Are you ready to stand out in your next interview? Understanding and preparing for Manage Patient Flow and Triage interview questions is a game-changer. In this blog, we’ve compiled key questions and expert advice to help you showcase your skills with confidence and precision. Let’s get started on your journey to acing the interview.
Questions Asked in Manage Patient Flow and Triage Interview
Q 1. Describe your experience with optimizing patient flow in a high-volume environment.
Optimizing patient flow in a high-volume environment requires a multifaceted approach focusing on efficiency and minimizing bottlenecks. My experience involves implementing and refining processes across various points in the patient journey. This includes streamlining registration, optimizing appointment scheduling (considering appointment types and provider availability), improving room utilization, and coordinating with ancillary departments like radiology and lab services.
For example, in a previous role at a large urban hospital, we implemented a new appointment scheduling system that utilized predictive analytics to forecast daily patient volumes. This allowed us to proactively adjust staffing levels and allocate resources more effectively, resulting in a 15% reduction in patient wait times. We also implemented a color-coded system for prioritizing patients based on their acuity level, ensuring that the most critical cases were seen first. This was coupled with a real-time dashboard showing the flow of patients through the department, enabling us to quickly identify and address potential issues.
Q 2. How do you prioritize patients based on urgency and acuity?
Prioritizing patients hinges on a combination of urgency and acuity. Urgency refers to the time-sensitivity of the situation (e.g., a patient experiencing chest pain needs immediate attention), while acuity describes the severity of the patient’s condition (e.g., a patient with a minor laceration has lower acuity than one with a severe head injury). We use a structured system, often involving a standardized triage system, to assess both factors. Many healthcare facilities employ a color-coded system (red, yellow, green) or a numerical scale (1-5) to denote the level of urgency and acuity.
This is often coupled with clinical decision support tools that help triage nurses to quickly assess the patient’s condition and assign the appropriate priority. For instance, a patient presenting with shortness of breath and a history of heart failure would be prioritized higher than a patient with a mild headache. The system must be regularly evaluated and adjusted to ensure its effectiveness and adherence to best practices.
Q 3. Explain your process for managing patient wait times.
Managing patient wait times is crucial for patient satisfaction and efficient resource allocation. My process involves several key strategies. Firstly, accurate appointment scheduling is paramount. This minimizes unnecessary waiting by aligning appointments with provider availability and the complexity of the visit. Secondly, real-time monitoring of patient flow allows for proactive intervention. If delays are anticipated, we communicate with patients and staff to manage expectations. Thirdly, continuous improvement processes are employed to analyze wait time data, identify bottlenecks, and implement targeted solutions.
For instance, we might identify that a particular procedure is consistently causing delays. This might prompt investigation into the process, potentially leading to workflow changes, equipment upgrades, or additional staff training. Regular review of key performance indicators (KPIs) like average wait times and patient throughput helps us track progress and refine our strategies.
Q 4. What methods do you use to effectively communicate with patients and staff regarding delays?
Effective communication is key to managing patient and staff expectations during delays. We utilize multiple channels, tailoring the approach to the audience. For patients, we use clear, concise language, explaining the reasons for any delays and providing estimated wait times. Digital signage in waiting areas can provide real-time updates, while staff members can personally address patient concerns.
For staff, we employ internal communication systems such as instant messaging or email to relay critical information about patient flow and potential issues. Regularly scheduled huddles or meetings enable collective problem-solving and coordination. Transparency is vital – keeping both patients and staff informed prevents frustration and maintains a positive working environment.
Q 5. Describe a time you had to handle a difficult patient situation related to wait times.
I recall a situation where a patient became extremely agitated due to a significant delay in seeing a specialist. He had been waiting for over two hours and was visibly distressed. I approached him calmly, acknowledged his frustration, and explained the reason for the delay – an unexpected emergency case requiring immediate attention. I apologized for the inconvenience, offered him water and a comfortable seating area, and provided regular updates on his anticipated wait time. I also personally contacted the specialist to expedite his case.
While I couldn’t eliminate the wait entirely, my focus on empathy, transparency, and proactive communication de-escalated the situation. He ultimately understood the circumstances and appreciated my efforts to address his concerns. This highlights the importance of combining effective communication skills with active problem-solving when dealing with challenging patient situations.
Q 6. How do you utilize technology to improve patient flow and triage?
Technology plays a significant role in improving patient flow and triage. Electronic health records (EHRs) streamline patient registration and information access, reducing manual processes. Patient portal access allows patients to manage their appointments and check-in remotely. Real-time dashboards provide a bird’s-eye view of patient flow, enabling proactive management of bottlenecks. Telehealth capabilities can be used for remote triage, freeing up in-person resources.
Furthermore, predictive analytics can be used to forecast patient volume and optimize staffing levels. For example, we might use data from past patient volumes to predict peak times and adjust our staffing accordingly. This allows us to allocate resources efficiently and mitigate potential delays.
