Are you ready to stand out in your next interview? Understanding and preparing for Autoclave Loading and Unloading interview questions is a game-changer. In this blog, we’ve compiled key questions and expert advice to help you showcase your skills with confidence and precision. Let’s get started on your journey to acing the interview.
Questions Asked in Autoclave Loading and Unloading Interview
Q 1. Explain the different types of autoclaves and their applications.
Autoclaves are sterilization chambers that use high-pressure saturated steam to kill microorganisms. Different types cater to specific needs.
- Gravity Displacement Autoclaves: These are the simplest and most common type. Sterilization relies on gravity to displace air with steam. They’re ideal for simple loads and are often found in smaller clinics or labs. Think of it like filling a container with water – the heavier water pushes the lighter air out.
- Pre-vacuum Autoclaves: These use a vacuum pump to remove air before steam enters, ensuring faster and more thorough sterilization. They are preferred for wrapped instruments and porous materials that are difficult to sterilize completely due to air pockets. Imagine vacuum-sealing a bag before cooking – it ensures even heating.
- High-Speed/Flash Autoclaves: Designed for rapid sterilization cycles, often used for instruments requiring quick turnaround time. These autoclaves usually have a smaller chamber and shorter cycles.
- Steam-Formaldehyde Autoclaves: These use a combination of steam and formaldehyde for sterilization, primarily employed for sterilizing materials sensitive to high temperatures. They’re less common due to the toxicity of formaldehyde.
The choice of autoclave depends on the type and volume of materials to be sterilized, the required cycle time, and budget considerations. For instance, a large hospital might use pre-vacuum autoclaves for their high volume and requirement for thorough sterilization, while a smaller dental office may opt for a gravity displacement unit.
Q 2. Describe the proper procedure for loading an autoclave.
Proper autoclave loading is crucial for effective sterilization. It’s all about ensuring steam penetrates every item.
- Prepare Items: Wrap instruments in appropriate sterilization wrappers or pouches. Ensure all items are clean and free from debris.
- Arrange Items: Place items loosely and evenly in the autoclave. Avoid overcrowding, which can impede steam penetration. Imagine trying to cook a dense casserole – it won’t heat evenly. Leave space between items and allow for steam circulation.
- Orientation: Position instruments vertically to allow for better steam penetration. Hollow items like surgical instruments should be placed with their openings up to allow for air to escape and steam to enter.
- Loading Trays: Use perforated trays to allow for good steam distribution. Don’t stack trays too high.
- Avoid Overloading: Overloading hinders steam penetration leading to incomplete sterilization. Always adhere to the autoclave manufacturer’s guidelines regarding maximum load capacity.
Consistent and proper loading technique is critical to achieving sterile items. Overloading, for example, can lead to potential sterilization failures, resulting in the need for reprocessing and compromising patient safety.
Q 3. What are the critical factors to consider when loading an autoclave to ensure effective sterilization?
Effective sterilization hinges on several key factors during autoclave loading:
- Steam Penetration: The steam must reach all surfaces of every item. Overloading, improper wrapping, and tightly packed items hinder steam penetration.
- Air Removal: Air pockets prevent effective sterilization because air is a poor conductor of heat. Pre-vacuum autoclaves are designed to address this.
- Temperature and Pressure: Achieving and maintaining the correct temperature and pressure for the designated cycle duration is paramount. This ensures the necessary lethality against microorganisms.
- Cycle Time: The cycle must run for the sufficient duration to effectively kill all microorganisms. This is determined by the type of load and the autoclave’s parameters.
- Load Size: Avoid exceeding the maximum load capacity. An overloaded autoclave will not sterilize items properly.
Failing to consider any of these can lead to sterilization failure, with potentially serious consequences. For example, incomplete sterilization of surgical instruments can lead to infections in patients.
Q 4. How do you prevent contamination during autoclave loading?
Preventing contamination during autoclave loading requires meticulous attention to detail:
- Cleanliness: Ensure all items to be sterilized are thoroughly cleaned before loading. Any organic matter can shield microorganisms, reducing the effectiveness of the sterilization process.
- Proper Wrapping: Use appropriate sterilization wrappers or pouches to prevent recontamination after sterilization. These wrappers should be intact and free of tears or punctures.
- Aseptic Technique: Maintain aseptic technique – this means following sterile procedures and minimizing the risk of introducing microorganisms to the load. Wear appropriate PPE like gloves.
- Handling: Handle sterile items carefully after sterilization to avoid contamination. Avoid touching the surfaces that have to remain sterile.
- Clean Autoclave Chamber: Regularly clean and maintain the autoclave chamber itself to prevent the build-up of debris and microbial contamination.
Think of it like baking a cake – you wouldn’t use a dirty pan! Maintaining cleanliness ensures the sterilization process is as effective as possible.
Q 5. What are the safety precautions to follow when loading and unloading an autoclave?
Safety is paramount when handling autoclaves:
- Personal Protective Equipment (PPE): Always wear appropriate PPE, including heat-resistant gloves and eye protection, when loading and unloading the autoclave.
- Hot Surfaces: Be aware that the autoclave chamber and its contents will be extremely hot after a sterilization cycle. Allow sufficient time for cooling before opening.
- Pressure Relief: Never attempt to force open the autoclave door while it is under pressure. Wait for the pressure to release naturally.
- Steam Release: Be cautious of escaping steam when opening the autoclave door, as it can cause burns. Open the door slowly and carefully.
