Unlock your full potential by mastering the most common Create and Maintain Electronic Health Records (EHR) interview questions. This blog offers a deep dive into the critical topics, ensuring you’re not only prepared to answer but to excel. With these insights, you’ll approach your interview with clarity and confidence.
Questions Asked in Create and Maintain Electronic Health Records (EHR) Interview
Q 1. Explain the difference between an EHR and an EMR.
While the terms are often used interchangeably, there’s a key distinction: an Electronic Medical Record (EMR) is a digital version of a patient’s chart, typically focused on a single healthcare provider or organization. Think of it as a snapshot of a patient’s care within a specific context. An Electronic Health Record (EHR), on the other hand, is a broader, more comprehensive record that can be shared across multiple healthcare organizations. It aims to provide a longitudinal view of a patient’s health journey, encompassing data from various sources throughout their lifetime. Imagine an EMR as a chapter in a book, while the EHR is the entire book, containing multiple chapters from different authors (doctors, specialists, hospitals).
For example, an EMR might contain a patient’s visit notes from a single clinic, while an EHR would include those notes, plus lab results from different labs, imaging reports from various radiology centers, hospital discharge summaries, and even data from wearable devices, all integrated into a single view.
Q 2. Describe your experience with different EHR systems (e.g., Epic, Cerner, Meditech).
I have extensive experience with several leading EHR systems, including Epic, Cerner, and Meditech. My experience spans from data entry and chart review to system administration and troubleshooting. With Epic, I’ve worked extensively with its robust reporting capabilities, using it to generate clinical dashboards and analyze population health data. Cerner‘s user interface was something I particularly appreciated for its intuitive workflow, making documentation more efficient. Finally, with Meditech, I was involved in optimizing its order entry system, contributing to improved workflow and reduced medication errors. In each system, I focused on ensuring data integrity and optimizing system functionality to improve patient care.
Each system has its strengths and weaknesses. For example, Epic is known for its comprehensive functionality but can have a steeper learning curve. Cerner often stands out for its user-friendliness, while Meditech is highly customizable but requires a greater understanding of system configuration.
Q 3. How do you ensure the accuracy and completeness of patient data in an EHR?
Ensuring accurate and complete patient data is paramount. My approach involves a multi-pronged strategy:
- Data Validation Rules: Implementing and maintaining robust data validation rules within the EHR system to flag inconsistencies or illogical entries. For instance, if a patient’s age is entered as 150, the system should immediately flag this as an error.
- Regular Data Audits: Performing regular audits to identify and correct errors. This includes reviewing charts for missing information, inconsistencies, and potential inaccuracies.
- Staff Training: Providing comprehensive training to all staff on proper data entry techniques and the importance of data accuracy. This includes standardized procedures and regular refresher courses.
- Data Reconciliation: Regularly reconciling data from different sources to ensure consistency. For instance, comparing medication lists from the pharmacy with the medication list entered in the EHR.
- Use of Templates and Drop-downs: Utilizing standardized templates and drop-down menus to minimize manual data entry and reduce the potential for errors. This reduces the likelihood of typos or inconsistencies.
These measures ensure data quality and minimize the risk of errors that could negatively impact patient care.
Q 4. What are the HIPAA regulations related to EHRs, and how do you ensure compliance?
HIPAA (Health Insurance Portability and Accountability Act) regulations are crucial for protecting patient health information. My approach to ensuring compliance includes:
- Strict adherence to access controls: Implementing and enforcing strict access controls to limit access to patient data based on the individual’s role and need-to-know basis. Only authorized personnel should have access to specific patient information.
- Data encryption: Utilizing data encryption techniques to protect patient data both in transit and at rest. This prevents unauthorized access to sensitive information, even if the system is compromised.
- Regular security audits: Conducting regular security audits to identify and address potential vulnerabilities in the system. This proactive approach helps to prevent breaches before they occur.
- Employee training on HIPAA compliance: Providing thorough and regular training to all employees on HIPAA regulations and their responsibilities in protecting patient data. This includes awareness of potential security threats and best practices for data protection.
- Incident response plan: Developing and regularly testing an incident response plan to handle potential data breaches or security incidents effectively. This minimizes the impact of any security event.
Understanding and implementing these measures are crucial for maintaining HIPAA compliance and protecting patient privacy.
Q 5. Describe your experience with data entry and data quality in an EHR.