Q 7. What are your strategies for managing patient flow during peak hours or emergencies?
Managing patient flow during peak hours or emergencies necessitates a flexible and adaptable approach. Pre-planned surge capacity strategies are crucial – this might include activating additional staff, re-allocating resources, and establishing clear communication protocols. Prioritization protocols should be strictly adhered to, ensuring that the most critical cases are addressed first.
During emergencies, a coordinated response involving all relevant staff is essential. Clear communication channels help maintain order and minimize confusion. Post-event reviews analyze the response, identifying areas for improvement to enhance preparedness for future events. Utilizing real-time data analysis, we can adjust resource allocation dynamically and improve the overall management of high-volume situations or unexpected surges in patient needs.
Q 8. How do you identify and address bottlenecks in the patient flow process?
Identifying bottlenecks in patient flow requires a systematic approach. Think of it like a highway system – if one lane is blocked, traffic backs up. We use a combination of methods to pinpoint these choke points. First, we analyze wait times at various stages: registration, triage, examination rooms, and discharge. Long wait times indicate a potential bottleneck. We also review patient flow charts and process maps to visually identify areas of congestion. Finally, we conduct direct observation and staff interviews to understand the root causes behind delays. For example, if we find consistently long wait times in the registration area, we might discover a shortage of staff, inefficient check-in procedures, or inadequate technology. Addressing these bottlenecks might involve hiring additional staff, streamlining processes (e.g., implementing online pre-registration), or investing in updated technology. If the bottleneck is in the examination room, we might look at improving room allocation or appointment scheduling to reduce overlap.
Q 9. What metrics do you track to measure the effectiveness of patient flow and triage?
Measuring the effectiveness of patient flow and triage relies on several key metrics. These metrics provide a quantifiable way to assess performance and identify areas for improvement. Key metrics include:
- Average wait time: This measures the time patients spend waiting at each stage of the process. A shorter wait time indicates better efficiency.
- Patient throughput: This metric reflects the number of patients processed within a specific timeframe (e.g., patients seen per hour). Higher throughput demonstrates greater efficiency.
- Patient satisfaction scores: These surveys assess patient experiences, helping to understand whether the flow process is patient-friendly. Feedback informs adjustments to improve the experience.
- Door-to-doctor time: Specifically tracks the time from patient arrival to seeing a physician. This is crucial for emergency situations.
- Length of stay (LOS): Measures the time a patient spends in the facility. Reducing LOS improves efficiency and frees up resources.
- Emergency Severity Index (ESI) adherence: In emergency departments, this measures how well triage assignments align with the actual severity of patients’ conditions.
By tracking these metrics and analyzing trends, we can make data-driven decisions to optimize patient flow and triage processes.
Q 10. How do you collaborate with other healthcare professionals to ensure efficient patient flow?
Effective collaboration is the cornerstone of efficient patient flow. It’s not a solo act; it’s teamwork. I regularly communicate with physicians, nurses, registration staff, technicians, and other healthcare professionals. We use daily huddles or weekly meetings to discuss flow challenges, patient volume, resource availability, and upcoming procedures. We utilize a collaborative approach to problem-solving, focusing on clear communication and shared goals. For example, if the radiology department is experiencing delays, we collaborate to prioritize urgent cases and explore alternative imaging solutions. Open communication channels – like instant messaging, shared scheduling systems, or even whiteboards – facilitate real-time coordination and responsiveness to unexpected events.
Q 11. Describe your experience with various triage systems (e.g., ESI, Manchester).
I have extensive experience with various triage systems, including the Emergency Severity Index (ESI) and the Manchester Triage System. The ESI is a five-level system used primarily in emergency departments to prioritize patients based on their acuity (how sick they are). It’s a structured approach using specific criteria to assign patients a level from 1 (most urgent) to 5 (least urgent). The Manchester system is similar but offers a more detailed assessment, with different pathways for different types of presentations. My experience includes using these systems to streamline patient assessment, optimize resource allocation, and enhance the overall efficiency of patient care. I understand their respective strengths and limitations, and adapt my approach accordingly, ensuring patient safety and timely treatment based on their needs.
Q 12. How do you handle situations where resources are limited?
Resource limitations necessitate a strategic approach to patient flow. When faced with limited staff, beds, or equipment, prioritization becomes critical. We use triage systems effectively to identify and prioritize patients according to their medical needs, focusing on those with the most urgent conditions. We might implement strategies like: optimizing appointment scheduling to maximize utilization, re-allocating staff to areas of greatest need, and postponing elective procedures. We also engage in proactive communication with patients and their families, keeping them informed about any potential delays or adjustments to care plans. For example, if we are facing a bed shortage, we might collaborate with nearby facilities to transfer less acute patients. Transparent and empathetic communication is key to mitigating patient anxiety during resource constraints.