- Proper Training: Ensure you are properly trained in the operation and safety procedures of the specific autoclave model you are using.
Ignoring safety protocols can lead to serious injuries such as burns or scalds. Following these guidelines is not only important for the operator’s safety, but also essential for preventing potential damage to the equipment.
Q 6. Explain the proper procedure for unloading an autoclave.
Unloading an autoclave requires a systematic approach to avoid contamination and injuries:
- Allow Cooling: Allow the autoclave to cool down completely before opening the door. This is crucial to prevent burns and ensure safe handling of sterilized items.
- Open Carefully: Open the door slowly and carefully to avoid being scalded by escaping steam.
- Aseptic Technique: Maintain aseptic technique throughout the unloading process. Wear appropriate PPE.
- Remove Items Carefully: Carefully remove items from the autoclave, avoiding touching the sterile surfaces. Use tongs or other appropriate tools as needed.
- Inspect Items: Visually inspect the items for any signs of damage or improper sterilization (like indicators that haven’t changed color).
- Proper Storage: Once removed, store the sterilized items appropriately to prevent recontamination.
Proper unloading ensures that the sterile items remain sterile and that they are handled safely, avoiding accidental contamination or injury to personnel.
Q 7. How do you identify and handle improperly sterilized items?
Identifying and handling improperly sterilized items is critical to prevent infection and ensure patient safety.
- Biological Indicators (BIs): BIs are essential for confirming sterilization. If a BI doesn’t show sterilization, it indicates a problem in the process. This requires investigation into the cause of failure, and discarding or re-sterilizing affected items.
- Chemical Indicators (CIs): CIs change color when exposed to the sterilization conditions. If a CI hasn’t changed color, this is a clear indication that item didn’t undergo proper sterilization. Similar to BIs, immediate action is required.
- Visual Inspection: Always conduct a visual inspection of sterilized items to identify any damage or signs of contamination.
- Documentation: Maintaining detailed records of sterilization cycles and BI/CI results is essential for tracking and tracing sterilization processes and identifying potential problems.
- Disposal: If items are determined to be improperly sterilized, they must be discarded according to established protocols to avoid accidental use.
Ignoring improperly sterilized items poses serious risks. Thorough checks and proper disposal are critical in maintaining high standards of hygiene and patient safety.
Q 8. What are the indicators you check to confirm sterilization?
Confirming sterilization goes beyond just relying on the autoclave’s completion signal. We use a multi-pronged approach involving several indicators to ensure the process was successful. These indicators provide independent verification that the required parameters – temperature, pressure, and duration – were met throughout the sterilization cycle.
Biological Indicators (BIs): These are the gold standard. BIs contain spores of a specific microorganism (like Geobacillus stearothermophilus for steam sterilization) that are highly resistant to the sterilization process. After the cycle, the BI is incubated. If the spores are killed (no growth), sterilization is confirmed. If growth occurs, it indicates a sterilization failure requiring investigation.
Chemical Indicators (CIs): These are less precise than BIs but offer immediate visual confirmation that the sterilization process occurred. They change color when exposed to the specific conditions within the autoclave. These are often found as tape strips or internal indicators integrated into packaging. While CIs show the process *happened*, they don’t guarantee the spores were killed, highlighting the need for BIs.
Mechanical Indicators: These are part of the autoclave itself – temperature and pressure gauges, cycle timers. They provide a record of the parameters during the cycle. These alone are insufficient to confirm sterility, serving mainly as a record of operation.
For example, in a recent surgery pack sterilization, we used both a BI and CI. The CI changed color correctly, indicating exposure to the sterilization parameters. We then incubated the BI; its negative result confirmed the sterilization of all materials in the pack.
Q 9. How do you ensure the proper documentation of autoclave cycles?
Proper documentation is crucial for traceability and quality control in sterilization. We follow a rigorous system to record and maintain autoclave cycle data. This typically involves a combination of electronic and paper records.
Electronic Logging: Modern autoclaves have built-in data loggers that automatically record parameters such as temperature, pressure, time, and cycle duration. This data is stored digitally and often can be exported for analysis and audit trails.
Printed Records: Many autoclaves also provide a printed record of each cycle, summarizing the key parameters. These printouts are filed according to established procedures.
Manual Logbooks: Even with electronic logging, we maintain a manual logbook. This includes details like the date, time, cycle type, load contents (with identification numbers), BI/CI results, and any comments regarding the cycle. This helps build a comprehensive record in case of electronic system malfunctions.
Batch Identification: All items are identified with unique batch numbers to trace them through the entire process, from cleaning and preparation to post-sterilization storage.
Imagine a situation where a post-operative infection occurs. Meticulous documentation allows us to quickly trace the origin of the instruments, the specific autoclave cycle used, and the results of the sterilization indicators to determine if there was any failure in the process.
Q 10. What are the common causes of autoclave malfunctions?
Autoclave malfunctions can stem from a variety of causes, ranging from minor operational issues to more serious mechanical problems. Regular maintenance and operator training are key to minimizing these issues.
Air Leaks: Air trapped in the chamber prevents proper steam penetration, compromising sterilization. This can result from faulty door seals or improperly loaded instruments.
Malfunctioning Sensors: Incorrect readings from temperature or pressure sensors lead to inaccurate cycle parameters. The autoclave might seem to have run correctly, but sterilization wasn’t achieved.
Faulty Heating Elements: If the heating elements fail to reach the required temperature, sterilization is impossible.
Blocked Drains: Water drainage problems affect pressure regulation and steam generation within the autoclave.
