Preparation is the key to success in any interview. In this post, we’ll explore crucial Primary Care interview questions and equip you with strategies to craft impactful answers. Whether you’re a beginner or a pro, these tips will elevate your preparation.
Questions Asked in Primary Care Interview
Q 1. Describe your approach to diagnosing common respiratory infections.
Diagnosing common respiratory infections involves a systematic approach combining history, physical examination, and sometimes, investigations. I begin by carefully listening to the patient’s description of their symptoms – onset, duration, character of cough (productive or non-productive), sputum color, fever, shortness of breath, chest pain, and any associated symptoms like sore throat or rhinorrhea. This helps differentiate between viral and bacterial infections.
The physical examination focuses on assessing vital signs (temperature, heart rate, respiratory rate, blood pressure, oxygen saturation), auscultating the lungs for wheezes, crackles, or rhonchi, and examining the throat for redness or exudates. For example, a patient with a sudden onset of high fever, productive cough with green sputum, and localized lung findings might suggest pneumonia, while a patient with gradual onset of cough, clear rhinorrhea, and mild fever likely has a viral upper respiratory infection.
Further investigations, such as a chest X-ray or blood tests (complete blood count with differential), might be necessary depending on the clinical picture. For instance, if pneumonia is suspected, a chest X-ray is crucial to confirm the diagnosis and guide treatment. In cases of atypical pneumonia, specific serological tests might be needed.
It’s also vital to consider other differential diagnoses like asthma exacerbations, COPD exacerbations, or even heart failure, as respiratory symptoms can overlap significantly. A thorough history and physical exam, combined with judicious use of investigations, are essential for accurate diagnosis and appropriate management.
Q 2. Explain your management strategy for hypertension in a 65-year-old patient.
Managing hypertension in a 65-year-old patient requires a multi-faceted approach focusing on lifestyle modifications and medication, tailored to the individual’s needs and comorbidities. First, I assess the patient’s cardiovascular risk factors – smoking, diabetes, dyslipidemia, family history of heart disease – to stratify their risk and determine the intensity of treatment required.
Lifestyle modifications are paramount and should always be implemented first. This includes dietary changes emphasizing a DASH diet (Dietary Approaches to Stop Hypertension) low in sodium and rich in fruits, vegetables, and whole grains; regular aerobic exercise (at least 150 minutes per week); weight reduction if overweight or obese; and limiting alcohol consumption. These changes can significantly improve blood pressure control and reduce the need for medications or minimize the dosages required.
Pharmacological management usually involves initiating medication if lifestyle changes alone are insufficient to reach target blood pressure (<70/80 mmHg typically, or lower if comorbidities are present). The choice of medication depends on factors like age, comorbidities, other medications, and patient preferences. Commonly used medications include thiazide diuretics, ACE inhibitors, ARBs, beta-blockers, and calcium channel blockers. For instance, a patient with concomitant diabetes might benefit from an ACE inhibitor for its renoprotective effects. Regular monitoring of blood pressure and potential side effects is crucial for optimizing treatment and ensuring patient safety.
I emphasize shared decision-making throughout the process, involving the patient actively in setting goals, understanding treatment options, and addressing their concerns. This approach improves adherence and contributes to better overall outcomes.
Q 3. How do you counsel patients on preventative health measures like vaccinations?
Counseling patients on preventative health measures, particularly vaccinations, requires a patient-centered approach that addresses individual concerns and misconceptions. I begin by explaining the importance of the specific vaccine, outlining the benefits and risks in clear, understandable language, avoiding medical jargon. For example, when discussing the influenza vaccine, I’ll explain how it can reduce the risk of severe illness, hospitalization, and even death. I emphasize the protection it offers not only to the individual but also to vulnerable individuals in their family and community.
Addressing patient concerns is crucial. Many hesitate due to fears of side effects or misinformation. I use evidence-based information to debunk myths and address their specific worries. For instance, if a patient is concerned about side effects, I’ll explain that common reactions are usually mild and temporary. I also leverage reputable resources like the CDC website for further clarification and patient education.
The counseling session also includes assessing the patient’s vaccination history and identifying any contraindications. For certain vaccines, blood tests might be required prior to administration. I ensure shared decision-making, empowering the patient to make an informed choice based on their understanding of the benefits, risks, and alternatives. Finally, I schedule the vaccination and provide clear instructions on post-vaccination care.
Q 4. What are the key indicators of diabetes, and how do you screen for it?
Key indicators of diabetes include hyperglycemia (high blood sugar), often manifested by classic symptoms like increased thirst (polydipsia), frequent urination (polyuria), unexplained weight loss, increased hunger (polyphagia), and blurred vision. However, many individuals with type 2 diabetes initially have no noticeable symptoms.
Screening for diabetes involves assessing risk factors such as age, family history of diabetes, obesity, physical inactivity, and ethnicity. The most common screening tests are fasting plasma glucose (FPG), oral glucose tolerance test (OGTT), and hemoglobin A1c (HbA1c).
An FPG level of ≥126 mg/dL on two separate occasions confirms a diagnosis of diabetes. The OGTT measures blood glucose levels after consuming a sugary drink, and a level of ≥200 mg/dL two hours post-ingestion confirms diabetes. HbA1c measures average blood glucose levels over the past 2-3 months, and a level of ≥6.5% confirms diabetes.