My experience with data entry and data quality focuses on accuracy, efficiency, and completeness. I have expertise in using various data entry methods, including structured data entry forms, and free-text documentation. I understand the importance of accurate coding and the use of standardized terminologies like SNOMED CT and LOINC to ensure data consistency and interoperability. Data quality is not just about correct information; it’s about consistent and complete documentation. I’ve worked on projects improving data quality by implementing data validation rules, using automated data entry tools, and conducting regular data audits to identify and correct inaccuracies. This ensures that the information recorded accurately reflects the patient’s condition and care.
For example, I’ve implemented systems that automatically populate certain fields in the EHR based on other entries, reducing manual data entry and associated errors. I’ve also developed training programs to educate staff on best practices in data entry and ensure data quality.
Q 6. How do you handle discrepancies or errors in patient data within the EHR?
Handling discrepancies or errors in patient data requires a systematic approach. First, I would identify the discrepancy and determine its nature. Then, I would investigate the source of the error – was it a data entry mistake, a system glitch, or an issue with data integration? Depending on the nature and severity of the error, I’d follow established protocols. This may involve correcting the data directly if authorized, documenting the discrepancy with an explanation and a correction note, or escalating the issue to a supervisor or IT department if needed. For significant discrepancies, a formal process might be required, potentially involving chart review by multiple clinicians. Accurate documentation of the error and resolution process is crucial, as is following established audit trail procedures. Patient safety is always the priority.
For example, if there’s a conflict between medication lists from different sources, I would carefully compare the information, consult with the prescribing physician if necessary, and ensure the most accurate and up-to-date information is reflected in the EHR.
Q 7. Explain your understanding of different EHR functionalities, such as charting, ordering, and reporting.
EHR functionalities are integral to efficient healthcare delivery. I am proficient in several key areas:
- Charting: This involves documenting patient encounters, including history, physical examination findings, diagnoses, and treatment plans. Proficiency in structured and unstructured data entry and proper use of clinical terminologies is crucial for effective charting.
- Ordering: EHRs allow for electronic ordering of lab tests, radiology studies, medications, and consultations. This streamlines the ordering process, reduces errors, and improves efficiency. I’m experienced in using various ordering workflows and ensuring appropriate authorization and verification processes are in place.
- Reporting: EHRs generate a wide variety of reports, including patient summaries, clinical dashboards, and population health reports. I have expertise in using EHR reporting tools to analyze data, track key metrics, and identify trends in patient care. This includes generating reports for quality improvement, regulatory compliance, and clinical research purposes.
Understanding these functionalities and integrating them into daily practice is essential for providing high-quality and efficient patient care.
Q 8. How do you prioritize tasks when managing a high volume of EHR data?
Prioritizing tasks in EHR management with high data volume requires a structured approach. Think of it like triage in a hospital – the most critical needs get addressed first. I use a combination of methods:
- Urgency and Importance Matrix: I categorize tasks based on urgency (immediate, short-term, long-term) and importance (critical, important, less important). This helps me visualize which tasks need immediate attention and which can be delegated or scheduled.
- Workflow Optimization: I analyze existing workflows to identify bottlenecks and inefficiencies. For example, if data entry is slowing down the process, I’d investigate implementing automation tools or streamlining the data entry forms.
- Technology Leverage: EHR systems often have built-in task management tools and reporting features. Utilizing these allows for better tracking, prioritization, and delegation. For instance, flagging critical alerts or setting reminders for overdue tasks.
- Team Collaboration: Effective communication and delegation are crucial. I ensure the team is aware of priorities and actively involve them in task management, leveraging their expertise and freeing up my time for higher-level tasks.
For example, if a patient’s critical lab results are overdue, that takes precedence over updating less urgent patient demographics. By strategically prioritizing, I ensure timely and efficient processing of all EHR data.
Q 9. Describe your experience with EHR security protocols and best practices.
EHR security is paramount. My experience encompasses a wide range of protocols and best practices, including:
- Access Control: Implementing role-based access control (RBAC) to restrict access to data based on job responsibilities. Only authorized personnel can access sensitive patient information. For example, nurses may have access to medication records, but not billing information.
- Data Encryption: Ensuring all data, both in transit and at rest, is encrypted using strong encryption algorithms (like AES-256) to protect against unauthorized access even if a breach occurs.
- Regular Security Audits and Vulnerability Assessments: Conducting regular security checks and penetration testing to identify and address vulnerabilities before they can be exploited. This includes checking for weak passwords, outdated software, and insecure configurations.
