Feeling uncertain about what to expect in your upcoming interview? We’ve got you covered! This blog highlights the most important Comprehensive Eye Exams interview questions and provides actionable advice to help you stand out as the ideal candidate. Let’s pave the way for your success.
Questions Asked in Comprehensive Eye Exams Interview
Q 1. Explain the procedure for performing a visual acuity test using a Snellen chart.
The Snellen chart is the most common tool for assessing visual acuity, which is the clarity of vision. The test measures how well you can see at various distances. It’s a simple yet crucial part of a comprehensive eye exam.
Procedure:
- Patient Positioning: The patient sits 20 feet away from the chart. This standardized distance is crucial for accurate interpretation.
- Chart Presentation: The patient covers one eye at a time while looking at the chart. They are instructed to read the smallest line of letters they can clearly discern.
- Recording Results: We record the smallest line the patient reads correctly. For example, ’20/20′ means the patient can see at 20 feet what a person with normal vision can see at 20 feet. A score of ’20/40′ means the patient can see at 20 feet what a person with normal vision can see at 40 feet, indicating some visual impairment.
- Repetition: The procedure is repeated for the other eye.
Practical Application: Identifying visual acuity issues early through this simple test allows for timely intervention, preventing further complications and improving quality of life. For instance, a child with 20/40 vision might need glasses to improve their academic performance.
Q 2. Describe the different types of refractive errors and how they are corrected.
Refractive errors occur when the shape of your eye prevents light from focusing correctly on the retina, leading to blurry vision. Common types include:
- Myopia (Nearsightedness): The eye is longer than normal, causing distant objects to appear blurry. Corrected with concave (minus) lenses.
- Hyperopia (Farsightedness): The eye is shorter than normal, making nearby objects blurry. Corrected with convex (plus) lenses.
- Astigmatism: The cornea (the eye’s front surface) is irregularly shaped, resulting in blurred vision at all distances. Corrected with cylindrical lenses or toric contact lenses.
Correction Methods:
- Eyeglasses: Lenses positioned in front of the eye refract light to correct the refractive error.
- Contact Lenses: Lenses placed directly on the eye’s surface offer a wider field of vision and are cosmetically appealing to many. Different types, like soft, rigid gas permeable (RGP), and toric lenses, address various needs and refractive errors.
- Refractive Surgery (e.g., LASIK): Reshapes the cornea to correct the refractive error permanently, eliminating the need for glasses or contacts.
Example: A patient with myopia of -2.00 diopters (a unit of refractive power) would require concave lenses with a power of -2.00 D to see clearly at a distance.
Q 3. How do you assess and manage glaucoma during a comprehensive eye exam?
Glaucoma is a group of eye diseases that damage the optic nerve, often due to increased intraocular pressure (IOP). Early detection and management are crucial to preventing vision loss.
Assessment:
- IOP Measurement (Tonometry): We use instruments like an applanation tonometer to measure IOP. Elevated IOP is a risk factor for glaucoma, but not everyone with high IOP develops the disease.
- Optic Nerve Examination (Ophthalmoscopy): A detailed examination of the optic nerve head, looking for cupping (a characteristic change in the appearance of the optic nerve associated with glaucoma).
- Visual Field Testing (Perimetry): This assesses the extent of peripheral vision. Glaucoma often causes peripheral vision loss before central vision is affected.
Management:
- Medications: Eye drops are often the first line of defense, lowering IOP and slowing disease progression.
- Laser Treatment (e.g., Laser Peripheral Iridotomy): May be used to improve fluid drainage in the eye, lowering IOP.
- Surgery (e.g., Trabeculectomy): Surgical procedures can create a new drainage pathway to reduce IOP when medication and laser treatment are insufficient.
Example: A patient with elevated IOP and characteristic optic nerve changes might be diagnosed with glaucoma and prescribed eye drops to manage their IOP and slow disease progression.
Q 4. What are the key steps in performing a dilated fundus examination?
Dilated fundus examination allows for a detailed view of the retina, optic nerve, macula, and blood vessels at the back of the eye. It is a critical part of a comprehensive eye exam, allowing for the detection of various eye conditions.
Steps:
- Pupil Dilation: Eye drops are used to dilate the pupils, widening them to allow better visualization of the fundus.
- Patient Positioning: The patient is positioned comfortably, usually lying down.
- Indirect Ophthalmoscopy: Using an indirect ophthalmoscope, we view the fundus through a lens system. This provides a wider field of view and allows us to assess the overall health of the retina and optic nerve.
- Direct Ophthalmoscopy: We may also use a direct ophthalmoscope for a closer, more detailed examination of specific areas.
- Documentation: We meticulously document our findings, including descriptions of the optic nerve, blood vessels, macula, and any abnormalities detected.
Practical Application: This detailed exam helps detect conditions such as diabetic retinopathy, macular degeneration, glaucoma, and other retinal diseases in their early stages, enabling timely intervention and preservation of vision.
Q 5. How do you detect and manage diabetic retinopathy during a comprehensive eye exam?
Diabetic retinopathy is a complication of diabetes that affects the blood vessels in the retina. Early detection and management are essential to prevent vision loss.
Detection:
- Dilated Fundus Examination: A detailed examination of the retina, allowing for the visualization of microaneurysms, hemorrhages, exudates, and neovascularization—characteristic signs of diabetic retinopathy.
- Optical Coherence Tomography (OCT): A non-invasive imaging technique provides detailed cross-sectional images of the retina, helping to assess the severity of retinopathy and monitor treatment response.