The choice of screening test depends on the individual’s risk factors and clinical presentation. Individuals with significant risk factors may require screening even in the absence of symptoms. Early detection and management are critical for preventing long-term complications of diabetes, such as heart disease, kidney disease, and blindness. I always emphasize lifestyle modifications as a cornerstone of diabetes management even before initiating medication.
Q 5. Describe your experience with managing chronic pain in primary care settings.
Managing chronic pain in primary care requires a holistic approach that considers the biopsychosocial aspects of the condition. I begin by thoroughly evaluating the patient’s pain history – onset, location, character, duration, intensity (using a validated pain scale like the 0-10 numeric rating scale), and aggravating/relieving factors. A comprehensive physical examination is essential to identify any underlying medical conditions that might be contributing to the pain.
My approach combines pharmacological and non-pharmacological interventions. Pharmacological management might include over-the-counter analgesics like acetaminophen or NSAIDs for mild to moderate pain, or stronger opioids for severe pain, always considering the potential risks and benefits. I emphasize a multimodal approach; combining different types of medications may be more effective and reduce the risk of side effects.
Non-pharmacological interventions are equally important and often the cornerstone of long-term management. These include physical therapy, occupational therapy, cognitive behavioral therapy (CBT), stress management techniques, and lifestyle modifications like regular exercise and healthy diet. For example, a patient with chronic back pain might benefit from physical therapy to improve strength and flexibility, along with CBT to manage pain-related anxiety and depression.
Regular follow-up appointments are crucial to monitor pain levels, assess treatment effectiveness, and adjust the management plan as needed. Shared decision-making is vital, empowering the patient to actively participate in their care and take ownership of their pain management.
Q 6. How do you approach patients with mental health concerns in a primary care setting?
Approaching patients with mental health concerns in primary care requires sensitivity, empathy, and a collaborative approach. I start by creating a safe and non-judgmental environment where patients feel comfortable sharing their experiences. I use open-ended questions to explore their concerns and understand the impact of their mental health on their daily life. This involves assessing symptoms using standardized tools like the PHQ-9 for depression and the GAD-7 for anxiety.
My approach involves a combination of strategies. For mild to moderate conditions, I might offer brief interventions, such as psychoeducation, relaxation techniques, and lifestyle modifications (like regular exercise and healthy sleep hygiene). I also actively collaborate with mental health specialists, providing referrals when necessary. This includes referring to psychiatrists for medication management or to psychologists or therapists for psychotherapy.
For more severe cases, I work closely with the mental health specialists to ensure continuity of care. I also pay close attention to the patient’s overall well-being, screening for other potential problems such as substance abuse or domestic violence, which might be intertwined with their mental health condition. Collaboration with community resources and support groups is essential to provide a comprehensive and supportive care plan.
I am mindful of the stigma associated with mental health and strive to reduce that barrier by fostering a supportive and understanding relationship with my patients.
Q 7. What is your approach to managing a patient with an acute exacerbation of COPD?
Managing an acute exacerbation of COPD requires prompt assessment and intervention to stabilize the patient’s respiratory status and prevent further deterioration. I begin by carefully assessing the patient’s symptoms, including shortness of breath (dyspnea), increased cough, sputum production (change in color, amount, or consistency), and wheezing. I evaluate vital signs (respiratory rate, heart rate, oxygen saturation) and auscultate the lungs to assess the severity of the exacerbation.
Immediate management usually involves supplemental oxygen therapy to maintain oxygen saturation above 90%, bronchodilators (short-acting beta-agonists and anticholinergics) to relieve bronchospasm and improve airflow, and systemic corticosteroids to reduce inflammation. In severe cases, hospitalization might be necessary for closer monitoring and more aggressive respiratory support, including non-invasive or invasive ventilation.
Blood gas analysis and chest X-ray may be crucial to assess the severity of the exacerbation and rule out other complications, such as pneumonia. Antibiotics are usually prescribed only if there are signs of infection, such as purulent sputum, increased fever, or worsening leukocytosis.
Patient education and long-term management are equally crucial. This involves reviewing medication regimens, inhaler technique, and lifestyle modifications, such as smoking cessation and pulmonary rehabilitation. Regular follow-up appointments are essential to monitor the patient’s progress and adjust the management plan as needed, aiming to prevent future exacerbations. The overall goal is to improve the patient’s quality of life and reduce hospital readmissions.
Q 8. How do you assess for and manage risk factors for cardiovascular disease?
Assessing and managing cardiovascular disease (CVD) risk factors involves a multifaceted approach. It begins with a thorough patient history, focusing on family history of CVD, lifestyle factors (diet, exercise, smoking), and existing conditions like diabetes and hypertension. A physical exam includes checking blood pressure, weight, and listening to heart and lung sounds. Laboratory tests are crucial; we order lipid panels to measure cholesterol levels, fasting blood glucose to screen for diabetes, and potentially other tests based on individual risk profiles.
Risk stratification is key. We use tools like the Framingham Risk Score to estimate the 10-year risk of a major CVD event. This helps determine the intensity of interventions. For example, a patient with a high risk might require aggressive lifestyle modifications, medication (statins to lower cholesterol, antihypertensives for blood pressure control), and close monitoring. A patient with a low risk may need focused lifestyle counseling and periodic check-ups.
