait time (e.g., unexpected emergencies, staffing shortages).
To address the brevity of the appointment, I offered to schedule a follow-up visit to discuss their concerns in more detail. I proactively checked if there were any other unmet needs or questions that could be addressed. I ensured they had all necessary information, including contact details for further assistance.
Through open communication and a sincere effort to understand and address their dissatisfaction, I was able to de-escalate the situation and ultimately improve the patient’s experience. I also used this experience to identify areas for improvement in our clinic’s workflow and communication strategies.
Q 20. What are some key performance indicators (KPIs) you track in ambulatory care?
Key performance indicators (KPIs) are vital for evaluating the effectiveness and efficiency of ambulatory care practices. The specific KPIs monitored will vary depending on the clinic’s goals and patient population, but some common ones include:
- Patient satisfaction scores: Measured through surveys, these reflect patient experiences and identify areas for improvement.
- Appointment wait times: Tracking this helps identify and address bottlenecks in the scheduling process.
- Patient no-show rates: Monitoring this helps implement strategies to reduce missed appointments.
- Timeliness of referrals: Ensuring timely referrals optimizes patient care and avoids delays in treatment.
- Medication adherence rates: This indicator helps assess the success of patient education and intervention programs.
- Cost per visit: Tracking this helps monitor efficiency and identify opportunities for cost reduction.
- Patient throughput: This measures the number of patients seen per unit of time, reflecting clinic capacity and efficiency.
By regularly monitoring these KPIs, we can identify areas of strength and weakness, enabling data-driven improvements in the quality and efficiency of care.
Q 21. How do you address healthcare disparities in your ambulatory care practice?
Addressing healthcare disparities is an ethical imperative in ambulatory care. It requires a multi-pronged approach focusing on identifying and mitigating factors that contribute to unequal access to and quality of care.
- Cultural competency training: All staff members need training on cultural sensitivity and awareness, ensuring effective communication and understanding of diverse patient needs and beliefs.
- Language access services: Providing interpretation and translation services ensures effective communication with patients who speak different languages.
- Community outreach: Engaging with community organizations and leaders helps increase awareness of available services and address barriers to access in underserved communities.
- Financial assistance programs: Offering sliding-scale fees or connecting patients with financial assistance programs helps reduce financial barriers to care.
- Transportation assistance: Providing information or assistance with transportation helps ensure access for patients who lack reliable transportation.
- Data collection and analysis: Regularly reviewing patient data to identify disparities in access to and quality of care helps guide targeted interventions.
For instance, I might proactively inquire about transportation challenges during patient intake or offer information about available community resources. Understanding the root causes of disparities – such as language barriers, lack of insurance, or limited health literacy – is key to designing effective interventions to achieve equitable healthcare for all.
Q 22. Explain your understanding of population health management in an ambulatory setting.
Population health management (PHM) in an ambulatory setting focuses on improving the health outcomes of a defined patient population. It moves beyond treating individual illnesses to proactively addressing the overall health and well-being of the group. This involves identifying high-risk individuals, implementing preventative measures, and managing chronic conditions to reduce hospital readmissions and improve quality of life.
For example, we might use a risk stratification tool to identify patients with diabetes who are at high risk for complications. Then, we create a care plan incorporating regular check-ups, medication management support, lifestyle counseling, and remote monitoring. We’d also coordinate care with specialists as needed, ensuring seamless transitions between various healthcare settings.
Success is measured by tracking key performance indicators (KPIs) like the number of preventable hospitalizations, improved A1c levels in diabetic patients, or patient satisfaction scores. It requires a collaborative approach involving physicians, nurses, health educators, social workers, and data analysts.
Q 23. Describe your experience with telehealth or virtual care in an ambulatory setting.
My experience with telehealth and virtual care in an ambulatory setting has been extensive and largely positive. I’ve used telehealth for various purposes, from routine follow-up appointments and medication reviews to acute care management and chronic disease monitoring. For instance, I utilize video conferencing to conduct virtual check-ins with patients managing hypertension. This allows for convenient monitoring of blood pressure readings reported by patients using home monitoring devices, medication adherence discussions, and prompt adjustments to treatment plans as needed.