- Fluorescein Angiography: A dye is injected into a vein, and images are taken to visualize the blood vessels in the retina. This helps to identify areas of leakage or abnormal blood vessel growth.
Management:
- Blood Sugar Control: Strict control of blood glucose levels is crucial to slow the progression of diabetic retinopathy.
- Anti-VEGF Injections: Medications that block vascular endothelial growth factor (VEGF), reducing abnormal blood vessel growth.
- Laser Photocoagulation: Laser treatment to seal off leaking blood vessels and reduce the risk of vision loss.
Example: A patient with diabetes undergoing a dilated fundus exam might be diagnosed with early diabetic retinopathy and recommended to maintain strict blood sugar control and undergo regular monitoring to prevent disease progression.
Q 6. Describe your experience with automated perimetry testing.
Automated perimetry, also known as automated visual field testing, is a crucial diagnostic tool in ophthalmology. It objectively measures the extent and sensitivity of a patient’s peripheral vision.
Experience: I have extensive experience using various automated perimeter devices. These tests are particularly useful in diagnosing and monitoring conditions such as glaucoma, where peripheral vision loss is an early and significant sign. The machines present stimuli (flashes of light) at various locations within the visual field, and the patient responds by pressing a button when they detect the stimuli. The results are mapped graphically, providing a detailed picture of the patient’s visual field.
Benefits of Automated Perimetry:
- Objectivity: It provides a quantitative and objective measurement of visual field defects, minimizing variability compared to manual perimetry.
- Efficiency: It’s faster and more efficient than manual perimetry.
- Reproducibility: Allows for repeated testing and accurate monitoring of disease progression or treatment response.
Example: In a patient suspected of glaucoma, automated perimetry can pinpoint areas of visual field loss, even before noticeable changes are apparent on a standard eye exam. This early detection is critical for effective glaucoma management.
Q 7. Explain the process of fitting contact lenses, including considerations for different lens types and patient needs.
Contact lens fitting is a specialized procedure requiring precise measurements and consideration of individual patient needs.
Process:
- Initial Consultation and Examination: A thorough eye examination is performed, including visual acuity testing, refractive error assessment, and evaluation of corneal topography (shape of the cornea).
- Measurements: Precise measurements of the cornea’s curvature, diameter, and thickness are taken using instruments such as a keratometer and sometimes a corneal topographer.
- Lens Selection: Based on the measurements and the patient’s needs and preferences, we select the appropriate lens type, material, and power.
- Trial Lens Fitting: Trial lenses are inserted, and the patient’s comfort, visual acuity, and the fit of the lenses are evaluated. Adjustments might be made to the lens parameters.
- Instruction and Follow-up: Patients are instructed on proper lens insertion, removal, care, and hygiene. Follow-up appointments are scheduled to monitor lens fit and comfort.
Considerations for Different Lens Types:
- Soft Contact Lenses: Generally comfortable and easy to handle, suitable for most refractive errors. However, they may not be ideal for high astigmatism or certain corneal conditions.
- Rigid Gas Permeable (RGP) Lenses: Provide sharper vision and better oxygen permeability than soft lenses, particularly beneficial for patients with astigmatism or corneal irregularities. However, they require a longer adjustment period.
- Toric Lenses: Designed to correct astigmatism.
- Multifocal Lenses: Correct both near and far vision.
Patient Needs: Factors like lifestyle (e.g., sports), occupation, and allergies are considered when selecting lens type. A patient who engages in water sports might prefer daily disposable lenses to avoid infection risk.
Q 8. How do you counsel patients on the importance of regular eye exams and preventative care?
Counseling patients about regular eye exams is crucial for preventative care. I begin by explaining that just like regular check-ups for your heart or other organs, eye exams are essential for detecting problems early, often before you notice any symptoms. I emphasize that early detection significantly improves treatment outcomes and can prevent vision loss. I use analogies to make it relatable, such as comparing an eye exam to a car tune-up – preventative maintenance keeps everything running smoothly. I tailor my approach to the individual’s age and risk factors. For example, I might emphasize the importance of glaucoma screening for patients over 60 or diabetic retinopathy screening for those with diabetes. I explain the different components of a comprehensive exam, including visual acuity testing, assessing eye pressure, and examining the retina, clarifying how each part contributes to a holistic understanding of their eye health. I also provide clear information about the frequency of recommended exams, typically annually for adults over 40 and potentially more frequently depending on individual needs and risk factors.
Q 9. Explain the difference between myopia, hyperopia, and astigmatism.
Myopia, hyperopia, and astigmatism are all refractive errors, meaning they result from how light focuses on the retina. Think of it like this: your eye is a camera, and the light needs to focus perfectly on the film (retina) to get a clear picture. In myopia (nearsightedness), the light focuses in front of the retina, resulting in blurry distance vision. Imagine the camera lens is too strong, pushing the focus point forward. Hyperopia (farsightedness) is the opposite; the light focuses behind the retina, causing blurry near vision. This is like the camera lens being too weak, unable to bring near objects into sharp focus. Astigmatism occurs when the cornea (the clear front part of the eye) is irregularly shaped, preventing the light from focusing properly on any part of the retina, leading to blurry vision at all distances. It’s like the camera lens having imperfections, distorting the image. Each condition can be corrected with eyeglasses, contact lenses, or refractive surgery.
Q 10. What are the signs and symptoms of age-related macular degeneration (AMD)?