Management involves collaborative goal setting. We work with the patient to create a personalized plan that’s realistic and achievable. This might involve referring them to a dietitian, encouraging regular exercise, smoking cessation programs, or stress management techniques. Regular follow-up appointments are crucial to monitor progress, adjust medication, and address any new concerns.
Example: A 55-year-old male smoker with a family history of heart disease and elevated cholesterol would be considered high-risk. We’d initiate statin therapy, prescribe blood pressure medication if needed, strongly advise him to quit smoking, and refer him to a cardiac rehabilitation program. We would also schedule regular follow-up visits to monitor his progress and adjust treatment as needed.
Q 9. Explain your method of patient education for managing asthma.
Patient education for asthma management is critical for achieving good control and preventing exacerbations. My approach involves a combination of verbal explanations, written materials, and demonstration. I use the teach-back method to ensure understanding. I explain asthma in simple terms, comparing the airways to a garden hose that’s narrowed by inflammation and mucus.
I cover the following key areas:
- Asthma triggers: Identifying and avoiding allergens (dust mites, pet dander, pollen), irritants (smoke, pollution), and triggers specific to the patient (exercise, stress, infections).
- Medication use: Clearly explaining how to use inhalers (spacer devices are useful for better delivery), peak flow meters (to monitor lung function), and rescue medications (short-acting bronchodilators) for acute symptoms. I demonstrate correct inhaler technique.
- Asthma action plan: A personalized plan that outlines steps to take based on symptoms and peak flow readings, helping patients manage their own asthma effectively and know when to seek medical attention. This often involves color-coded zones (green, yellow, red) to indicate severity.
- Lifestyle modifications: Encouraging regular exercise (aerobic activities are generally beneficial), a healthy diet, and strategies for stress reduction.
I provide written materials like brochures and action plans, tailored to the patient’s reading level and cultural background. Regular follow-up appointments allow for reinforcement, adjustment of the treatment plan, and addressing any questions or concerns.
Example: I would demonstrate the proper use of a metered-dose inhaler (MDI) with a spacer, ensuring the patient understands how to coordinate inhaling and depressing the canister. I would also provide them with a written action plan, explaining what to do in each zone (green: maintain treatment, yellow: increase medication, red: seek immediate medical care).
Q 10. Describe a situation where you had to deal with a difficult patient or family member.
I once had a patient who was extremely resistant to lifestyle changes despite a clear diagnosis of type 2 diabetes and significant risk factors for CVD. He was angry and frustrated by the diagnosis, and refused to follow my recommendations for diet and exercise. His family, while supportive, also felt overwhelmed by his lack of cooperation.
My approach was to actively listen to his concerns and validate his feelings without minimizing the seriousness of his condition. I addressed his anger with empathy, acknowledging the challenges of changing long-standing habits. We collaboratively developed a plan, focusing on small, achievable steps rather than drastic changes. Instead of demanding complete dietary overhaul, we targeted one or two unhealthy habits to modify at a time, like reducing sugary drinks or increasing vegetable intake. We set realistic expectations and celebrated small victories.
I involved his family in the process, providing them with educational resources and strategies for supportive communication. Over time, the patient’s attitude shifted; he became more engaged in his treatment, recognizing the gradual positive impact of the changes he made. This situation emphasized the importance of patient-centered care, empathy, and collaborative goal-setting, particularly when dealing with challenging patients.
Q 11. How do you ensure patient confidentiality and comply with HIPAA regulations?
Patient confidentiality and HIPAA compliance are paramount in my practice. I strictly adhere to HIPAA regulations by only accessing and disclosing protected health information (PHI) when necessary for providing care or when legally required. This includes securing all electronic and paper records, using strong passwords, and implementing appropriate access controls within the electronic health record (EHR) system.
I follow these key practices:
- Limited access: Only authorized personnel have access to patient records. I make sure to log out of the EHR system when leaving my workstation.
- Secure communication: I use secure messaging systems when communicating with patients or other healthcare professionals about confidential information. I avoid discussing PHI in public areas.
- Patient education: I inform patients about their rights regarding their health information, including their right to access, amend, and restrict the use of their data. I obtain their consent before sharing information with anyone.
- Data breaches: I understand the procedures for reporting potential data breaches and handling such incidents effectively.
Example: I would never discuss a patient’s diagnosis or treatment plan with anyone outside the healthcare team without their explicit consent, unless legally obligated to do so, such as in a case of mandatory reporting of child abuse or public health concerns.
Q 12. What is your preferred method for ordering and interpreting laboratory tests?
My approach to ordering and interpreting laboratory tests is evidence-based and patient-specific. I don’t order tests routinely; instead, I select tests based on the patient’s symptoms, physical exam findings, and relevant risk factors. I choose tests that will directly influence the diagnosis and management plan.
I utilize our electronic health record system (EHR) to order tests, which ensures accurate entry of information and facilitates communication with the laboratory. Once results are available, I carefully review them, correlating them with the clinical picture. I consider factors such as potential interference from medication, the reliability of the test, and the patient’s overall health status when interpreting results.
Example: For a patient presenting with fatigue and anemia symptoms, I would order a complete blood count (CBC) and potentially iron studies to evaluate for iron deficiency anemia. If the CBC reveals leukocytosis (elevated white blood cells), further investigations like a differential count might be necessary. I would interpret the results in light of the patient’s history and physical findings, potentially adjusting treatment based on my findings.
Q 13. How do you utilize electronic health records (EHRs) in your daily practice?