Power Supply Issues: Interruptions or problems with the power supply can cause the cycle to stop prematurely or not start at all.
For example, we once experienced a cycle failure due to a blocked drain. The resulting pressure inconsistencies prevented proper steam generation, highlighting the importance of regular maintenance checks.
Q 11. How do you troubleshoot a malfunctioning autoclave?
Troubleshooting a malfunctioning autoclave requires a systematic approach. Safety is paramount, and if there’s any doubt, the autoclave should be shut down and a qualified technician contacted.
Safety First: Ensure the autoclave is safely shut down following the manufacturer’s instructions.
Identify the Problem: Note down any error messages displayed on the console and check the manual logbook for any unusual behavior in recent cycles.
Visual Inspection: Check for any obvious problems, such as leaks around the door seals, water buildup, or any signs of damage.
Sensor Checks: If possible and safe, check the readings of the temperature and pressure sensors to see if they are accurate.
Test Run (after safety checks and with appropriate supervision): After addressing obvious issues, a test run with empty chamber may be performed to evaluate if the basic functions are operating correctly, following manufacturer instructions.
Documentation: Record all observations, actions taken, and results throughout the troubleshooting process.
Professional Assistance: If the problem cannot be easily identified or resolved, contact a qualified service technician. Do not attempt to repair the autoclave yourself unless you are properly trained.
In one case, a seemingly simple error message pointed towards a faulty pressure sensor. Replacing the sensor resolved the issue and prevented further sterilization failures.
Q 12. Describe your experience with different types of sterilization indicators.
My experience encompasses a wide range of sterilization indicators, each with its strengths and limitations. The choice of indicator depends on the specific application and required level of assurance.
External Chemical Indicators: These are typically tape strips or labels that change color when exposed to the required temperature and steam. They provide a simple visual check that the autoclave reached the necessary conditions but don’t guarantee sterility.
Internal Chemical Indicators: These are integrated into packaging materials. They indicate exposure to steam and time parameters, providing better assurance compared to external indicators, but still not a guarantee of sterility.
Biological Indicators: These are the most reliable indicators. They contain heat-resistant bacterial spores, which, when killed, confirm that the process achieved true sterility. Different types of BIs are available for various sterilization methods.
Multi-parameter Indicators: These indicators combine chemical and sometimes physical indicators for a more comprehensive record of the sterilization process, offering both visual confirmation and some indication of process completion.
For example, when sterilizing surgical instruments, we always use BIs for definitive sterility confirmation along with internal chemical indicators to visually verify the package was exposed to the correct sterilization parameters.
Q 13. How do you manage the disposal of contaminated materials after autoclave use?
Disposal of contaminated materials after autoclave use is governed by strict safety protocols to prevent the spread of infectious agents. We adhere to both institutional and local regulations regarding biohazardous waste disposal.
Appropriate Containers: All contaminated materials are placed in designated autoclave bags or containers specifically designed for biohazardous waste. These are autoclaved to decontaminate the materials.
Waste Segregation: Different types of waste (e.g., sharps, liquids, solid waste) are segregated according to the institution’s guidelines to ensure proper handling and disposal.
Labeling: All containers are clearly labeled as biohazardous waste, including the date and contents.
Authorized Disposal: The labeled containers are then handed over to the designated waste management personnel or a licensed medical waste disposal service.
Think of it like this: the autoclave renders the waste non-infectious, but the proper handling and disposal procedures are essential to prevent any accidental exposure or environmental contamination.
Q 14. Explain the importance of proper cleaning and preparation of instruments before autoclaving.
Proper cleaning and preparation of instruments *before* autoclaving are crucial for effective sterilization. The autoclave kills microorganisms, but it cannot remove soil, debris, or organic matter. These materials can interfere with steam penetration and prevent effective sterilization of the instruments.
Pre-cleaning: This involves removing visible debris and organic matter from instruments using appropriate brushes, detergents, and enzymatic cleaners. It involves washing and rinsing thoroughly to remove all traces of soil and potential contaminants.
Inspection: A thorough visual inspection should be carried out to check for any damage or defects in the instruments before sterilization.
Drying: Instruments must be thoroughly dried to avoid corrosion and prevent the formation of water spots which can interfere with the sterilizing process.
Packaging: Instruments are carefully packaged in appropriate sterilization pouches or wraps to maintain sterility after the autoclave cycle.
Imagine trying to sterilize a knife covered in food residue – the autoclave won’t be able to effectively penetrate the debris to kill the microbes. Proper pre-cleaning is the foundation of effective sterilization and is critical for patient safety.
Q 15. What is the difference between gravity displacement and pre-vacuum autoclaves?
The main difference between gravity displacement and pre-vacuum autoclaves lies in how they remove air from the chamber before sterilization. Gravity displacement autoclaves rely on steam pushing air out of the chamber as steam enters. Think of it like filling a glass of water – the water (steam) displaces the air. This method is slower and less effective at removing air pockets, which can prevent proper sterilization. Pre-vacuum autoclaves, on the other hand, actively remove air from the chamber using a vacuum pump *before* steam is introduced. This ensures complete steam penetration and more efficient sterilization. Imagine a vacuum cleaner sucking out the air before you fill the glass with water – much more thorough, right?
In a nutshell:
- Gravity Displacement: Slower, less effective air removal, potential for air pockets.
- Pre-Vacuum: Faster, more effective air removal, superior sterilization.