Age-related macular degeneration (AMD) is a progressive eye disease affecting the macula, the central part of the retina responsible for sharp, central vision. Early signs are often subtle and might include blurred vision, difficulty seeing fine details (like reading), and a distortion of straight lines appearing wavy. As AMD progresses, central vision loss worsens. Patients may describe a dark or blurry spot in the center of their vision. Advanced AMD can lead to significant vision impairment, making everyday tasks like reading and driving challenging. There are two main types: dry AMD, which is more common but progresses slower, and wet AMD, characterized by abnormal blood vessel growth that can rapidly lead to vision loss. Regular eye exams, particularly after age 50, are crucial for early detection and management.
Q 11. How do you differentiate between cataracts and other eye conditions?
Cataracts and other eye conditions can share some similar symptoms like blurry vision, but there are key differences. Cataracts are a clouding of the eye’s natural lens, gradually impairing vision. The vision often gets progressively blurrier, like looking through a frosted window, and can be associated with glare and halos around lights. Other conditions, such as macular degeneration, glaucoma, and diabetic retinopathy, affect different parts of the eye and present with distinct symptoms. For example, glaucoma often causes peripheral vision loss first, while diabetic retinopathy can lead to blurry vision and floaters. A comprehensive eye exam, including a dilated pupil examination, allows for a thorough assessment of the eye’s structures and helps differentiate between these conditions. Often, ophthalmoscopy and imaging tests (like OCT) are crucial for accurate diagnosis.
Q 12. Describe your experience with interpreting ophthalmic imaging (e.g., OCT, fundus photography).
I have extensive experience interpreting ophthalmic imaging, including optical coherence tomography (OCT) and fundus photography. OCT provides high-resolution cross-sectional images of the retina, allowing for detailed assessment of retinal thickness, macular edema, and the health of the optic nerve. I use OCT scans to diagnose and monitor conditions like macular degeneration, glaucoma, and diabetic retinopathy. Fundus photography captures detailed images of the retina and optic nerve, enabling detection of abnormalities such as hemorrhages, exudates, and drusen (characteristic deposits in AMD). My interpretation skills involve not only recognizing specific features on these images but also correlating them with the patient’s clinical presentation and other diagnostic tests. For example, seeing thickened retinal layers on an OCT scan and corresponding swelling during a clinical exam helps confirm macular edema. The integration of imaging data with clinical findings significantly enhances diagnostic accuracy and treatment planning.
Q 13. How do you assess and manage dry eye disease?
Dry eye disease is a common condition causing discomfort and vision problems due to insufficient lubrication and tear film quality. Assessment involves a detailed history, evaluating symptoms like dryness, burning, itching, foreign body sensation, and fluctuating vision. I perform a comprehensive examination, including tear film evaluation (measuring tear production and assessing tear film stability), assessing the meibomian glands (responsible for oil secretion in the tear film), and evaluating the ocular surface for signs of inflammation. Management starts with conservative measures like artificial tears, lid hygiene (warm compresses and lid scrubs to remove debris from the eyelids), and avoiding environmental irritants such as smoke and wind. For more severe cases, I might recommend punctal plugs (to reduce tear drainage) or prescription eye drops to reduce inflammation. In some cases, in-office procedures like meibomian gland expression are beneficial. Regular follow-up visits are crucial to monitor the disease’s progression and adjust treatment as needed.
Q 14. What are the common causes of eye infections, and how do you manage them?
Common causes of eye infections include bacterial, viral, and fungal organisms. Bacterial conjunctivitis (pinkeye), characterized by redness, discharge, and itching, is often treated with antibiotic eye drops. Viral conjunctivitis, frequently associated with upper respiratory infections, is typically self-limiting, requiring symptomatic treatment with artificial tears and cool compresses. Fungal infections are less common but can be serious and require antifungal medication. Herpes simplex virus can cause keratitis, affecting the cornea, potentially leading to vision impairment if not treated promptly with antiviral medication. Diagnosis relies on careful history taking, clinical examination, and sometimes cultures or specialized tests to identify the causative organism. Treatment is tailored to the specific infection, emphasizing proper hygiene to prevent spread. Patients are advised to avoid sharing towels, wash hands frequently, and use prescribed medication as directed. I always emphasize the importance of seeking prompt medical attention for any eye infection, especially if vision is affected or there are signs of severe inflammation.
Q 15. How do you perform a proper external eye exam?
A proper external eye exam begins with a thorough assessment of the patient’s overall appearance, followed by a systematic evaluation of the eyelids, surrounding tissues, and the eyeball itself. Think of it like a visual ‘head-to-toe’ examination, specifically for the eye region.
Assessment of the eyelids: We look for ptosis (drooping eyelids), edema (swelling), lesions (abnormal growths), or any signs of inflammation such as redness or crusting. For instance, a patient presenting with significantly droopy eyelids might point towards a neurological condition.
Examination of the surrounding tissues: This includes checking the conjunctiva (the membrane lining the inside of the eyelids and covering the sclera, the white part of the eye), the sclera for any discoloration (jaundice can manifest as yellowing), and the lacrimal apparatus (tear ducts) for signs of blockage or inflammation. Noticeable redness in the conjunctiva could indicate an infection like conjunctivitis.
Inspection of the eyeball: We assess the position of the eyes (looking for strabismus or misalignment), the cornea (for clarity and irregularities), and the pupil (size, shape, and reactivity to light). An unevenly sized pupil, for example, could signal a neurological problem.