Electronic health records (EHRs) are indispensable tools in my daily practice. I use them for a wide range of functions, enhancing both efficiency and patient care.
Clinical documentation: The EHR allows me to efficiently record patient encounters, including the history of present illness, physical examination findings, diagnoses, treatment plans, and progress notes. This ensures comprehensive and easily accessible records.
Order entry: I use the EHR to order laboratory tests, imaging studies, and medications, minimizing errors and ensuring accurate and timely completion of orders.
Medication management: The EHR helps me monitor medication lists, identify potential drug interactions, and ensure appropriate dosing regimens. It also facilitates medication reconciliation.
Patient communication: Secure messaging within the EHR facilitates communication with patients, providing them with quick access to important information such as test results, appointment reminders, and medication refills.
Population health management: I use the EHR’s reporting and analytics capabilities to identify patients due for preventative screenings, manage chronic disease, and identify trends in patient populations. This supports proactive care and improvement in healthcare outcomes.
Example: Using EHRs, I can quickly generate a patient’s complete medication list and identify a potential drug interaction before it causes harm. This is a crucial feature of safety and patient-centered care.
Q 14. Describe your approach to preventive care for women’s health.
My approach to preventive care for women’s health is comprehensive and age-appropriate, encompassing risk factor assessment, screening tests, and health promotion strategies.
Age-specific screening: I tailor recommendations based on the patient’s age and risk factors. For example, younger women need education on birth control, sexually transmitted infections (STIs), and healthy lifestyle habits. Older women require screening for osteoporosis, cardiovascular disease, and other age-related conditions.
Preventive services: I provide guidance on:
- Pap smears: Regular cervical cancer screening, guided by updated guidelines.
- Mammograms: Breast cancer screening, adhering to current recommendations based on age and risk.
- STI testing: Based on individual risk factors and sexual history.
- Bone density scans: For women at increased risk of osteoporosis.
- Cardiovascular risk assessment: Including blood pressure, cholesterol, and diabetes screenings.
- Mental health screening: Addressing anxiety, depression, and stress.
Lifestyle counseling: I encourage a healthy lifestyle, including regular exercise, a balanced diet, and smoking cessation. I discuss healthy weight management, safe sun exposure, and stress-reduction strategies.
Family planning counseling: I offer guidance on contraception, fertility, and pregnancy planning.
Example: A 45-year-old woman would receive counseling on mammogram scheduling, cardiovascular disease risk assessment, and screening for osteoporosis. A younger woman might require counseling on birth control options, safe sex practices, and vaccinations for HPV.
Q 15. How do you address concerns about medication side effects with patients?
Addressing medication side effects starts with proactive communication and patient education. Before prescribing, I thoroughly discuss potential side effects, their likelihood, and their severity, using clear, non-medical jargon. I provide patients with written information and encourage them to ask questions. If side effects occur, I listen empathetically, validating their experience. We then collaboratively explore options: reducing dosage, switching medications, managing side effects with additional medications or lifestyle changes, or discontinuing the medication altogether, depending on the severity and the patient’s priorities. For example, if a patient experiences nausea from a new blood pressure medication, we might try a different medication, adjust the timing of the dose (e.g., taking it with food), or add an anti-nausea medication. Ultimately, the goal is to find a medication regimen that is both effective and tolerable for the patient.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you handle a patient who is non-compliant with treatment recommendations?
Non-compliance is a complex issue requiring a patient-centered approach. I begin by understanding the reasons for non-compliance – are there barriers to accessing medication, financial constraints, misunderstanding of the treatment plan, side effects, or other concerns? I use open-ended questions to explore their perspectives and create a therapeutic alliance. We then collaboratively develop a plan to address those barriers. This might involve simplifying the medication regimen, providing financial assistance, adjusting the treatment plan based on patient preferences, or connecting them with support services like transportation or home health care. Regular follow-up appointments and using motivational interviewing techniques are crucial to reinforce adherence and address any emerging challenges. For example, if a patient is struggling to take their medication due to forgetfulness, we may explore the use of a pill organizer or set reminders on their phone.
Q 17. What is your approach to managing patients with substance use disorders?
Managing substance use disorders (SUDs) requires a holistic approach combining medical, psychological, and social support. I conduct a thorough assessment of the patient’s substance use history, mental health status, and social circumstances. I offer evidence-based treatments like medication-assisted treatment (MAT), such as buprenorphine or naltrexone, in conjunction with counseling and support groups. I connect patients with appropriate resources like addiction specialists, therapists, and support networks. Regular follow-up is vital to monitor progress, address relapses (which are a normal part of recovery), and adjust the treatment plan accordingly. Building rapport and fostering trust are essential to promoting engagement in treatment and long-term recovery. The approach is highly individualized, recognizing the unique challenges faced by each patient.
Q 18. How do you differentiate between bacterial and viral infections?
Differentiating between bacterial and viral infections isn’t always straightforward, often requiring clinical judgment and sometimes laboratory testing. However, some clues can help. Bacterial infections often present with localized symptoms like pus, swelling, and high fever, while viral infections might involve more generalized symptoms such as fatigue, muscle aches, and a low-grade fever. The timing of symptoms can also be helpful: bacterial infections might develop more quickly. However, it’s critical to note that some conditions can be caused by both (e.g., pneumonia). Ultimately, a thorough history, physical examination, and possibly laboratory tests like blood cultures or rapid strep tests are necessary to determine the cause and guide appropriate treatment. This is crucial because treating a bacterial infection with antibiotics is important, while antibiotics are ineffective and sometimes harmful against viral infections.