The choice between the two depends on the application and the level of sterility required. Pre-vacuum autoclaves are generally preferred for critical applications where complete sterilization is paramount, while gravity displacement might suffice for less critical items.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. What are the limitations of autoclave sterilization?
Autoclave sterilization, while highly effective, has certain limitations. It’s not suitable for all materials. For example, certain plastics and materials sensitive to high heat and pressure can melt, warp, or degrade. Also, the effectiveness depends heavily on proper loading techniques. Overcrowding or improper wrapping can create air pockets, hindering steam penetration and rendering the sterilization process ineffective. Additionally, certain substances, like prions, may be resistant to standard autoclave cycles, requiring specialized procedures.
Other limitations include:
- Material incompatibility: Some materials cannot withstand the high temperatures and pressures.
- Incomplete sterilization: Improper loading or malfunctioning equipment can lead to inadequate sterilization.
- Limited efficacy against certain agents: Some biological agents, such as prions, may require more aggressive sterilization methods.
It’s crucial to understand these limitations and choose the appropriate sterilization method and loading techniques to ensure the desired level of sterility.
Q 17. What are the regulatory requirements for autoclave operation and maintenance?
Regulatory requirements for autoclave operation and maintenance vary depending on location and the specific application (e.g., healthcare, research, manufacturing). However, common requirements generally include:
- Regular testing and validation: This usually involves biological indicators (BIs) and chemical indicators (CIs) to verify sterilization efficacy. Records must be meticulously maintained.
- Operator training and competency: Personnel operating the autoclave must receive adequate training on proper loading, operation, and safety procedures.
- Maintenance and calibration logs: Detailed records of preventative maintenance, calibration checks, and any repairs must be kept.
- Compliance with relevant standards: Adherence to standards such as those set by the FDA, ISO, or other relevant regulatory bodies is crucial.
- Safety protocols: Strict adherence to safety protocols, including appropriate personal protective equipment (PPE), is necessary to prevent accidents.
Failure to meet these requirements can lead to serious consequences, including infection control breaches, compromised product sterility, and potential legal liabilities. Thorough documentation is key to demonstrating compliance.
Q 18. How do you maintain the autoclave’s log books and records?
Maintaining autoclave log books and records requires meticulous attention to detail. Each logbook entry should be clear, concise, and include essential information such as:
- Date and time of cycle: Precise recording is crucial for traceability.
- Cycle type and parameters: Specify the type of cycle (e.g., liquid, wrapped goods) and the temperature, pressure, and duration.
- Materials sterilized: Detail the items sterilized, including their quantity and type.
- Biological and chemical indicator results: Record the results of all BI and CI tests, indicating whether the sterilization cycle was successful.
- Maintenance records: Document all preventative maintenance, repairs, and calibrations performed on the autoclave.
- Operator initials/signature: The operator must sign and date each entry.
Logbooks should be stored securely and kept for a period compliant with relevant regulations. Digital records, if used, should be backed up and secured according to best practices. Regular review of the logbooks is essential to identify trends and potential issues.
Q 19. What are the signs of a malfunctioning autoclave?
Several signs indicate a malfunctioning autoclave. These can range from subtle anomalies to obvious failures. Some key indicators include:
- Inconsistent sterilization results: Repeated failures of biological indicators suggest a problem with the autoclave’s performance.
- Unusual noises or vibrations: Unusual sounds or excessive vibration during operation could indicate mechanical issues.
- Leaks: Steam leaks are a serious safety hazard and indicate a need for immediate repair.
- Inaccurate temperature or pressure readings: Inconsistencies between the set parameters and actual readings point towards a sensor or control system malfunction.
- Delayed cycle completion: Cycles taking significantly longer than usual suggest a problem with heating, pressure, or vacuum systems.
- Error messages: The autoclave should display error messages if it detects a problem. These must be investigated.
Ignoring these signs can lead to ineffective sterilization, potential safety hazards, and regulatory non-compliance. Any suspicion of malfunction should trigger immediate investigation and, if necessary, professional servicing.
Q 20. Describe your experience with autoclave maintenance and calibration.
Throughout my career, I’ve been extensively involved in autoclave maintenance and calibration. I’ve worked with both gravity displacement and pre-vacuum autoclaves, performing routine checks, preventative maintenance, and troubleshooting issues. My responsibilities have included:
- Preventative maintenance: Regular cleaning, inspection of seals and gaskets, checking safety valves and sensors.
- Calibration: Using certified equipment, I’ve calibrated temperature and pressure sensors to ensure accuracy, documenting each step thoroughly.
- Troubleshooting: I’ve diagnosed and repaired various issues, from minor leaks to more complex problems with the control system. This frequently involved working with manufacturers’ manuals and technical support.
- Validation and testing: Conducting regular sterilization cycle validation using biological and chemical indicators to verify effectiveness.
For example, I once identified a faulty pressure sensor in a pre-vacuum autoclave leading to inconsistent sterilization. Prompt replacement prevented further compromised sterilization processes. My methodical approach, coupled with my experience in interpreting maintenance manuals and troubleshooting, allows me to keep autoclaves functioning optimally and safely.
Q 21. What is the appropriate temperature and pressure for sterilizing different materials?
The appropriate temperature and pressure for sterilizing different materials vary greatly. There’s no one-size-fits-all answer. Sterilization parameters must be carefully chosen based on the material’s properties and the desired sterility assurance level. Generally, a standard autoclave cycle employs saturated steam at 121°C (249°F) and 15 psi for 15-20 minutes. However, this isn’t suitable for all materials.