Palpation: Gently palpating the orbit (the bony socket) helps to detect any underlying masses or abnormalities. This step is crucial in assessing the extent of any trauma.
Throughout the exam, I meticulously document all observations, including the use of standardized terminology and precise measurements, creating a comprehensive record for accurate diagnosis and treatment planning. This methodical approach ensures no detail is missed, allowing for a thorough understanding of the patient’s eye health.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. What are the potential risks and complications of contact lens wear?
Contact lens wear, while offering excellent vision correction, carries potential risks and complications. These range from minor inconveniences to serious sight-threatening conditions.
Infections: One of the most serious risks is microbial keratitis, an infection of the cornea. This can lead to vision impairment or even blindness if left untreated. Proper hygiene and lens care are crucial to prevent this.
Allergic reactions: Contact lens solutions or the lens material itself can trigger allergic reactions, resulting in redness, itching, and discomfort. Switching to a hypoallergenic solution or lens type might be necessary.
Corneal damage: Improper lens fit, extended wear, or inadequate hygiene can cause corneal abrasions, ulcers, or scarring. Regular eye exams and appropriate lens fitting are vital to avoid this.
Giant papillary conjunctivitis (GPC): This condition, characterized by the formation of large papillae on the conjunctiva, is often associated with contact lens wear, especially extended-wear lenses. Symptoms include itching, redness, and blurry vision. Switching lens materials or wearing schedules can help.
Dry eye disease: Contact lenses can exacerbate dry eye symptoms by interfering with the tear film. Patients with pre-existing dry eye are usually advised to use alternative correction methods.
Educating patients about proper hygiene, lens care, and the importance of regular follow-up appointments is a critical aspect of responsible contact lens prescribing and management. The risks should always be carefully weighed against the benefits for each patient.
Q 17. Describe your experience with pediatric eye exams.
Pediatric eye exams require a unique approach because children cannot always articulate their visual experiences. It’s a combination of careful observation, engaging techniques, and specialized tools. I use age-appropriate strategies to gain cooperation and obtain accurate assessment.
Creating a comfortable and playful environment: I use toys, games, and positive reinforcement to make the experience less stressful for the child. Building rapport is key.
Employing specialized techniques: For very young children, I might rely on observation of their eye movements and reactions to stimuli, rather than verbal responses. We also use retinoscopy, a technique to objectively measure refractive error.
Parental involvement: Parents are crucial in providing relevant history and offering support and reassurance to the child during the exam. Their observations about the child’s vision are valuable.
Early detection of amblyopia and strabismus: Early identification of these conditions in young children is vital for effective treatment. My approach emphasizes thorough screening and appropriate referrals when needed.
I’ve had many rewarding experiences helping children achieve optimal vision. One example includes detecting amblyopia (lazy eye) in a young patient and guiding them through a successful treatment plan, resulting in significantly improved vision. Early intervention is paramount in pediatric eye care.
Q 18. How do you handle patients with visual field defects?
Patients with visual field defects present unique challenges, necessitating a comprehensive approach to understand the extent of the loss and the underlying cause. A thorough history, including any neurological symptoms, is crucial.
Visual field testing: This is the cornerstone of assessing visual field defects. I use automated perimetry, a sophisticated test that maps out the extent of the visual field loss. Manual perimetry may be used in certain cases.
Identifying the cause: The location and nature of the defect help determine the underlying cause, which could be anything from glaucoma, stroke, brain tumors, or other neurological conditions.
Referral and management: Depending on the cause, I may refer patients to neurologists, ophthalmologists specializing in glaucoma or other conditions, or other specialists as needed. This often involves collaboration with a multidisciplinary team.
Adaptive strategies and rehabilitation: I work with the patient to develop strategies to compensate for visual field defects. This might involve vision therapy techniques, low vision aids, or adaptive strategies for daily living.
For instance, a patient with a right homonymous hemianopsia (loss of vision in the right half of both visual fields) would need careful instruction on scanning techniques to compensate for the loss of peripheral vision on the right side. The key is to help patients maximize their remaining vision.
Q 19. Explain the importance of pupillary responses in assessing neurological function.
Pupillary responses—the changes in pupil size in response to light and accommodation (focusing)—provide invaluable insights into neurological function. The pupillary light reflex is an essential test to evaluate the integrity of the pathways connecting the eye to the brain.
Direct and consensual light reflex: Shining a light into one eye should cause constriction (narrowing) of that pupil (direct reflex) and the other pupil (consensual reflex). The absence or asymmetry of these reflexes suggests damage to the oculomotor nerve or pathways in the brainstem.
Accommodation reflex: As the patient focuses on a near object, their pupils should constrict and converge (move inwards). Disruptions in this reflex can indicate damage to the parasympathetic nervous system.
Significance in neurological assessment: Pupillary abnormalities can be a sign of a variety of neurological conditions, including stroke, trauma, tumors, and drug intoxication. For example, a unilateral dilated pupil that is nonreactive to light (blown pupil) could indicate a serious neurological emergency such as a brain herniation.
Careful assessment of pupillary responses is a quick and effective method for detecting potential neurological compromise. Any abnormalities necessitate a more thorough neurological evaluation.
Q 20. Describe your experience with documenting findings from a comprehensive eye exam.
Meticulous documentation is crucial in ophthalmology. It ensures clear communication among healthcare providers, facilitates effective patient care, and provides a comprehensive record for future reference. My documentation follows a consistent format to ensure completeness and clarity.
Patient demographics and history: This includes age, medical history, medication history, and relevant family history of eye conditions.