Q 19. Describe your understanding of common childhood illnesses and their management.
Common childhood illnesses require prompt recognition and appropriate management. These include respiratory infections like croup, bronchiolitis, and pneumonia; gastrointestinal illnesses like rotavirus and gastroenteritis; and skin infections like impetigo. My approach involves thorough history-taking, focusing on symptoms, duration, and exposure to other sick children. A physical exam helps assess the severity of illness. Management includes supportive care – fluids, rest, and fever management – and, in some cases, specific treatments like antibiotics for bacterial infections or antiviral medications for specific viral infections. I emphasize preventive measures such as vaccinations and hand hygiene. For example, a child with croup may need humidified air or even corticosteroids, while a child with gastroenteritis requires careful monitoring for dehydration. Parental education is crucial for managing symptoms and recognizing when medical attention is needed.
Q 20. Explain your approach to managing geriatric patients with multiple comorbidities.
Managing geriatric patients with multiple comorbidities requires a comprehensive, patient-centered approach. I start by obtaining a detailed medical history, including all medications, allergies, and past illnesses. I conduct a thorough physical exam paying close attention to age-related changes. I prioritize medication reconciliation to avoid polypharmacy and drug interactions. Functional assessment is vital, focusing on activities of daily living (ADLs) and instrumental activities of daily living (IADLs) to tailor interventions to maintain independence. I involve the patient and family in shared decision-making, taking into account their preferences and goals of care. Regular monitoring and close collaboration with specialists are crucial for managing complex medical needs. A geriatric patient with hypertension, diabetes, and osteoarthritis may require a coordinated plan involving medication adjustments, physical therapy, and lifestyle modifications to optimize their overall health and quality of life.
Q 21. How do you handle emergency situations in a primary care setting?
Handling emergencies in a primary care setting requires a systematic approach. I follow the ABCDEs of resuscitation: Airway, Breathing, Circulation, Disability, and Exposure. I immediately assess the patient’s vital signs and initiate appropriate life support measures, including CPR and defibrillation if necessary. I contact emergency medical services (EMS) promptly and provide them with essential information. I stabilize the patient until EMS arrives and ensure a smooth handoff. I document the event thoroughly, including the patient’s condition, interventions performed, and EMS communication. Regular training and drills are essential to maintain proficiency in emergency procedures. The priority is always to ensure the patient’s safety and survival while coordinating with higher levels of care.
Q 22. Describe your experience with ordering and interpreting imaging studies.
Ordering and interpreting imaging studies are crucial aspects of providing comprehensive primary care. My experience encompasses a wide range of imaging modalities, including X-rays, CT scans, ultrasounds, and MRIs. I understand the indications for each type of imaging and carefully select the appropriate test based on the patient’s clinical presentation and suspected diagnosis. For example, if a patient presents with acute abdominal pain, I might order an ultrasound to assess for appendicitis or gallstones, whereas chest X-rays are often the first-line imaging for suspected pneumonia.
Interpreting the results requires a thorough understanding of anatomy, physiology, and pathology. I don’t attempt to interpret complex imaging myself. Instead, I rely on radiologists’ reports, but I have the necessary skills to understand the key findings and correlate them with the patient’s clinical picture. If the radiology report is unclear or raises concerns, I always clarify with the radiologist directly, ensuring we’re on the same page for effective patient management. I also frequently use the PACS (Picture Archiving and Communication System) to review images myself to have a clearer visual understanding of the patient’s condition. This collaborative approach ensures accurate diagnosis and appropriate treatment.
Q 23. How do you collaborate with specialists to ensure comprehensive patient care?
Collaboration with specialists is paramount in delivering comprehensive patient care. I believe in a team-based approach, involving specialists when necessary and maintaining open communication throughout the process. This often begins with a well-structured referral, clearly outlining the patient’s history, presenting complaint, examination findings, and any preliminary investigations. For example, if a patient presents with symptoms suggestive of diabetes, I might refer them to an endocrinologist for further assessment and management of the condition.
Following the specialist consultation, I actively follow up with both the specialist and the patient to ensure seamless continuity of care. We often discuss treatment plans collaboratively, ensuring the plan aligns with the patient’s overall health goals and preferences. Regular communication keeps the patient informed and empowered throughout their healthcare journey. I use secure electronic communication methods like patient portals and dedicated healthcare platforms for efficient and confidential information exchange.
Q 24. What resources do you utilize to stay updated on the latest guidelines and best practices in primary care?
Staying updated on the latest guidelines and best practices is crucial for providing high-quality primary care. I utilize a variety of resources to achieve this. The most important sources are peer-reviewed medical journals like the Journal of the American Medical Association (JAMA), the New England Journal of Medicine (NEJM), and the BMJ. I regularly review guidelines published by organizations such as the US Preventive Services Task Force (USPSTF) and the Centers for Disease Control and Prevention (CDC).
Furthermore, I actively participate in continuing medical education (CME) activities such as workshops, conferences, and online courses. This allows me to stay abreast of advancements in medical knowledge and learn new techniques and approaches to patient care. Professional organizations like the American Academy of Family Physicians (AAFP) provide valuable resources, including online learning modules and newsletters. I also find participating in journal clubs with colleagues incredibly beneficial for a shared understanding of current research and its practical application in our practice.