For example:
- Thermally sensitive materials: May require lower temperatures and shorter exposure times.
- Porous materials: Often require longer exposure times to ensure complete steam penetration.
- Liquids: Require specific cycles tailored to avoid boiling or splashing.
Consult the manufacturer’s instructions for specific materials, as incorrect settings can damage the items or render the sterilization process ineffective. It’s crucial to remember that exceeding recommended parameters can damage equipment and materials, while insufficient parameters can result in inadequate sterilization.
Q 22. How do you ensure that instruments are properly wrapped before autoclaving?
Proper wrapping of instruments before autoclaving is crucial for maintaining sterility. Think of it like wrapping a precious gift – you want to protect it from contamination until it’s needed. We use specifically designed medical-grade wraps, typically paper or fabric-based, to create a barrier.
- Material Selection: We choose wraps that allow for steam penetration while maintaining a robust barrier against external contaminants after sterilization. Common materials include muslin wraps, paper-plastic pouches, and specialized sterilization wraps. The choice depends on the instrument type and intended use.
- Wrapping Technique: The wrapping technique is standardized to ensure complete coverage and prevent tearing during handling. Instruments are arranged logically, typically with the handles outward for easy grasping after sterilization. The wrap is folded neatly, creating several layers of protection and allowing for efficient steam penetration. We avoid over-tightening which can compromise steam distribution.
- Indicators: Chemical indicators are incorporated into the packaging. These change color when exposed to the sterilization process, providing visual confirmation that the package has been subjected to the required temperature and steam exposure. This is a simple yet vital check that the process has worked correctly.
For example, a laparoscopic instrument set would require meticulous wrapping to ensure all components are properly protected, and the entire set remains sterile after autoclaving. Incorrect wrapping, such as leaving gaps or using unsuitable materials, can lead to instrument contamination.
Q 23. What are the potential risks associated with improper autoclave loading and unloading?
Improper autoclave loading and unloading carries significant risks, impacting both patient safety and operational efficiency. Imagine trying to cook a meal in an oven that’s overcrowded and poorly organized – you won’t get consistent results, and there’s a higher chance of accidents.
- Incomplete Sterilization: Overcrowding hinders steam penetration, resulting in incomplete sterilization. This leaves instruments contaminated and puts patients at high risk of infection.
- Equipment Damage: Incorrectly loaded instruments can damage the autoclave itself, leading to malfunctions or even serious damage. For example, instruments stacked too tightly can impede steam flow and potentially block pressure release valves.
- Burns and Injuries: Improper unloading can result in burns from hot instruments or scalding steam. Also, improperly wrapped instruments that were not fully sterilized pose a risk for contamination and subsequent infection.
- Spoilage of Sterile Goods: Improper loading, causing uneven steam distribution, may result in some items being inadequately sterilized, and others being damaged by excess heat or moisture.
In a healthcare setting, these risks can have severe consequences, potentially leading to serious infections, costly repairs, and legal implications. Strict adherence to loading and unloading protocols is non-negotiable.
Q 24. How do you deal with an emergency situation during autoclave operation?
Emergency situations during autoclave operation require immediate and decisive action. Think of it like a fire drill – knowing the procedures beforehand is vital. My training emphasizes safety protocols.
- Malfunctions: If a malfunction occurs, such as an alarm sounding, immediately turn off the autoclave and follow the manufacturer’s emergency shutdown procedure. Never attempt to troubleshoot a malfunction yourself; contact qualified technicians.
- Spills or Leaks: If a spill or leak occurs, ensure the area is safely evacuated, and contact the appropriate personnel (e.g., safety officer, biomedical engineering) to clean and decontaminate the area using appropriate protocols. Never handle spills without proper PPE.
- Burns or Injuries: If a burn or injury occurs, immediately administer first aid, notify superiors and seek appropriate medical assistance.
Regular safety training, familiarity with the equipment, and established emergency procedures are crucial to effectively handle such situations. Knowing the location of emergency shut-off switches and safety equipment is critical.
Q 25. Explain your experience with different types of autoclave packaging materials.
My experience encompasses various autoclave packaging materials, each with its own strengths and limitations. Choosing the right material depends on the instrument, the sterilization method, and the storage duration.
- Muslin Wraps: These are reusable cloth wraps offering good steam penetration. However, they require careful handling to avoid tearing and require thorough cleaning and sterilization before reuse.
- Paper-Plastic Pouches: These single-use pouches offer good barrier properties and steam penetration, and they provide a clear indication of sterilization through a color change indicator. They are convenient and reduce the risk of contamination.
- Sterilization Wraps: These specialized wraps are designed for specific applications, providing enhanced barrier properties and protection against moisture and contamination. Some are designed to be compatible with ethylene oxide sterilization.
I’ve worked with different manufacturers’ products, noting variations in material strength, steam permeability, and indicator reliability. Careful selection is essential to ensure optimal sterilization results. The selection process also considers cost-effectiveness and environmental impact.
Q 26. What are the best practices for storing sterilized items after autoclave use?
Proper storage of sterilized items is critical to maintaining sterility. Think of it like keeping food fresh after cooking – proper storage methods prevent spoilage.
- Clean and Dry Environment: Sterilized items should be stored in a clean, dry environment free from dust and debris to avoid contamination.
- Designated Storage Area: A designated storage area, ideally a dedicated room or cabinet, minimizes the risk of cross-contamination.