Visual acuity: Recorded using standardized notation (e.g., 20/20, 20/40).
External examination findings: Detailed description of the eyelids, conjunctiva, sclera, cornea, and iris.
Intraocular pressure (IOP): If measured, IOP is recorded in mmHg.
Refraction: The refractive error is meticulously documented, including the spherical, cylindrical, and axis components.
Dilated fundus examination: A comprehensive description of the optic nerve, retina, blood vessels, and macula, including any pathological findings.
Visual field testing results: Summarized and interpreted.
Diagnosis, treatment plan, and prognosis: Clearly stated and justified.
I utilize an electronic health record (EHR) system, allowing for efficient and organized storage of patient information. I regularly review and update the record as needed to ensure its accuracy and relevance.
Q 21. What is your approach to managing patients with ocular trauma?
Managing patients with ocular trauma requires a swift and methodical approach, prioritizing immediate assessment and treatment to minimize long-term complications. Every second counts.
Initial assessment: A rapid assessment of visual acuity, level of consciousness, and the extent of the injury is paramount. This often involves determining whether the injury is open-globe or closed-globe.
Immediate steps: In the case of an open-globe injury (a perforation of the eyeball), the priority is to protect the eye from further damage. This usually involves covering the eye with a shield or cup, minimizing eye movement, and promptly referring the patient to a specialist.
Imaging: Imaging studies such as CT scans or ultrasound may be necessary to assess the extent of the damage.
Surgical intervention: In many cases, surgical repair is needed to restore the integrity of the eye and prevent vision loss. This often requires immediate consultation with an ophthalmologist specialized in ophthalmic trauma.
Post-operative care: This involves meticulous monitoring and management of pain, infection, and inflammation. Long-term follow-up is essential to assess visual recovery and manage any complications.
I’ve managed numerous cases of ocular trauma, from minor corneal abrasions to severe open-globe injuries. A calm and decisive approach is crucial in these situations to ensure the best possible outcome for the patient. Collaboration with other specialists is often key to success in these often urgent situations.
Q 22. How do you communicate complex medical information to patients effectively?
Communicating complex medical information effectively requires a multi-pronged approach. I prioritize using plain language, avoiding jargon whenever possible. For instance, instead of saying ‘your visual acuity is 20/40,’ I’d explain, ‘This means you need to be twice as close to an object to see it as clearly as someone with perfect vision.’ I also use visual aids like diagrams or even simple drawings to illustrate concepts. Active listening is key; I ensure the patient understands by asking them to explain the information back in their own words. Finally, I tailor my communication style to the individual patient’s understanding and learning style, recognizing that some patients may need more time or simpler explanations than others. For example, for a visually impaired patient, I’d prioritize a clear and concise verbal explanation rather than relying heavily on written materials.
Q 23. What are the ethical considerations involved in diagnosing and managing eye conditions?
Ethical considerations in diagnosing and managing eye conditions are paramount. Patient autonomy is central – informed consent is crucial before any procedure or treatment. This means patients must understand their condition, treatment options, potential benefits, and risks in terms they can grasp. Confidentiality is also critical; all patient information must be kept private and protected. Maintaining professional boundaries is essential to avoid conflicts of interest. For example, I would never recommend a specific brand of contact lenses unless it’s the most appropriate choice for the patient based on their needs, avoiding any financial incentives. Furthermore, accurate diagnosis and honest communication are vital, even if delivering difficult news. I always strive to empower patients by providing them with the knowledge and resources they need to make informed decisions about their care. In situations with ethical dilemmas, I’d consult with colleagues or ethical review boards to ensure I’m making the best decisions for the patient.
Q 24. How do you stay up-to-date with advancements in ophthalmology and optometry?
Staying current in ophthalmology and optometry is an ongoing process. I actively participate in continuing medical education (CME) courses and workshops, focusing on the latest diagnostic techniques and treatment protocols. I regularly read peer-reviewed journals like the American Journal of Ophthalmology and Ophthalmology, as well as reputable online resources. Attending professional conferences and meetings, such as those held by the American Academy of Ophthalmology, allows for networking with colleagues and learning about the latest breakthroughs. I also participate in online professional communities and discussion forums to engage with other eye care professionals and stay updated on current research and best practices. Keeping abreast of new technologies is also important; for example, I’ve recently completed training on the use of optical coherence tomography (OCT) and its applications in diagnosing various retinal conditions.
Q 25. Describe your experience with using different types of ophthalmic instruments.
My experience with ophthalmic instruments is extensive. I’m proficient in using autorefractors for objective refractive error assessment, phoropters for subjective refraction, and various types of ophthalmoscopes for fundoscopy, including direct and indirect ophthalmoscopes. I’m also skilled in using slit-lamp biomicroscopes for detailed examination of the anterior segment of the eye, including the cornea, iris, and lens. I routinely use tonometers for measuring intraocular pressure (IOP) to screen for glaucoma. My expertise extends to the use of advanced imaging modalities such as OCT for high-resolution retinal imaging and visual field analyzers for assessing peripheral vision. I’m comfortable operating and interpreting data from all these instruments, ensuring accurate diagnosis and personalized treatment plans. For example, using OCT has allowed me to detect early signs of macular degeneration in several patients, leading to timely interventions.
Q 26. How do you handle challenging or emotional patient interactions?