Q 13. What is your understanding of patient throughput and how do you improve it?
Patient throughput refers to the number of patients processed or treated within a specific time period. Improving throughput involves a multifaceted approach. It starts with optimizing the various stages of the patient journey, reducing wait times at each step, including registration, triage, examination, and discharge. Streamlining processes, improving staff efficiency, and investing in appropriate technology (like electronic health records and appointment scheduling systems) all contribute. Efficient use of space and resources, such as optimizing examination room allocation and using advanced imaging technologies to reduce the length of patient stays, also increases throughput. For example, we can reduce wait times by utilizing online pre-registration, improving communication between departments, and empowering nursing staff to manage certain tasks independently.
Q 14. How do you ensure patient confidentiality and HIPAA compliance during triage?
Maintaining patient confidentiality and HIPAA compliance is paramount during triage. All information collected during triage is treated as protected health information (PHI). We strictly adhere to HIPAA regulations, which includes using secure systems for recording and storing patient data, limiting access to PHI only to authorized personnel, and providing patients with clear explanations of how their information is used. We also use coded identifiers instead of names wherever possible, and securely dispose of any paper documents containing PHI. Training all staff members on HIPAA regulations is essential to ensure a culture of compliance and to prevent breaches of patient privacy. Furthermore, we implement and regularly review our security protocols to proactively address any potential vulnerabilities.
Q 15. Describe your experience with patient scheduling and appointment management.
Patient scheduling and appointment management are crucial for efficient healthcare delivery. My experience encompasses the entire process, from initial patient contact and appointment booking to managing appointment reminders and cancellations. I’ve worked with various scheduling systems, including both paper-based and electronic systems, and am proficient in optimizing schedules to maximize provider time while minimizing patient wait times. For example, in my previous role, I implemented a new appointment scheduling software that reduced patient wait times by 15% by optimizing appointment durations and incorporating buffer time between appointments to account for unexpected delays. I also developed a system for prioritizing urgent appointments, ensuring that patients requiring immediate attention were seen promptly.
My experience includes:
- Utilizing various scheduling software to book, modify, and cancel appointments.
- Implementing strategies to minimize no-shows and cancellations.
- Managing complex schedules for multiple providers across various specialties.
- Coordinating appointments with specialists and other healthcare professionals.
- Developing and implementing efficient appointment reminder systems (e.g., SMS, email, automated phone calls).
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you handle patient cancellations or no-shows?
Handling patient cancellations and no-shows requires a multi-pronged approach. The first step is to understand the reason for the cancellation or no-show. Was it due to unforeseen circumstances, a scheduling conflict, or lack of communication? Once the reason is identified, I tailor my response accordingly. For unavoidable cancellations, I offer empathy and reschedule the appointment as soon as possible. For no-shows, I initiate a follow-up call to understand the situation and prevent future occurrences. This may involve reinforcing appointment reminders or discussing alternative communication methods.
I also utilize data analysis to identify patterns in cancellations and no-shows. For instance, if a particular time slot consistently has a high cancellation rate, it might indicate a need to adjust the scheduling strategy or improve communication surrounding appointments.
My approach includes:
- Implementing robust appointment reminder systems.
- Following up with patients who cancel or do not show up for appointments.
- Analyzing cancellation and no-show data to identify trends and improve scheduling practices.
- Offering flexible scheduling options to accommodate patient needs.
- Communicating clearly and effectively with patients regarding appointment policies.
Q 17. Explain your experience with different patient populations (e.g., pediatrics, geriatrics).
My experience spans diverse patient populations, including pediatrics, geriatrics, and adults with various medical needs. Working with pediatric patients requires a different approach than working with geriatric patients. With children, I prioritize creating a calm and playful environment to reduce anxiety. Clear, simple communication with parents or guardians is essential. For elderly patients, I take extra care to ensure they feel comfortable and understood, often providing additional time for their needs and considering potential physical limitations. I understand that communication and care must be tailored to the individual’s cognitive and physical abilities, as well as their cultural background.
For example, when working with geriatric patients with cognitive impairments, I use visual aids and simple language to enhance understanding. With pediatric patients, I involve parents or guardians in the process, explaining procedures in age-appropriate terms while reassuring them.
Q 18. How do you adapt your communication style to meet the needs of diverse patient populations?
Adapting communication style is paramount to effective patient care. I employ active listening techniques and adjust my language and tone based on the patient’s age, cultural background, and health literacy. For example, I use clear and concise language with limited medical jargon when communicating with patients who have limited health literacy. With patients from diverse cultural backgrounds, I’m mindful of cultural sensitivities and communication preferences. I strive to create a safe and comfortable environment where patients feel heard and understood.
Techniques I use include:
- Using plain language and avoiding medical jargon.
- Employing active listening and empathetic communication.