Q 25. How do you approach ethical dilemmas in your practice?
Ethical dilemmas are an inevitable part of medical practice. My approach involves a systematic framework to navigate these complex situations. First, I carefully identify the ethical issue at hand, considering all relevant factors involved. For example, a patient might refuse a life-saving treatment due to religious beliefs, presenting a conflict between beneficence (doing good) and respecting patient autonomy.
Next, I consult relevant ethical guidelines and resources, considering the principles of medical ethics: beneficence, non-maleficence, autonomy, and justice. I might seek counsel from colleagues, ethics committees, or mentors experienced in handling similar dilemmas. A structured approach involving careful consideration of the patient’s values, preferences, and the medical facts will help in reaching a solution that respects the patient’s autonomy while ensuring they receive the best possible care. Documentation of the decision-making process and the rationale behind it is crucial for transparency and accountability.
Q 26. Explain your understanding of health disparities and how you address them in your practice.
Health disparities, the unequal distribution of healthcare resources and outcomes based on factors like race, ethnicity, socioeconomic status, and geographic location, are a significant concern. I recognize their impact on patient health and strive to address them in my practice. I begin by actively acknowledging the social determinants of health that might influence a patient’s access to care or health outcomes. These factors include poverty, lack of transportation, limited health literacy, and inadequate access to healthy food.
To combat these disparities, I tailor my approach to each patient’s unique circumstances. This includes providing culturally sensitive care, using plain language to ensure clear understanding, and connecting patients with community resources such as food banks, transportation assistance programs, and language services. I advocate for policy changes that address social determinants of health at a broader level, participating in community initiatives aimed at improving health equity. This might include participating in local health fairs or community outreach programs that improve awareness and access to care.
Q 27. Describe your experience with patient advocacy and health promotion.
Patient advocacy and health promotion are integral to my role as a primary care physician. Patient advocacy involves acting on behalf of patients to ensure they receive the best possible care and have their needs met. This can range from navigating complex healthcare systems to advocating for access to specialized services or financial assistance. For example, I’ve helped patients access affordable medications, navigate insurance coverage issues, and obtain necessary home healthcare services.
Health promotion involves educating and empowering patients to take control of their health. I provide individualized counseling on lifestyle modifications, including diet, exercise, and stress management. I actively screen for common preventable diseases and offer vaccinations. I encourage patients to participate in shared decision-making by involving them in choosing their treatment plan, fostering a collaborative approach. Regular health check-ups and proactive health discussions with patients are key elements of my approach to health promotion and patient advocacy.
Q 28. How do you use data and metrics to improve the quality of your primary care services?
Data and metrics play a vital role in improving the quality of primary care services. We use electronic health records (EHRs) to track key performance indicators (KPIs) such as blood pressure control rates, HbA1c levels in diabetic patients, and cancer screening rates. By regularly analyzing these metrics, we can identify areas of strength and weakness in our practice. For example, if our diabetes control rates are below target, we can review our protocols, implement quality improvement initiatives, and provide additional patient education to improve outcomes.
We also use patient satisfaction surveys to gauge patient experiences and identify areas for improvement in communication, accessibility, and overall care. Data analytics helps us to assess our performance on various quality measures set by regulatory bodies and accreditation agencies. The use of data allows us to make informed decisions about resource allocation, refine our processes, and ultimately provide more efficient and effective primary care services to our patients. This iterative process of data analysis, intervention, and reassessment is key to continuous quality improvement.
Key Topics to Learn for Primary Care Interview
- Patient-Centered Care: Understanding the principles of patient-centered care, including shared decision-making and incorporating patient preferences into treatment plans. Practical application: Describe a situation where you prioritized patient autonomy in a clinical setting.
- Chronic Disease Management: Mastering the management of common chronic conditions like diabetes, hypertension, and hyperlipidemia, including preventative measures and treatment strategies. Practical application: Outline your approach to managing a patient with poorly controlled type 2 diabetes.
- Preventive Medicine: Familiarity with screening guidelines, vaccination schedules, and health promotion strategies for various age groups and risk factors. Practical application: Explain your rationale for recommending specific screening tests for a 50-year-old male patient.
- Common Presenting Complaints: Thorough understanding of the diagnosis and management of frequently encountered conditions in primary care, including respiratory infections, musculoskeletal pain, and gastrointestinal issues. Practical application: Describe your approach to diagnosing and managing a patient presenting with acute bronchitis.
- Mental Health Integration: Knowledge of common mental health disorders, screening tools, and collaborative care models for integrating mental health into primary care. Practical application: Discuss your approach to identifying and managing depression in a primary care setting.
- Health Maintenance and Wellness: Understanding the importance of health promotion, disease prevention, and patient education in achieving optimal health outcomes. Practical application: Outline a wellness plan for a patient seeking to improve their cardiovascular health.
- Ethical and Legal Considerations: Familiarity with relevant ethical guidelines, legal frameworks, and professional responsibilities in primary care. Practical application: Describe a challenging ethical dilemma you faced and how you resolved it.