The benefits are clear: improved access to care, especially for patients in rural areas or with mobility limitations; increased patient convenience and satisfaction; and potentially reduced healthcare costs due to fewer in-person visits. However, it’s vital to ensure appropriate patient selection, maintain strong communication strategies to address potential technology barriers, and maintain the privacy and security of patient data through HIPAA-compliant platforms.
Q 24. How do you incorporate patient preferences into care planning?
Incorporating patient preferences is paramount to successful care planning. I start by actively listening to patients, understanding their values, goals, and concerns. I employ a shared decision-making model, presenting treatment options clearly and discussing the pros, cons, and potential risks associated with each.
For example, a patient with osteoarthritis might prefer physical therapy over surgery. My role is to gather information about their physical activity level, pain tolerance, and life goals to collaboratively select a care pathway best aligned with their preferences and medical needs. This might involve exploring less invasive options initially and then escalating to surgery only if necessary. Documenting these shared decisions within the electronic health record is crucial for maintaining consistency and transparency.
Q 25. What is your experience with quality improvement initiatives in ambulatory care?
I have been actively involved in several quality improvement initiatives in ambulatory care. One notable example was our participation in a project to reduce medication errors. We implemented a barcoding system for medication dispensing and improved medication reconciliation processes. This resulted in a significant decrease in medication errors, as documented through regular audits and incident reporting.
Another initiative involved improving patient wait times. Through data analysis of appointment scheduling and patient flow, we identified bottlenecks and implemented changes, like staggered appointment scheduling and improved communication with patients. This resulted in a 25% reduction in average wait times, improving patient satisfaction and clinic efficiency. The Plan-Do-Study-Act (PDSA) cycle was instrumental in guiding these efforts – testing smaller changes iteratively and measuring outcomes.
Q 26. How do you manage patient confidentiality and HIPAA compliance?
Patient confidentiality and HIPAA compliance are non-negotiable. I strictly adhere to HIPAA regulations, ensuring that all patient information is handled with utmost care and only accessed by authorized personnel. This includes secure electronic health records, password-protected computers, and adherence to strict protocols for data sharing.
Specific examples include encrypting electronic communications with patients, using secure portals for data exchange, and disposing of paper records appropriately. We conduct regular training sessions for staff on HIPAA compliance to maintain awareness of regulations and best practices. We also have procedures in place to address data breaches and security incidents, emphasizing prompt reporting and mitigation strategies.
Q 27. Describe your experience with billing and coding in an ambulatory setting.
My experience with billing and coding in an ambulatory setting is substantial. I understand the importance of accurate and timely billing to ensure reimbursement for services rendered. I am familiar with various coding systems, such as ICD-10 for diagnoses and CPT for procedures, and I regularly review and update my knowledge to stay current with changes and guidelines.
I work closely with our billing department to ensure proper documentation is maintained in patient charts, so that the codes accurately reflect the services provided. This minimizes claim denials and facilitates prompt payment. I also participate in audits to identify areas for improvement and prevent future billing errors. In cases of complex billing issues, I consult with billing specialists or compliance officers to ensure adherence to regulations.
Q 28. How do you contribute to a positive and supportive team environment in ambulatory care?
Contributing to a positive and supportive team environment is essential for providing high-quality patient care. I actively participate in team meetings, share my expertise, and offer support to colleagues. I believe in fostering open communication and collaboration, creating a space where everyone feels valued and respected.
For example, I regularly mentor junior colleagues, sharing my knowledge and providing constructive feedback. I actively participate in team-building activities, promoting camaraderie and a sense of shared purpose. I believe that a strong team is critical for effective and efficient patient care, improving both the quality of work and job satisfaction for everyone involved.
Key Topics to Learn for Ambulatory Medicine Interview
- Patient Assessment & Triage: Understanding the process of quickly and accurately assessing patient needs in an ambulatory setting, prioritizing urgency, and determining appropriate interventions.
- Chronic Disease Management: Practical application of managing common chronic conditions like diabetes, hypertension, and asthma in the ambulatory setting, including patient education and medication management.