- Being mindful of cultural differences and communication styles.
- Using visual aids and other tools to enhance understanding.
- Confirming understanding with patients by asking clarifying questions.
Q 19. Describe your proficiency in using electronic health records (EHRs) for patient flow management.
I am proficient in using various EHR systems for patient flow management. This includes using EHR functionalities for appointment scheduling, patient registration, check-in/check-out processes, and managing patient data. I understand how to utilize EHR features to optimize patient flow, such as automated appointment reminders, electronic intake forms, and real-time updates on patient status. My experience includes using EHR systems to track patient wait times, identify bottlenecks in the patient flow process, and generate reports to monitor key performance indicators.
For example, I’ve used EHR data to identify peak appointment times and adjust staffing levels accordingly to minimize patient wait times. I’ve also used the EHR’s reporting functionalities to track key performance indicators (KPIs) such as patient satisfaction scores and appointment adherence rates to improve workflow and patient experience.
Q 20. How do you handle unexpected patient arrivals or changes in schedule?
Handling unexpected patient arrivals or schedule changes requires flexibility and quick thinking. My approach involves assessing the situation, prioritizing patients based on urgency, and communicating effectively with the team and patients. I utilize the EHR to update patient information and communicate any changes to the healthcare team. If a patient arrives unexpectedly, I evaluate their condition and determine the appropriate course of action, ensuring they receive timely and appropriate care. Schedule changes are communicated promptly to the affected parties, and appointments are rescheduled as needed, minimizing disruption.
In a real-world scenario, a patient might arrive without an appointment due to a medical emergency. I would immediately assess the situation, determine the severity of the condition, and arrange for them to be seen by a provider as quickly as possible, often prioritizing them over scheduled appointments.
Q 21. What strategies do you use to reduce patient anxiety during triage?
Reducing patient anxiety during triage is crucial for a positive patient experience. My strategies include creating a welcoming and calming environment, providing clear and concise explanations, and actively listening to the patient’s concerns. I use reassuring language and maintain eye contact to build rapport. I prioritize empathy and understanding, acknowledging the patient’s feelings and providing reassurance. Furthermore, I ensure that the triage process is efficient and minimizes wait times. For patients experiencing high anxiety, I might offer comfort measures such as offering a warm blanket or a drink of water.
For example, I might say something like, “I understand you’re feeling anxious; let’s take a few minutes to get you settled and explain what will happen next.” This demonstrates empathy and provides a sense of control for the patient. In cases of severe anxiety, I may consult with a healthcare professional to provide additional support.
Q 22. How do you ensure accurate documentation of patient assessments and treatment plans during triage?
Accurate documentation is the cornerstone of effective patient care. In triage, this means meticulously recording all assessments and treatment plans to ensure continuity of care and legal compliance. This involves using a standardized system, whether electronic or paper-based, with clearly defined fields for all relevant data.
- Patient Demographics: Accurate recording of name, date of birth, contact information, and medical record number is essential for identification and tracking.
- Presenting Complaint: A detailed description of the reason for the patient’s visit, using the patient’s own words where possible, helps determine the urgency of the situation.
- Vital Signs: Thorough recording of temperature, heart rate, blood pressure, respiratory rate, and oxygen saturation provides objective data to assess the patient’s condition.
- Assessment Findings: A concise and comprehensive account of the physical examination, including observations, palpation, auscultation, and any other relevant findings. This should include noting any allergies or current medications.
- Treatment Plan: Detailed documentation of the triage decisions, including the urgency level assigned, any interventions performed (e.g., medication administration, wound care), and referral to another healthcare professional or department.
For example, instead of simply noting ‘chest pain,’ I would document: ‘Patient reports substernal chest pressure radiating to the left arm, onset 30 minutes ago, associated with diaphoresis and shortness of breath. Denies nausea or vomiting.’ This level of detail ensures clear communication and avoids ambiguity.
Q 23. How would you address a situation where a patient becomes agitated or angry while waiting?
Dealing with an agitated or angry patient requires a calm and empathetic approach. The key is to de-escalate the situation while ensuring the patient’s safety and the safety of others. My approach would involve:
- Active Listening: Allowing the patient to express their concerns without interruption, showing genuine empathy and understanding. This often helps the patient feel heard and less frustrated.
- Validation: Acknowledging the patient’s feelings, even if I don’t agree with their perspective. For instance, saying ‘I understand you’re frustrated with the wait time’ can go a long way.
- Calm Communication: Maintaining a calm, reassuring tone, using clear and concise language. Avoiding confrontation or raising my voice is paramount.
- Problem-Solving: Offering solutions to address the patient’s concerns whenever possible. This might involve offering a more comfortable waiting area, providing updates on their wait time, or explaining the triage process.
- Seeking Assistance: If the situation escalates beyond my ability to manage, I would immediately seek assistance from a supervisor, security personnel, or other members of the healthcare team. Patient safety is the utmost priority.