- Compliance with Regulations: Adherence to regulations such as HIPAA (Health Insurance Portability and Accountability Act) and other relevant data privacy laws. This includes implementing robust audit trails to track all access to patient data.
- Employee Training: Providing regular security awareness training to all staff to educate them on phishing scams, social engineering tactics, and secure password management. A well-trained workforce is a strong line of defense.
In a past role, I implemented a multi-factor authentication system, significantly reducing the risk of unauthorized access. This layered approach ensures robust EHR security, aligning with best practices and industry standards.
Q 10. How familiar are you with HL7 and other health data interoperability standards?
I’m highly familiar with HL7 (Health Level Seven) and other health data interoperability standards. HL7 is a crucial standard for exchanging electronic health information between different healthcare systems. My experience includes:
- HL7 Messaging: Working with various HL7 message types (e.g., ADT, ORU, ORM) to integrate EHR systems with other healthcare applications such as lab systems, pharmacy systems, and picture archiving and communication systems (PACS).
- FHIR (Fast Healthcare Interoperability Resources): Understanding and utilizing FHIR, the newer, more flexible standard for exchanging healthcare data using APIs (Application Programming Interfaces). This allows for greater integration and data sharing capabilities.
- Interface Engine Configuration: Experience configuring and managing interface engines to facilitate seamless data exchange between different systems. This involves mapping data fields, troubleshooting integration issues, and ensuring data integrity.
- Data Mapping and Transformation: Understanding how to map data elements between different systems, handling data transformations to ensure compatibility and consistency. This often involves dealing with variations in data formats and terminology.
For instance, I was involved in a project that integrated our EHR system with a regional health information exchange (HIE) using HL7 FHIR, enabling secure sharing of patient data across different healthcare organizations within the region.
Q 11. Explain your experience with EHR reporting and data analysis.
EHR reporting and data analysis are critical for improving patient care, operational efficiency, and clinical decision-making. My experience includes:
- Data Extraction and Transformation: Extracting data from the EHR system using various methods (e.g., SQL queries, report writers) and transforming it into a usable format for analysis. This often requires cleaning and standardizing data to ensure accuracy.
- Data Visualization: Creating meaningful visualizations using tools like Tableau or Power BI to effectively communicate key findings to stakeholders. This might involve creating charts, graphs, and dashboards to illustrate trends and patterns in patient data.
- Report Generation: Developing custom reports to meet specific needs, such as analyzing readmission rates, tracking medication adherence, or assessing the effectiveness of treatment protocols. This involves understanding the data required and designing reports that provide actionable insights.
- Statistical Analysis: Performing statistical analysis to identify trends, correlations, and significant differences in patient data. This might involve using techniques such as regression analysis or hypothesis testing to answer specific clinical questions.
For example, I developed a report that analyzed patient readmission rates within 30 days of discharge. This revealed a specific area for improvement in discharge planning, leading to the implementation of new protocols and a subsequent reduction in readmissions.
Q 12. How do you ensure patient confidentiality and data privacy within the EHR?
Patient confidentiality and data privacy are paramount. My approach to ensuring this within the EHR system involves a multi-faceted strategy:
- Strict Adherence to Policies and Procedures: Following strict protocols for access control, data encryption, and data disposal in accordance with HIPAA and other relevant regulations.
- Regular Security Audits: Conducting regular security audits and vulnerability assessments to identify and mitigate any potential risks to patient data. This includes checking access logs for unusual activity.
- Employee Training: Providing comprehensive training to all staff on privacy regulations, best practices, and the importance of protecting patient data. This is reinforced through regular refreshers and awareness campaigns.
- Data Minimization: Collecting and storing only the minimum necessary patient information, minimizing the risk of unauthorized disclosure. Only relevant data is collected and stored.
- Incident Response Plan: Having a well-defined incident response plan in place to handle any data breaches or security incidents promptly and effectively. This plan outlines the steps to take in the event of a security breach.
Imagine a scenario where a staff member accidentally accesses a patient’s record without authorization. Our incident response plan would trigger an investigation, ensuring the breach is contained and appropriate action is taken.
Q 13. Describe your experience with EHR training and education for medical staff.
EHR training is crucial for effective system utilization and improved patient care. My experience includes developing and delivering training programs for medical staff using various methods:
- Needs Assessment: Starting with a thorough needs assessment to identify specific training requirements based on roles and skill levels. This ensures the training is relevant and targeted.
- Modular Training: Developing modular training programs that break down complex topics into manageable segments. This allows for flexible learning and targeted skill development.