- Preventive Care & Health Promotion: Developing strategies for promoting wellness and preventing disease through screenings, vaccinations, and lifestyle counseling.
- Electronic Health Records (EHR) Systems: Demonstrating proficiency in using EHR systems for documentation, ordering tests, and managing patient data efficiently and accurately. This includes understanding HIPAA regulations and maintaining patient privacy.
- Teamwork & Communication: Highlighting effective collaboration with nurses, other healthcare providers, and patients to ensure optimal care coordination. This includes clear and empathetic communication skills.
- Common Ambulatory Procedures & Techniques: Understanding the practical application and limitations of common procedures performed in ambulatory settings (e.g., wound care, injections, ECG interpretation).
- Pharmacology & Medication Reconciliation: Demonstrating knowledge of common medications used in ambulatory care, including their indications, contraindications, and potential adverse effects. Understanding medication reconciliation processes to avoid medication errors.
- Ethical and Legal Considerations: Understanding the ethical and legal responsibilities of healthcare professionals in an ambulatory care setting, including informed consent, patient confidentiality, and end-of-life care.
- Quality Improvement & Patient Safety: Familiarity with quality improvement methodologies and their application to enhance patient safety and outcomes in an ambulatory care setting.
Next Steps
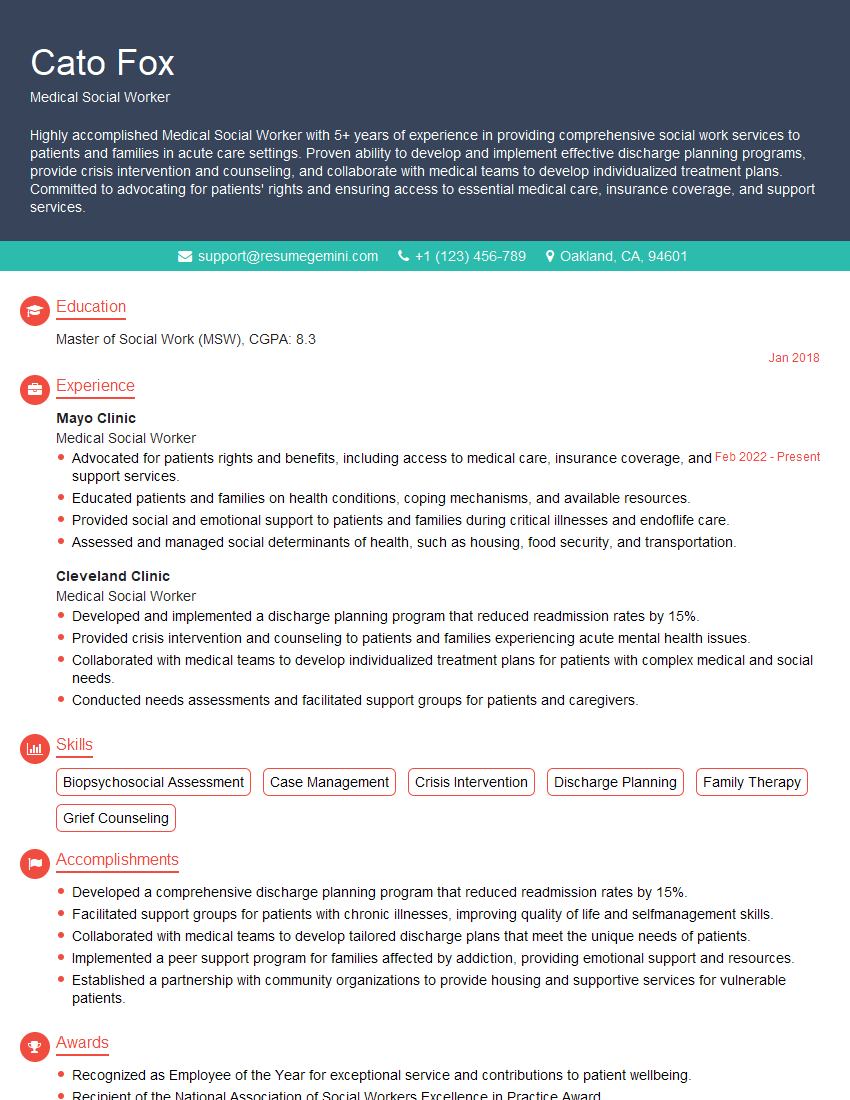
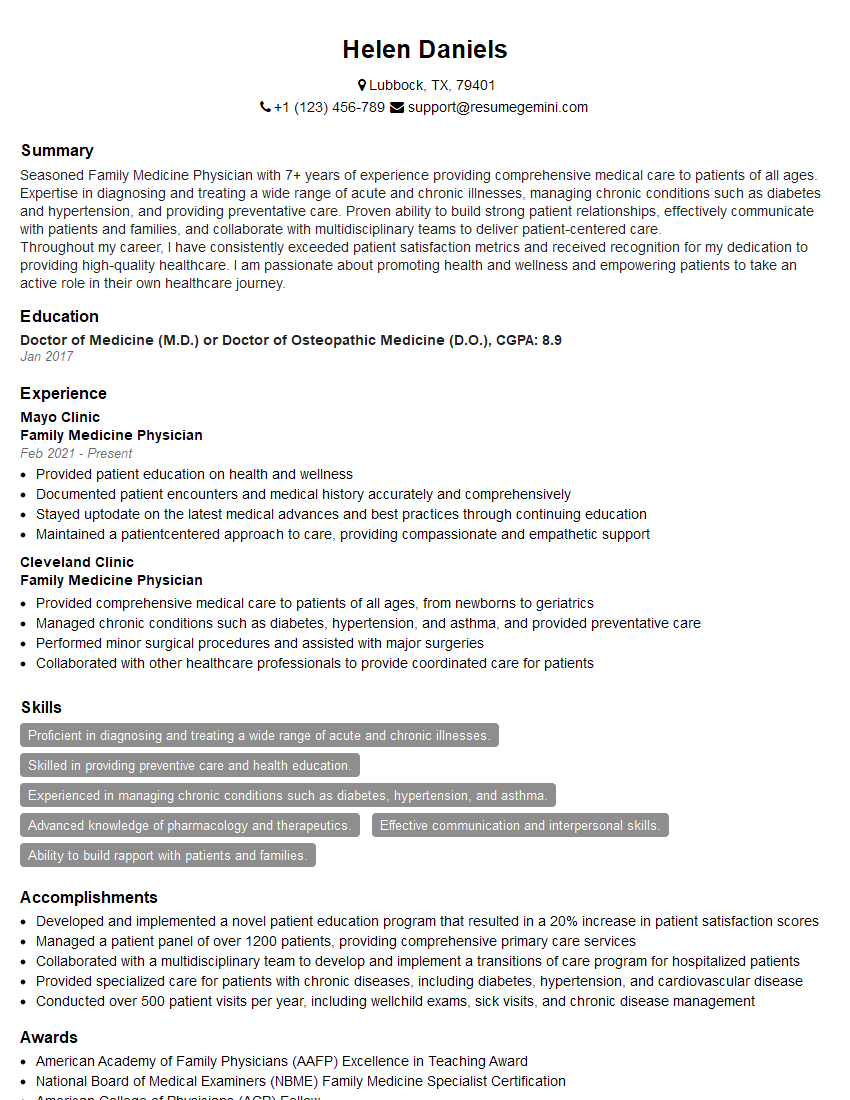