For example, if a patient is angry about a long wait time, I might say: ‘I understand this is frustrating, and I apologize for the delay. Let me check on your estimated wait time and see if there’s anything we can do to make you more comfortable while you wait.’
Q 24. Describe a time you had to make a quick decision in a high-pressure triage situation.
During a busy shift, a patient presented with severe respiratory distress. He was cyanotic (bluish discoloration of the skin), struggling to breathe, and exhibiting signs of significant anxiety. His initial vital signs were alarming: low oxygen saturation and rapid, shallow breathing. Given the critical nature of his condition, immediate intervention was crucial.
I prioritized him over other patients waiting, bypassing the usual order based on chief complaint and vital signs. I immediately called for respiratory support, initiated high-flow oxygen, and contacted the emergency physician. Simultaneously, I communicated clearly with the waiting patients, explaining the situation and reassuring them that the critical patient was receiving the necessary attention.
This quick decision, guided by clinical judgment and a prioritization of immediate life threats, ultimately resulted in the stabilization of the patient. While this was stressful, my training and experience allowed me to swiftly assess the situation and take appropriate action. The immediate response likely saved the patient’s life, and the clear communication reduced anxiety among other waiting patients.
Q 25. What are your strengths and weaknesses related to patient flow and triage?
My strengths in patient flow and triage include strong clinical judgment, efficient prioritization skills, and effective communication. I’m adept at quickly assessing patient acuity and making sound decisions under pressure, ensuring optimal resource allocation. I’m also a skilled communicator, capable of interacting calmly and professionally with patients of all backgrounds, even during stressful situations.
My area for improvement lies in delegating tasks more effectively. While I’m efficient, I sometimes take on too much myself. I’m actively working on improving this by proactively assigning tasks and empowering my team members to take on more responsibility. This is a work in progress, and I am committed to refining this skill.
Q 26. How do you stay updated on current best practices in patient flow management?
Staying updated on best practices in patient flow management requires a multifaceted approach. I regularly participate in continuing medical education (CME) courses and workshops focusing on triage, emergency medicine, and patient flow optimization. I also actively seek out relevant journal articles and research studies. Professional memberships, such as those offered by relevant medical associations, provide access to the latest guidelines and best practices. Additionally, I actively participate in professional networks and attend conferences to learn from colleagues and experts in the field. Following key healthcare organizations and regulatory bodies on social media and through their publications is another important strategy.
Q 27. Describe your approach to continuous improvement in patient flow and triage processes.
My approach to continuous improvement involves a cyclical process focusing on data analysis, process evaluation, and implementation of changes. This starts with collecting data on patient wait times, throughput, and patient satisfaction scores. This data is then analyzed to identify bottlenecks and areas for improvement. We then implement changes, pilot them, and assess the impact of those changes. After evaluating the outcome of implemented changes, we iterate, refining our processes for even greater efficiency and patient satisfaction. For example, if our data indicates long wait times in a specific area, we might explore options such as optimizing staffing levels, improving patient registration processes, or implementing a new queuing system. This iterative process is key to continuous improvement.
Q 28. How do you contribute to a positive and efficient team environment?
Contributing to a positive and efficient team environment is crucial for successful patient flow. I believe in fostering open communication, mutual respect, and collaboration. I actively participate in team meetings, sharing my expertise and offering support to colleagues. I’m always willing to help out when needed, regardless of my assigned tasks. I encourage teamwork through proactive communication and by celebrating successes as a team. I also believe in providing constructive feedback to both my colleagues and myself, focusing on continuous growth and improvement. A positive team atmosphere translates directly into efficient and high-quality patient care.
Key Topics to Learn for Manage Patient Flow and Triage Interview
- Patient Prioritization & Triage Systems: Understanding different triage systems (e.g., ESI, Manchester), prioritization algorithms, and their application in various healthcare settings. Consider the ethical implications of prioritization decisions.
- Optimizing Patient Flow: Explore strategies for efficient patient movement through the healthcare system, including appointment scheduling, resource allocation, wait time management, and effective communication with patients and staff. Practical application: Analyze a scenario with a congested waiting room and propose solutions.
- Communication & Teamwork: Effective communication skills are crucial. Focus on clear and concise communication with patients, doctors, nurses, and other healthcare professionals. Consider the importance of teamwork in managing patient flow and resolving conflicts.
- Data Analysis & Reporting: Learn how to collect, analyze, and interpret data related to patient flow and triage. This includes understanding key performance indicators (KPIs) like wait times, patient satisfaction, and resource utilization. Practical application: Interpret data to identify bottlenecks in patient flow and suggest improvements.
- Emergency Response & Crisis Management: Understand procedures for handling emergencies and critical situations. This includes recognizing and responding to life-threatening conditions and coordinating resources effectively during crises. Consider the importance of maintaining calm and composure under pressure.