- Proper Shelving: Items should be stored on shelves to allow air circulation and prevent moisture accumulation.
- Rotation System: A first-in, first-out (FIFO) system ensures that older items are used before newer items, minimizing the risk of exceeding storage times.
- Storage Containers: Using appropriate containers, such as sterile storage bins or cabinets prevents airborne contamination.
Clear labeling, including date of sterilization and expiration date, is essential for proper inventory management and efficient use of resources. Regular checks of the storage area and inventory are vital to ensure optimal storage conditions and prevent spoilage.
Q 27. How do you handle spills or contamination incidents within the autoclave area?
Spills or contamination incidents within the autoclave area require immediate and appropriate response. It’s akin to cleaning up a mess in a kitchen – swift and proper action prevents further issues.
- Immediate Containment: First, contain the spill or contamination using appropriate absorbent materials. This prevents the spread of any hazardous materials.
- Personal Protective Equipment (PPE): Always wear appropriate PPE, including gloves, gowns, eye protection, and masks, depending on the nature of the spill.
- Decontamination: Follow established decontamination protocols using approved disinfectants or sterilants. These protocols vary depending on the nature of the spill (e.g., blood, chemical spills).
- Waste Disposal: Dispose of contaminated materials according to appropriate guidelines and regulations.
- Documentation: Thoroughly document the incident, including the type of spill, the actions taken, and any injuries sustained.