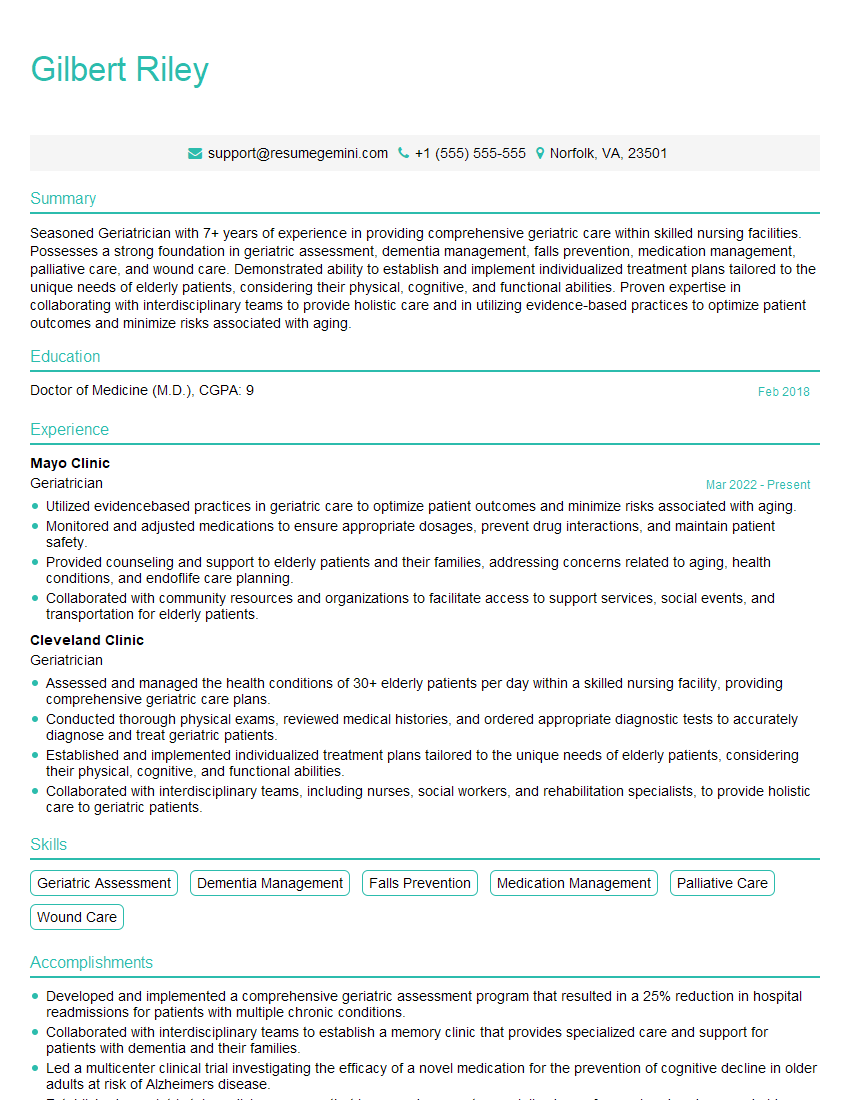
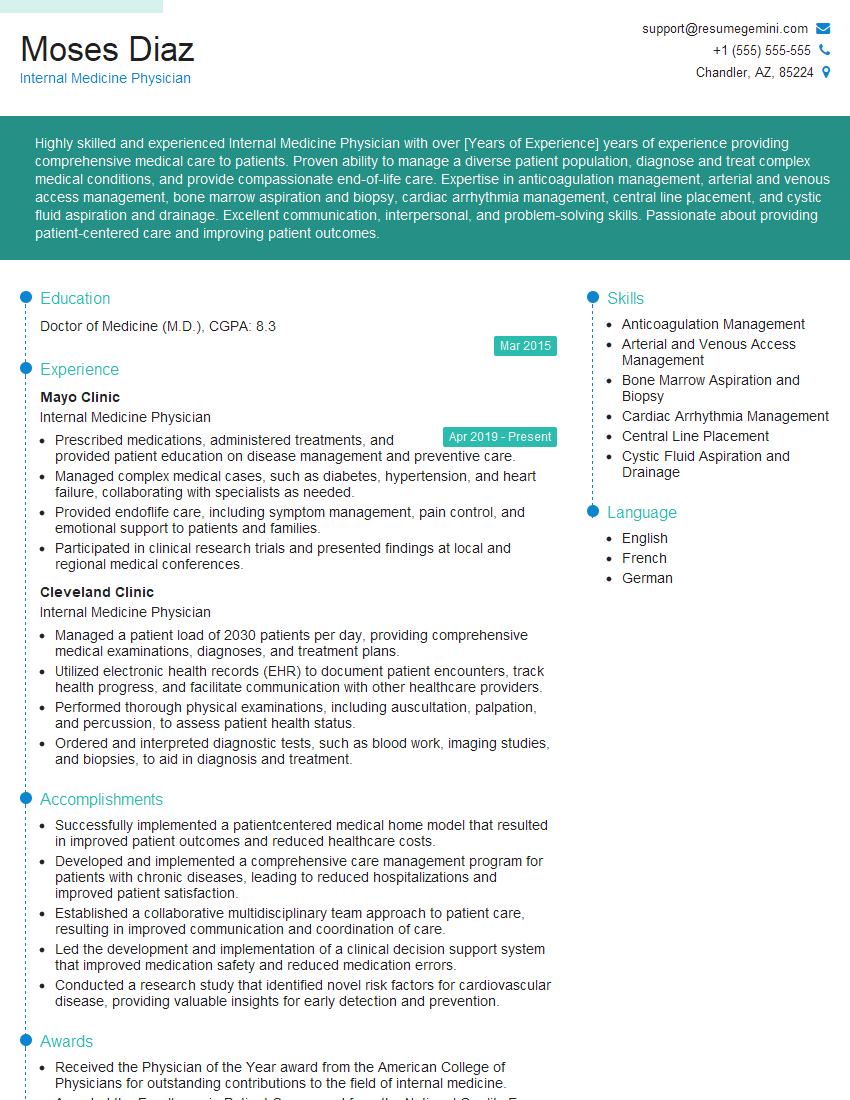
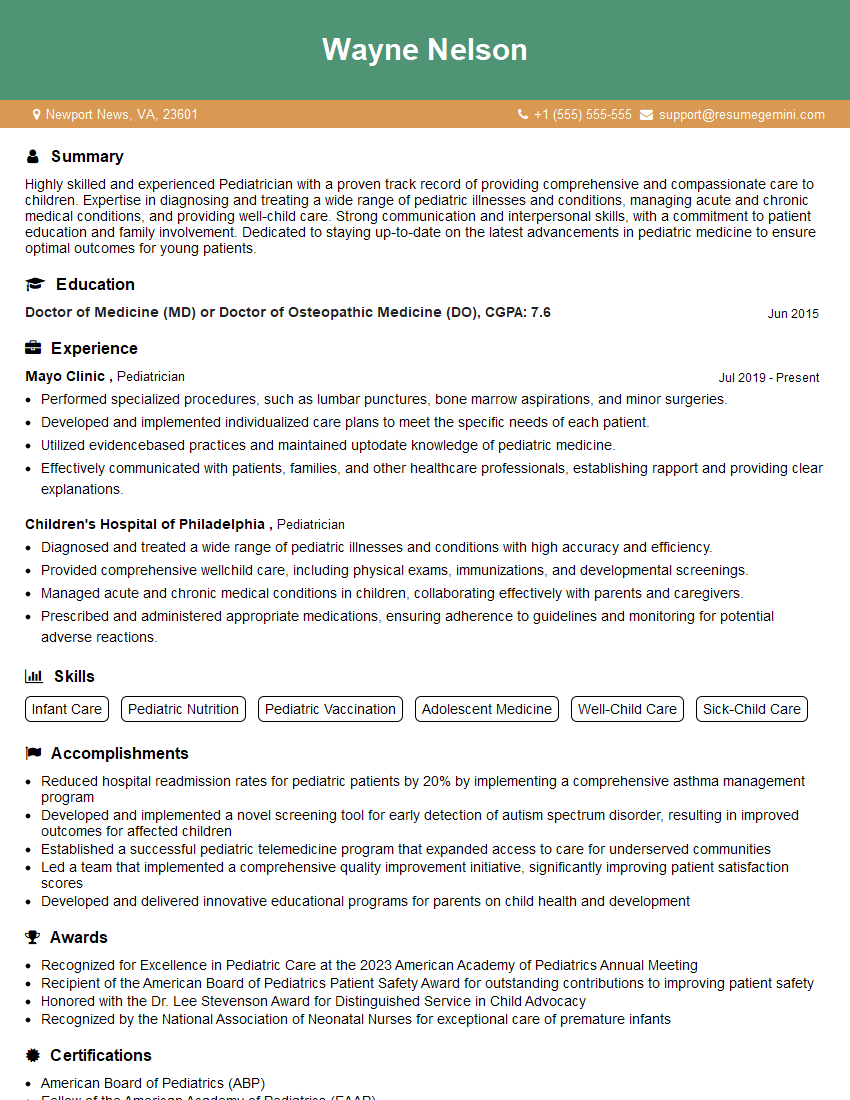
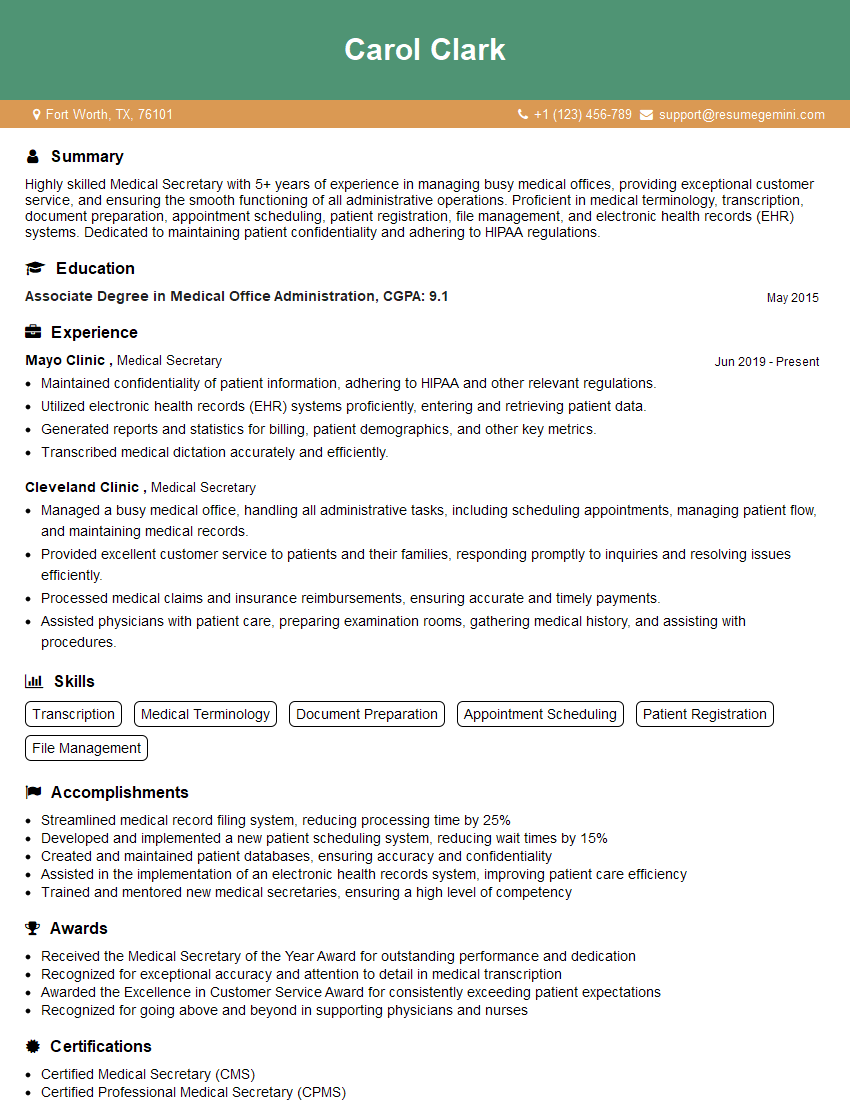
Mastering Ambulatory Medicine principles is crucial for career advancement and opens doors to diverse roles in this rapidly growing field. A strong resume is essential for showcasing your skills and experience to potential employers. Building an ATS-friendly resume significantly increases your chances of getting noticed by recruiters. We strongly recommend using ResumeGemini to craft a compelling and effective resume. ResumeGemini offers a user-friendly platform and provides examples of resumes tailored to Ambulatory Medicine to help you present yourself in the best possible light. This will help you stand out in a competitive job market.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Interesting Article, I liked the depth of knowledge you’ve shared.
Helpful, thanks for sharing.
Hi, I represent a social media marketing agency and liked your blog
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?