- Technology & Systems: Familiarity with electronic health records (EHRs), patient scheduling software, and other relevant technologies used in managing patient flow and triage is beneficial. Understanding how these systems support efficient workflow is key.
- Regulatory Compliance & Legal Aspects: Understand relevant healthcare regulations and legal considerations related to patient privacy (HIPAA), safety, and liability. This includes understanding informed consent and maintaining patient confidentiality.
Next Steps
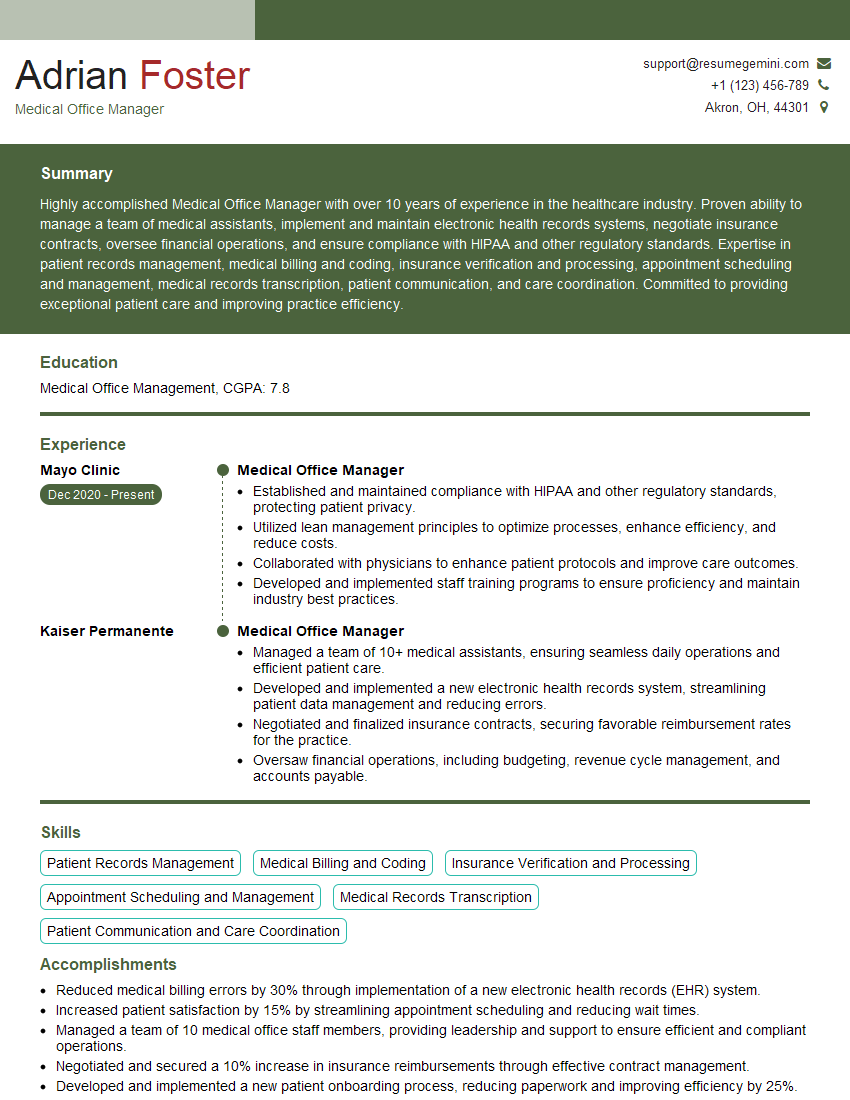
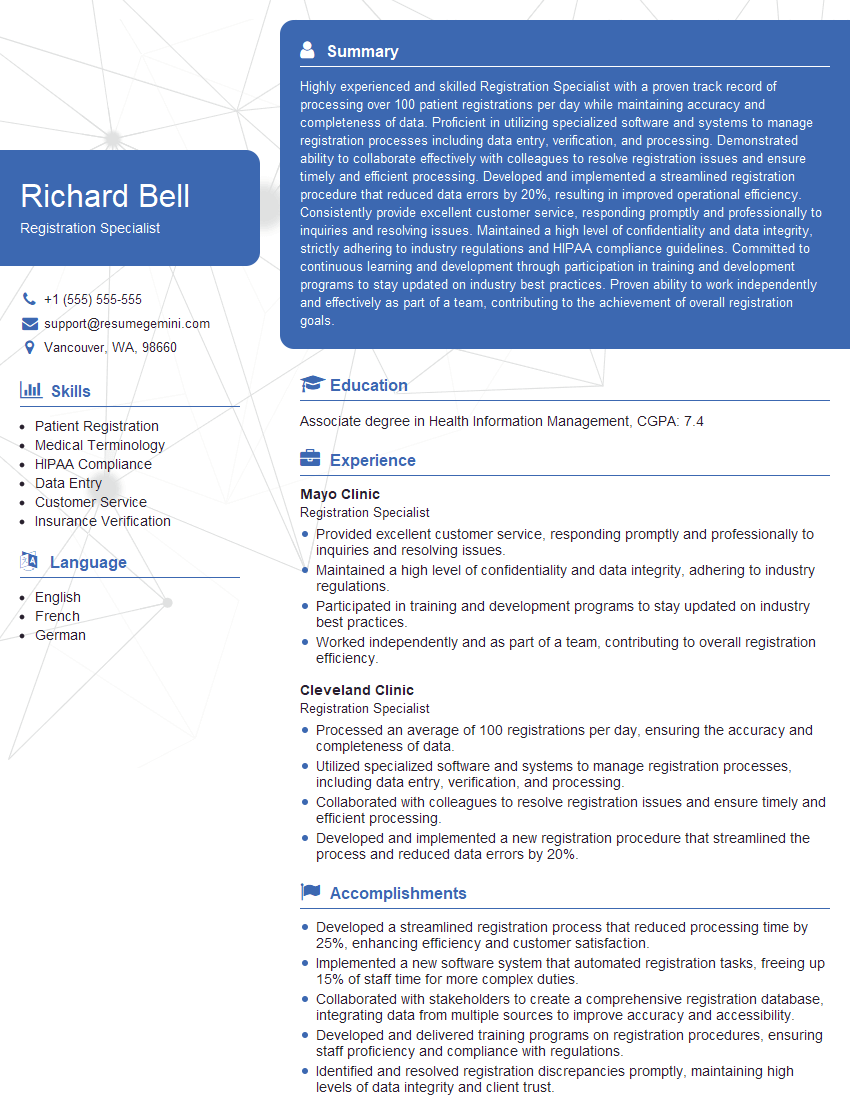
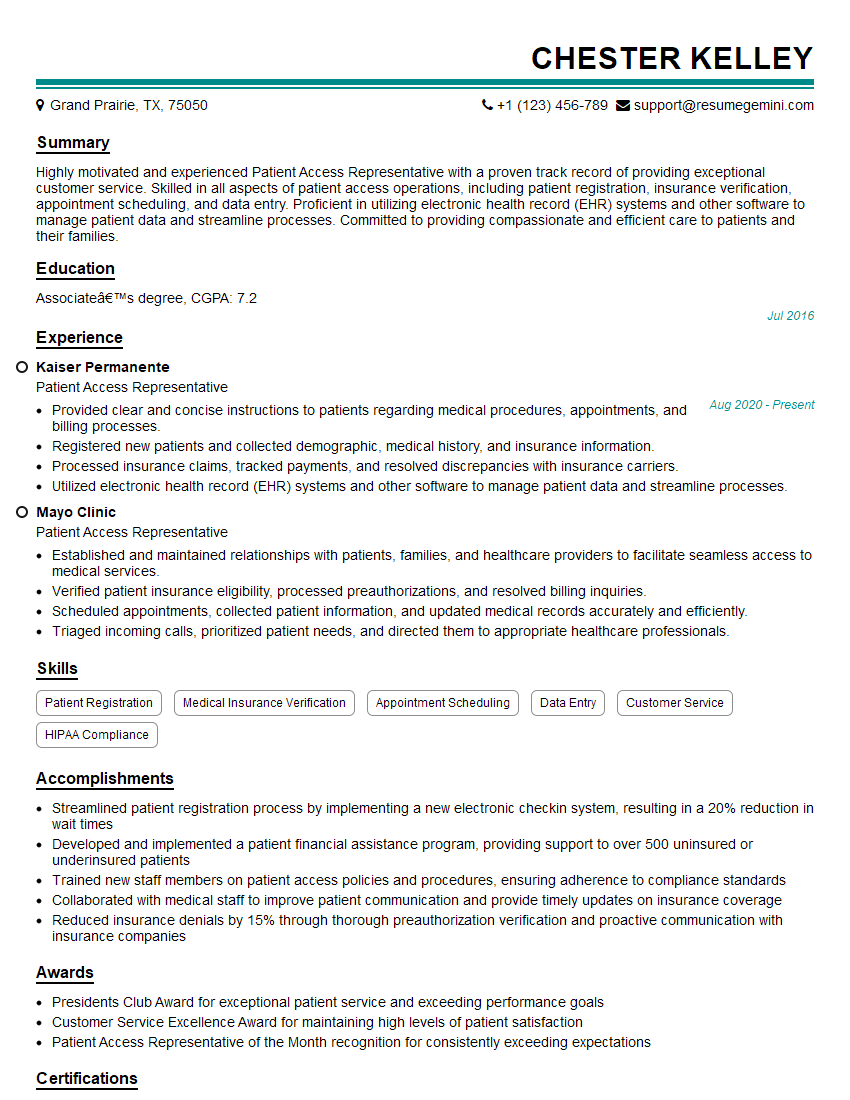
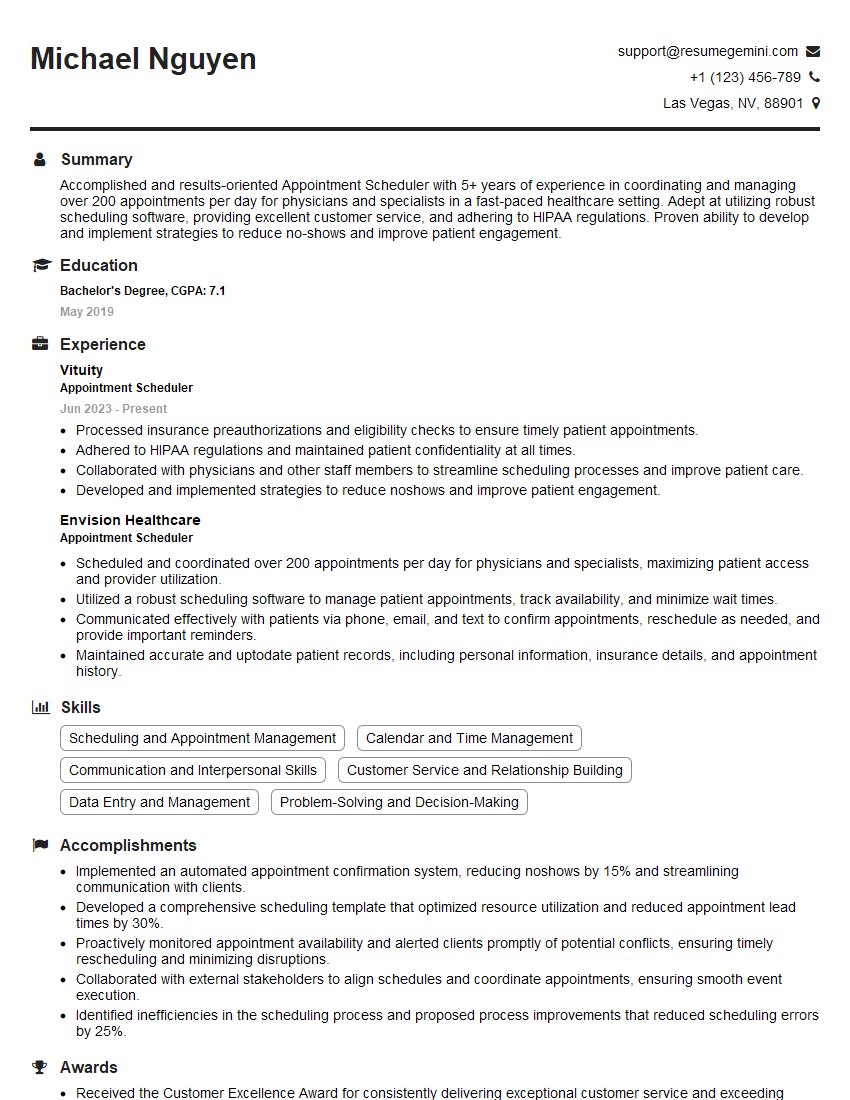
Mastering Manage Patient Flow and Triage significantly enhances your value in any healthcare setting, opening doors to leadership roles and increased responsibility. A