- Hands-on Training: Including extensive hands-on training sessions using realistic scenarios to allow staff to practice using the EHR system in a safe environment.
- Ongoing Support and Resources: Providing ongoing support and resources such as quick reference guides, FAQs, and online help resources to address questions and issues that arise after initial training.
- Feedback Mechanisms: Implementing feedback mechanisms to assess the effectiveness of training and identify areas for improvement. This ensures the training program remains current and relevant.
In a previous role, I developed a comprehensive EHR training program that reduced training time by 25% and significantly improved user satisfaction, leading to increased adoption and improved efficiency.
Q 14. What are some common challenges in managing EHR systems, and how have you overcome them?
Managing EHR systems presents several challenges:
- Data Interoperability: Integrating different EHR systems and applications can be complex and challenging, requiring careful planning and coordination. This often involves dealing with varying data formats and standards.
- System Downtime: System downtime can disrupt clinical workflows and compromise patient care. Having robust backup and recovery plans is crucial to minimize disruption.
- Data Security and Privacy: Protecting sensitive patient data from unauthorized access and breaches is a continuous challenge, requiring ongoing vigilance and investment in security measures.
- User Adoption and Training: Getting medical staff to adopt and effectively use the EHR system can be challenging. Comprehensive training and ongoing support are essential for successful implementation.
- Cost of Maintenance and Upgrades: EHR systems require significant ongoing investment in maintenance, upgrades, and support. Budget planning and resource allocation are crucial.
For example, when facing system downtime, I implemented a temporary workaround using paper-based charts while working with IT to resolve the issue quickly. For interoperability issues, I actively participated in system integration projects, collaborating with vendors and other healthcare providers to ensure seamless data exchange.
Q 15. How do you stay current with the latest updates and advancements in EHR technology?
Staying current in the rapidly evolving field of EHR technology requires a multi-pronged approach. It’s not enough to simply rely on one source of information. I actively engage in several strategies to maintain my expertise.
- Professional Organizations: I am a member of HIMSS (Healthcare Information and Management Systems Society) and AMIA (American Medical Informatics Association). These organizations provide access to webinars, conferences, journals, and networking opportunities that keep me abreast of the latest trends and best practices.
- Industry Publications and Websites: I regularly read publications like Healthcare IT News, Modern Healthcare, and others focusing on EHR technology. I also follow key vendors’ websites and blogs for updates on their products and services.
- Continuing Education: I actively pursue continuing education credits through online courses and workshops focused on EHR system updates, data analytics, and security protocols. This ensures my skills remain sharp and relevant.
- Vendor-Specific Training: Given the breadth of EHR systems, in-depth training is crucial. I actively participate in vendor-provided training sessions for the specific systems I work with, paying close attention to new features, updates, and functionality.
- Networking and Collaboration: Attending industry events and engaging with colleagues in the field allows me to share knowledge and insights, learn about new developments, and discuss challenges we’re all facing. This collaborative learning is invaluable.
Essentially, I view staying current as an ongoing process, not a one-time event. It’s a commitment to continuous learning and professional development that ensures I remain a valuable asset in this field.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Describe your experience with EHR system implementation and upgrades.
I have extensive experience with EHR system implementation and upgrades, having participated in several projects across different healthcare settings. My role has ranged from initial needs assessment and vendor selection to user training and post-implementation support.
- Implementation: In one project, we implemented Epic at a large hospital system. My responsibilities included configuring the system, customizing workflows, developing training materials, and conducting user training sessions. We followed a phased approach, starting with pilot units before rolling out system-wide. This allowed for early identification and resolution of issues, improving overall success.
- Upgrades: I’ve managed multiple EHR system upgrades, including migrating data to newer versions and addressing compatibility issues with other systems. For instance, upgrading a smaller clinic’s system to a newer version required rigorous data validation and verification to ensure data integrity throughout the process. We mapped the old data fields to the new ones meticulously, ensuring a smooth transition with minimal disruption.
- Change Management: A critical component of both implementation and upgrades is effective change management. I understand that transitions can be difficult, so my approach emphasizes clear communication, comprehensive training, and providing ongoing support to users throughout the process. This minimizes user frustration and improves adoption rates.
Throughout these experiences, I’ve learned the importance of meticulous planning, rigorous testing, and strong communication. These are key to the success of any EHR implementation or upgrade project.
Q 17. How do you troubleshoot common EHR system problems?
Troubleshooting EHR system problems requires a systematic approach. My strategy typically involves a series of steps, beginning with the most basic and progressing to more advanced solutions if necessary.