Regular training in spill response and decontamination procedures is essential to handle such incidents safely and effectively. Understanding the safety data sheets (SDS) for all chemicals used in the autoclave area is crucial in formulating a safe and effective response.
Key Topics to Learn for Autoclave Loading and Unloading Interview
- Understanding Autoclave Operation: Familiarize yourself with the different types of autoclaves, their operating principles (pressure, temperature, time cycles), and safety mechanisms.
- Sterilization Principles: Grasp the fundamental concepts of sterilization, including the factors influencing sterilization effectiveness (e.g., temperature, pressure, exposure time, load configuration).
- Proper Loading Techniques: Learn best practices for loading autoclaves efficiently and effectively, ensuring proper air removal and even steam distribution. This includes understanding the importance of load configuration and avoiding overloading.
- Packaging and Wrapping Materials: Know the different types of packaging materials used for sterilization, their properties, and how to select appropriate materials for different applications. Understand the implications of incorrect packaging on sterilization efficacy.
- Unloading Procedures and Aseptic Techniques: Master safe and aseptic unloading techniques to prevent contamination of sterilized items. Understand the importance of maintaining a sterile field during the unloading process.
- Quality Control and Documentation: Learn how to document sterilization cycles accurately and completely, including monitoring parameters like temperature, pressure, and time. Understand the importance of quality control measures to ensure the efficacy of the sterilization process.