Next Steps
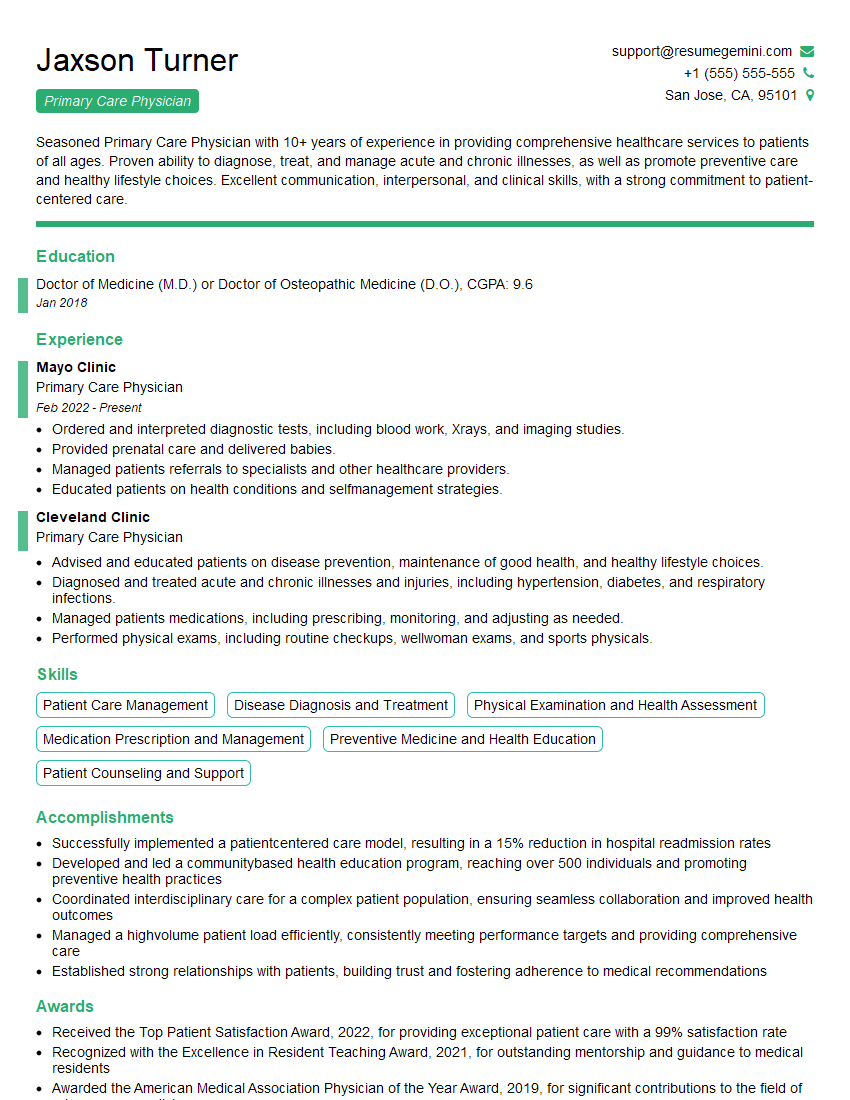
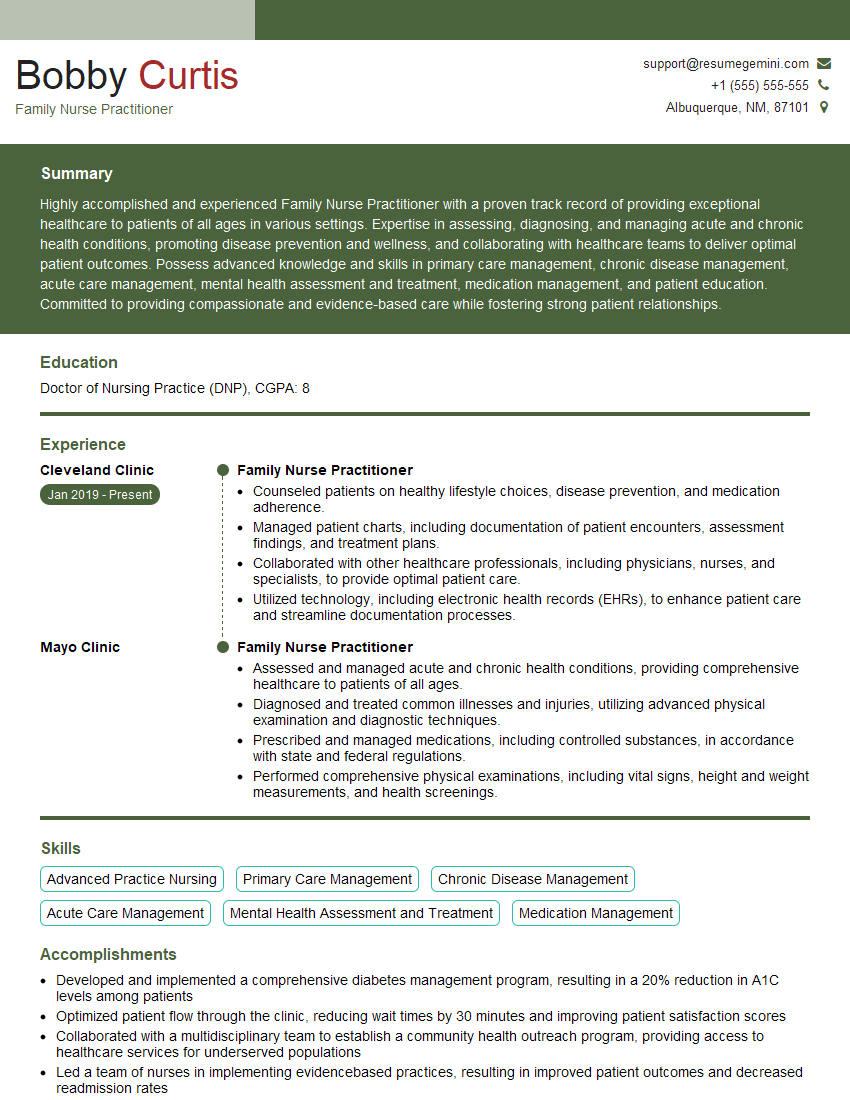
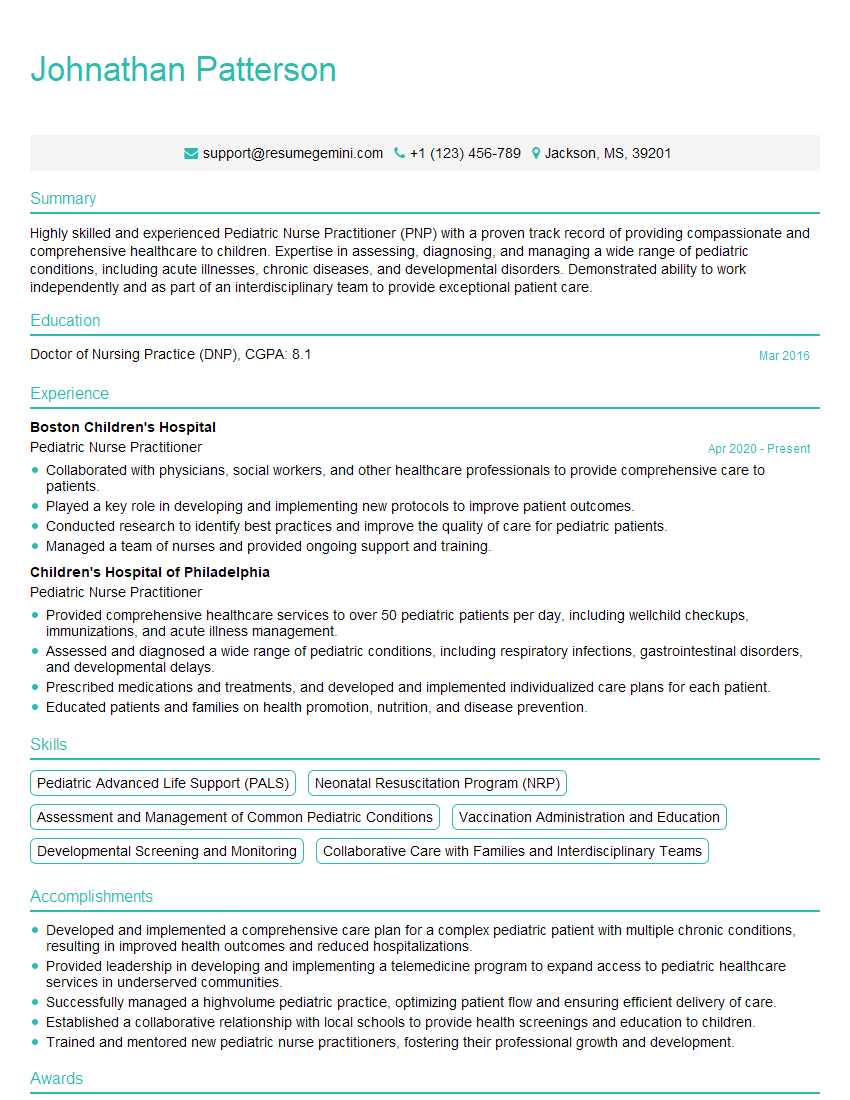
Mastering these key areas of Primary Care will significantly enhance your career prospects and allow you to make a real difference in patients’ lives. A strong resume is crucial for showcasing your skills and experience to potential employers. Creating an ATS-friendly resume is essential for maximizing your chances of getting your application noticed. We strongly recommend using ResumeGemini, a trusted resource for building professional resumes, to help you present your qualifications effectively. ResumeGemini provides examples of resumes tailored to Primary Care to guide you through the process.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Amazing blog
hello,
Our consultant firm based in the USA and our client are interested in your products.
Could you provide your company brochure and respond from your official email id (if different from the current in use), so i can send you the client’s requirement.
Payment before production.
I await your answer.
Regards,
MrSmith
hello,
Our consultant firm based in the USA and our client are interested in your products.
Could you provide your company brochure and respond from your official email id (if different from the current in use), so i can send you the client’s requirement.
Payment before production.
I await your answer.
Regards,
MrSmith
These apartments are so amazing, posting them online would break the algorithm.
https://bit.ly/Lovely2BedsApartmentHudsonYards
Reach out at [email protected] and let’s get started!
Take a look at this stunning 2-bedroom apartment perfectly situated NYC’s coveted Hudson Yards!
https://bit.ly/Lovely2BedsApartmentHudsonYards
Live Rent Free!
https://bit.ly/LiveRentFREE
Interesting Article, I liked the depth of knowledge you’ve shared.
Helpful, thanks for sharing.
Hi, I represent a social media marketing agency and liked your blog
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?