Handling challenging or emotional patient interactions requires empathy, patience, and strong communication skills. I approach such situations by first actively listening to the patient’s concerns without interrupting. I validate their feelings and attempt to understand their perspective. For instance, a patient receiving a diagnosis of a serious eye condition might experience fear or anxiety. In such cases, I provide a supportive environment, answer their questions patiently, and offer reassurance. I explain their condition clearly and concisely, and offer available support systems, including referrals to counselors or support groups if necessary. My goal is not just to treat their medical condition but to also address their emotional needs and build trust. Documenting these interactions thoroughly in the patient’s medical record is also crucial.
Q 27. What are your strengths and weaknesses as an eye care professional?
My strengths as an eye care professional include my strong diagnostic skills, my ability to build rapport with patients, and my dedication to providing compassionate care. I’m highly organized and efficient in managing my workload. My commitment to continuing education ensures I remain at the forefront of advancements in the field. A weakness I’ve identified is occasionally struggling to balance patient care with administrative tasks, though I’m actively working on improving my time management skills by implementing better scheduling and prioritization techniques. I’m also striving to improve my delegation skills to more effectively manage my responsibilities. Continuous self-assessment and seeking feedback from colleagues helps me identify areas for improvement and ensures I deliver the highest quality of care.
Key Topics to Learn for Comprehensive Eye Exams Interview
- Visual Acuity Assessment: Understanding different methods (Snellen chart, pinhole test), interpreting results, and recognizing common refractive errors (myopia, hyperopia, astigmatism).
- Refraction: Mastering subjective and objective refraction techniques, understanding cycloplegic refraction, and its application in various patient populations (pediatrics, adults).
- Binocular Vision Testing: Familiarize yourself with tests like cover test, phorias and tropias, stereopsis assessment (e.g., using random dot stereograms), and the significance of binocular vision in daily life.
- Ocular Motility and Extraocular Muscle Function: Understanding the anatomy and function of extraocular muscles, performing and interpreting diagnostic tests for strabismus and other motility disorders.
- Pupil Examination: Learn to assess pupil size, reactivity to light and accommodation, and recognizing abnormal pupil responses indicative of neurological conditions.
- External Eye Examination: Mastering the techniques for examining the eyelids, conjunctiva, sclera, cornea, and anterior chamber. Recognizing common pathologies and understanding their significance.
- Intraocular Pressure Measurement (Tonometry): Understanding the different methods (Applanation tonometry, non-contact tonometry), interpreting results, and recognizing the implications of elevated or lowered IOP.
- Ophthalmoscopy: Developing proficiency in direct and indirect ophthalmoscopy, visualizing the optic disc, retina, macula, and blood vessels, recognizing common retinal pathologies.