strong resume is crucial for showcasing your skills and experience to potential employers. Creating an ATS-friendly resume is essential to ensure your application gets noticed. ResumeGemini is a trusted resource that can help you build a professional and effective resume tailored to highlight your accomplishments in Manage Patient Flow and Triage. Examples of resumes tailored to this specific area are available to guide you.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Amazing blog
hello,
Our consultant firm based in the USA and our client are interested in your products.
Could you provide your company brochure and respond from your official email id (if different from the current in use), so i can send you the client’s requirement.
Payment before production.
I await your answer.
Regards,
MrSmith
hello,
Our consultant firm based in the USA and our client are interested in your products.
Could you provide your company brochure and respond from your official email id (if different from the current in use), so i can send you the client’s requirement.
Payment before production.
I await your answer.
Regards,
MrSmith
These apartments are so amazing, posting them online would break the algorithm.
https://bit.ly/Lovely2BedsApartmentHudsonYards
Reach out at [email protected] and let’s get started!
Take a look at this stunning 2-bedroom apartment perfectly situated NYC’s coveted Hudson Yards!
https://bit.ly/Lovely2BedsApartmentHudsonYards
Live Rent Free!
https://bit.ly/LiveRentFREE
Interesting Article, I liked the depth of knowledge you’ve shared.
Helpful, thanks for sharing.
Hi, I represent a social media marketing agency and liked your blog
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?