- Troubleshooting Common Issues: Develop problem-solving skills related to autoclave operation, including identifying and resolving common issues like air entrapment, inadequate sterilization, and equipment malfunctions.
- Safety Regulations and Procedures: Familiarize yourself with relevant safety regulations and procedures for working with autoclaves, including personal protective equipment (PPE) and emergency response protocols.
- Validation and Qualification: Understand the importance of autoclave validation and qualification processes to ensure consistent and reliable sterilization.
Next Steps
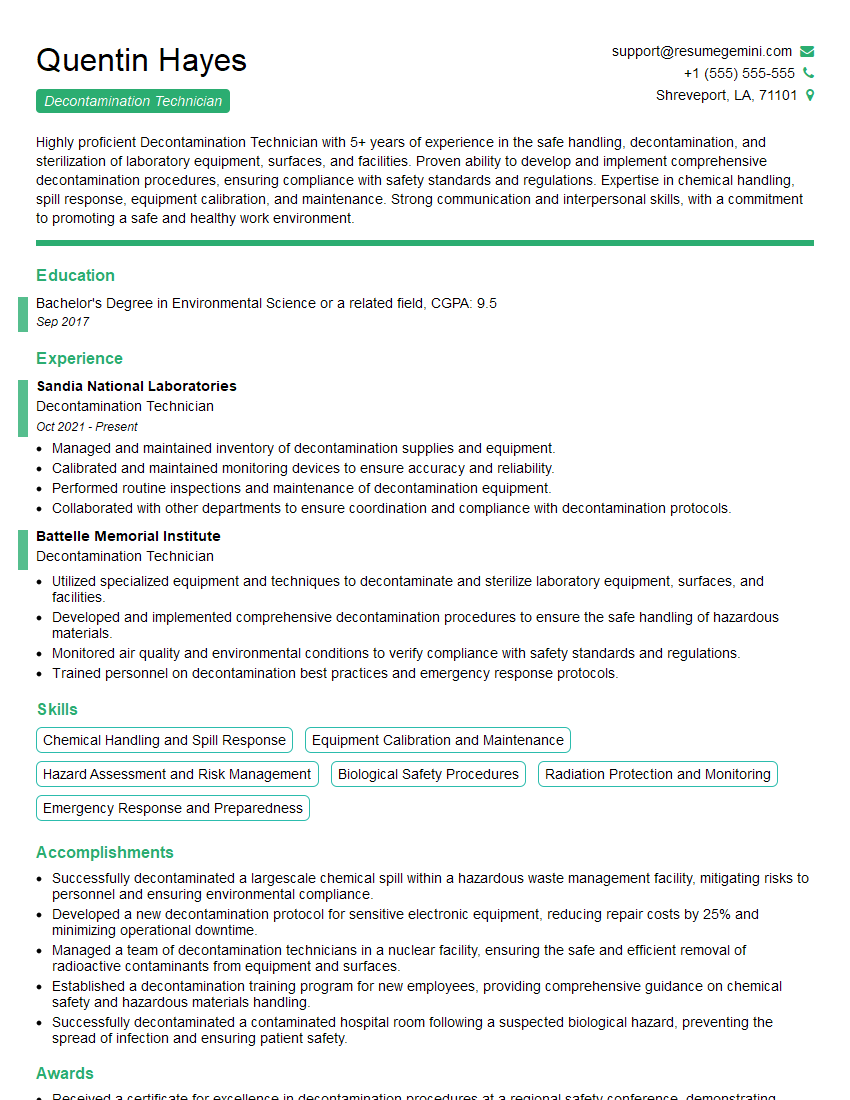
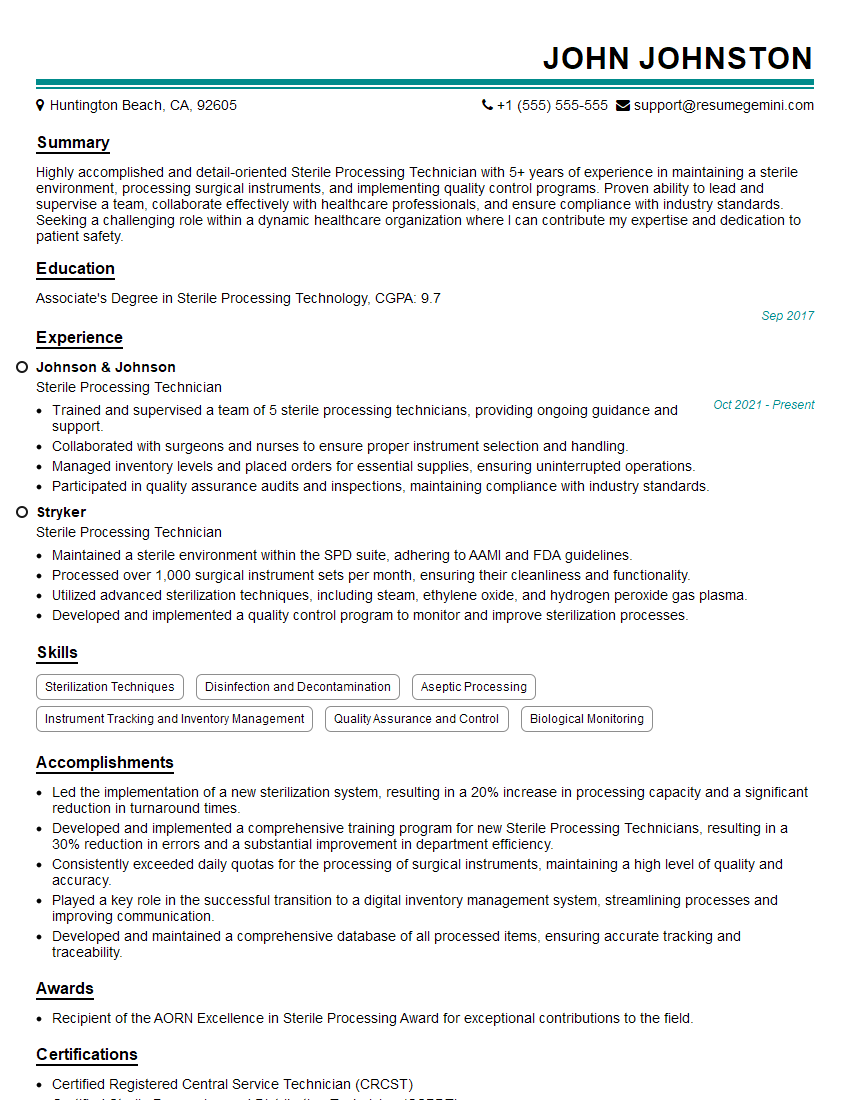
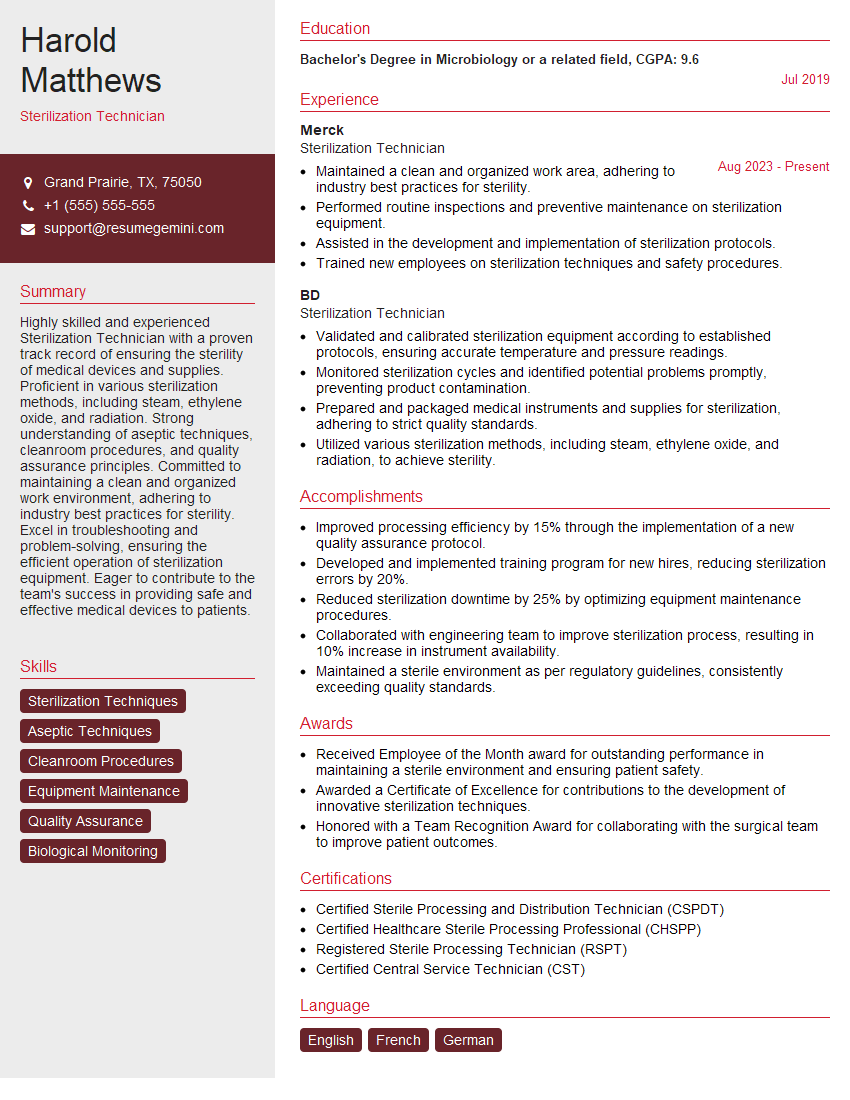
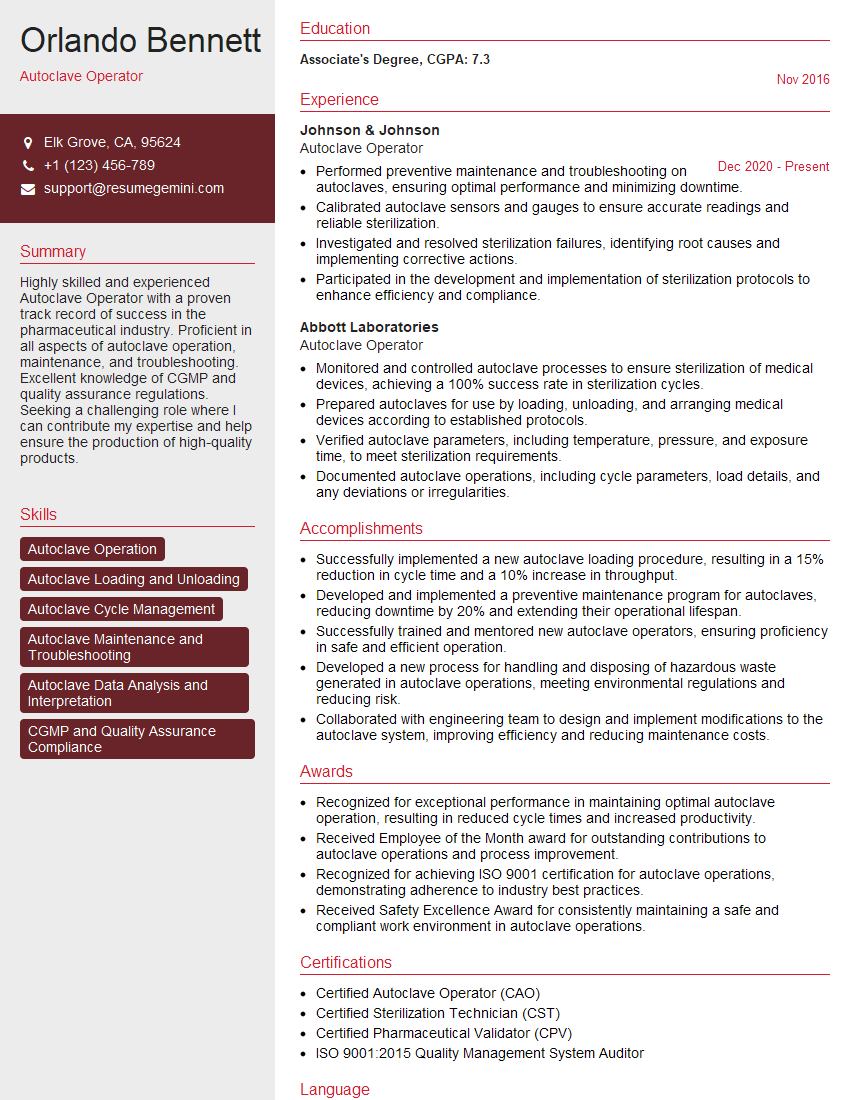
Mastering autoclave loading and unloading is crucial for career advancement in many industries, including healthcare, pharmaceuticals, and research. A strong understanding of these procedures demonstrates essential skills in sterile processing and quality control, opening doors to various opportunities and higher responsibilities. To enhance your job prospects, create an ATS-friendly resume that highlights your skills and experience effectively. ResumeGemini is a trusted resource that can help you build a professional and impactful resume. We provide examples of resumes tailored to Autoclave Loading and Unloading positions to guide you in crafting your own compelling application materials.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Live Rent Free!
https://bit.ly/LiveRentFREE
Interesting Article, I liked the depth of knowledge you’ve shared.
Helpful, thanks for sharing.
Hi, I represent a social media marketing agency and liked your blog
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?