- Patient History Taking and Communication: Mastering effective communication skills to gather relevant patient information, accurately document findings, and build rapport.
- Interpreting Diagnostic Results: Understanding and interpreting various diagnostic tests and imaging results (e.g., visual field testing, OCT). Analyzing data to formulate a comprehensive diagnosis.
Next Steps
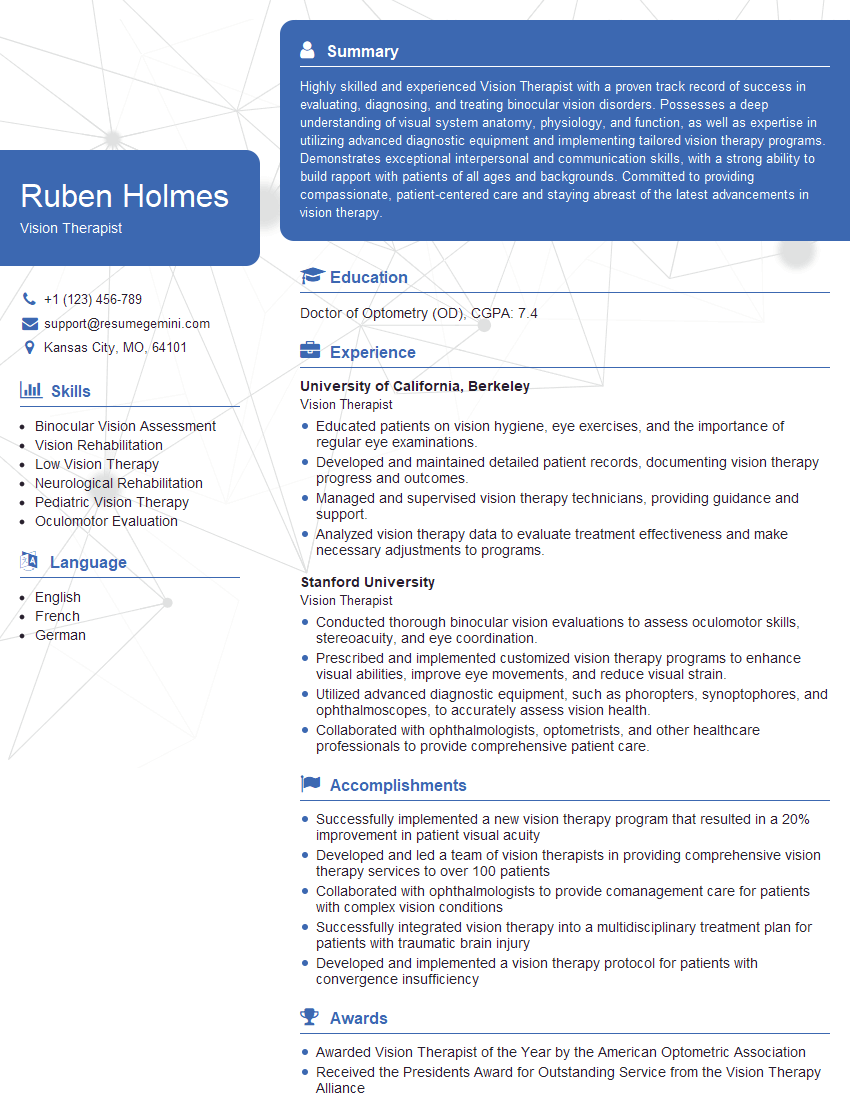
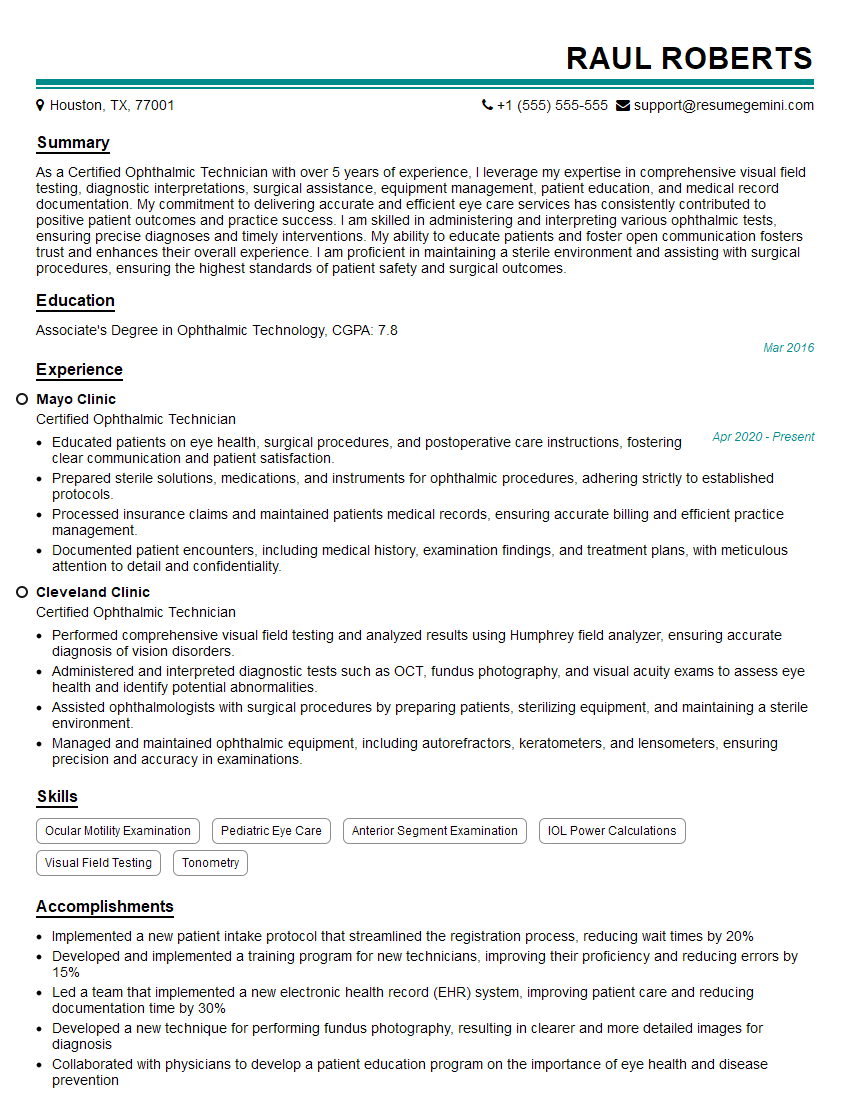
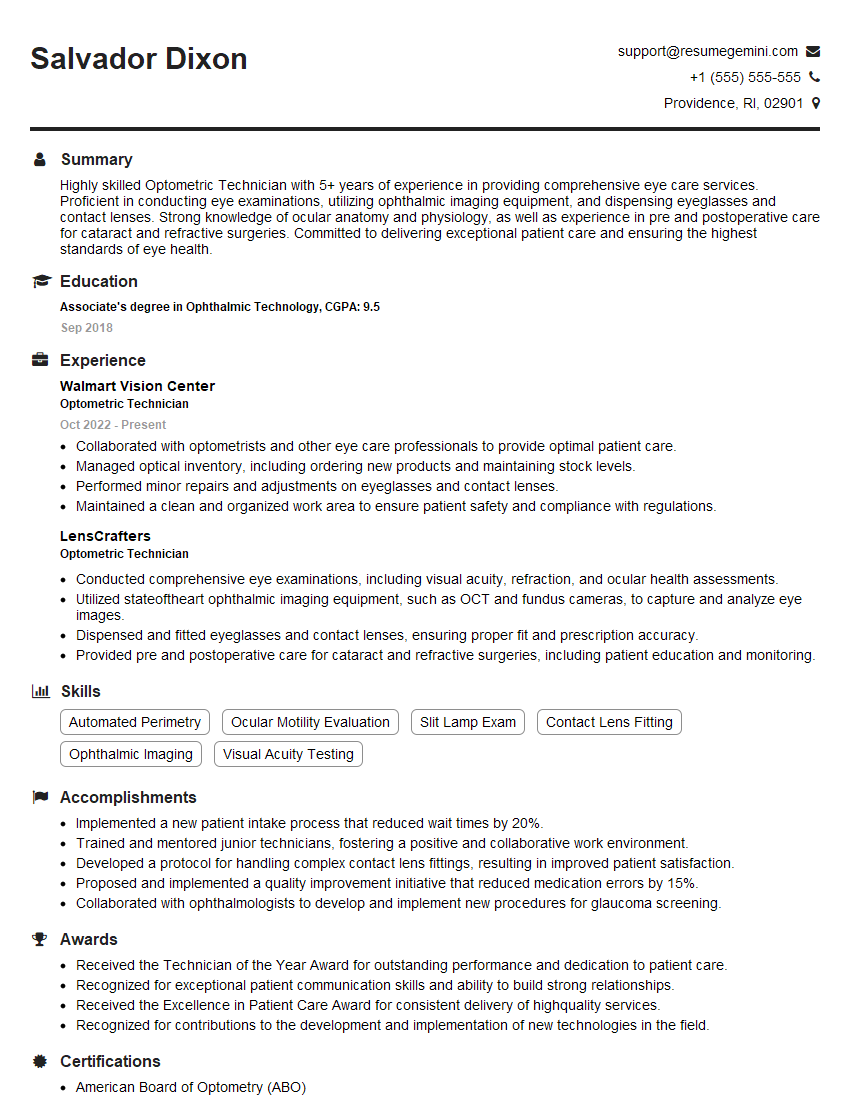
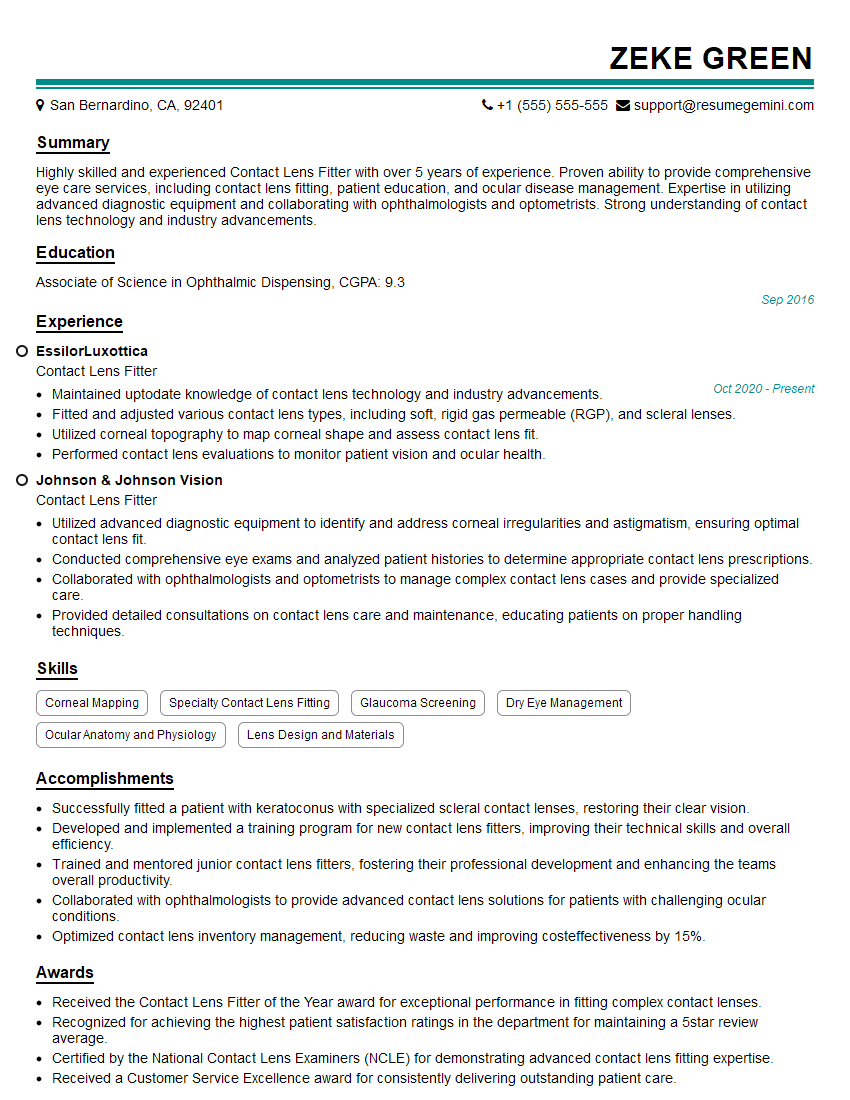
Mastering comprehensive eye exams is crucial for advancing your career in ophthalmology and optometry, opening doors to specialized roles and higher earning potential. To maximize your job prospects, crafting an ATS-friendly resume is essential. ResumeGemini can help you build a professional and impactful resume that highlights your skills and experience. ResumeGemini offers examples of resumes tailored to Comprehensive Eye Exams to provide you with valuable templates and guidance. Take the next step and create a resume that truly showcases your expertise!
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Dear Sir/Madam,
Do you want to become a vendor/supplier/service provider of Delta Air Lines, Inc.? We are looking for a reliable, innovative and fair partner for 2025/2026 series tender projects, tasks and contracts. Kindly indicate your interest by requesting a pre-qualification questionnaire. With this information, we will analyze whether you meet the minimum requirements to collaborate with us.
Best regards,
Carey Richardson
V.P. – Corporate Audit and Enterprise Risk Management
Delta Air Lines Inc
Group Procurement & Contracts Center
1030 Delta Boulevard,
Atlanta, GA 30354-1989
United States
+1(470) 982-2456