- Identify the Problem: Clearly define the issue. Is it a software glitch, a hardware problem, a user error, or a connectivity issue? Gather all relevant information, such as error messages, timestamps, and affected users.
- Check for Simple Solutions: Before diving into complex troubleshooting, check for obvious solutions. This could include verifying internet connectivity, restarting the computer, or checking for system updates.
- Consult Documentation and Knowledge Bases: Most EHR systems have comprehensive documentation and knowledge bases. These resources often contain solutions to common problems. I thoroughly search these resources before escalating the issue.
- Use System Logs and Audit Trails: Examining system logs and audit trails can often pinpoint the root cause of the problem. These logs provide detailed information on system activity and can reveal errors or unexpected behaviors.
- Contact Support: If the problem persists, I contact the EHR vendor’s support team. I clearly articulate the issue, provide all relevant information, and follow their instructions to resolve the problem.
For example, if a user reports they can’t access patient charts, I would first check their network connection and login credentials. Then I would examine system logs for any access errors. If the issue persists, I’d contact the vendor’s support team.
Q 18. Explain your experience with using EHR systems for clinical documentation improvement.
EHR systems are crucial for clinical documentation improvement. My experience includes using EHR functionalities to ensure accurate, complete, and timely documentation. This improves patient care, reduces errors, and supports compliance with regulations.
- Templates and Order Sets: I utilize standardized templates and order sets within the EHR to guide documentation, ensuring consistency and completeness. This reduces the risk of omitting critical information.
- Clinical Decision Support Systems (CDSS): EHR systems often incorporate CDSS, which provide alerts and reminders to help clinicians make informed decisions and improve documentation. For instance, reminders about preventive screenings or medication reconciliation contribute significantly to documentation completeness.
- Data Analytics and Reporting: I use EHR data analytics to identify areas for improvement in documentation. This may involve analyzing the frequency of incomplete notes or identifying patterns of documentation errors. Using this data, tailored training or process improvements can then be implemented.
- Auditing and Compliance: Ensuring documentation adheres to regulatory requirements is vital. EHR systems help in auditing documentation and identifying areas for improvement to ensure compliance with standards like Meaningful Use.
For example, by analyzing documentation trends, we noticed a significant number of missing allergy details. By implementing a new template with a prominent allergy section and educating clinicians, we drastically reduced this omission.
Q 19. How familiar are you with different EHR interfaces and integration points?
I’m very familiar with various EHR interfaces and integration points. Understanding how different systems communicate and exchange data is critical for seamless workflow and data sharing.
- HL7: I have extensive experience with Health Level Seven (HL7) messaging, the standard protocol for exchanging healthcare information between different systems. This includes understanding HL7 message types, segments, and fields, and troubleshooting integration issues.
- FHIR: I am familiar with Fast Healthcare Interoperability Resources (FHIR), the newer standard for interoperability. I understand its benefits in improving data exchange and its potential in building more agile and adaptable healthcare systems.
- APIs: I’m proficient in working with Application Programming Interfaces (APIs) to integrate EHR systems with other applications, such as billing systems, lab information systems, and patient portals.
- Data Mapping: A crucial aspect of integration is data mapping, which involves aligning data elements between different systems. I have experience in mapping data fields to ensure data consistency and accurate transfer.
Understanding these interfaces allows for the smooth exchange of data, reducing manual processes and improving efficiency in things like order entry, results reporting, and billing. For example, I have worked on projects integrating EHRs with pharmacy systems to automate medication reconciliation, improving patient safety and reducing medication errors.
Q 20. How do you manage and resolve EHR-related technical issues?
Managing and resolving EHR-related technical issues requires a methodical approach combining technical expertise with problem-solving skills. My approach focuses on efficient issue resolution, minimizing downtime and user disruption.
- Prioritization: I prioritize issues based on their severity and impact. Critical issues that affect patient care or system stability are addressed immediately. Less urgent issues are handled according to their priority.
- Remote Support and Diagnostics: Leveraging remote access tools allows me to quickly diagnose and resolve many issues without needing on-site intervention. This speeds up troubleshooting and reduces downtime.
- Escalation Procedures: I know when and how to escalate issues to the appropriate levels. This includes contacting vendor support, engaging internal IT teams, or reporting security breaches according to established protocols.
- Documentation and Tracking: I meticulously document all issues, troubleshooting steps, and resolutions. This provides a record for future reference and helps identify recurring problems.
- Preventive Maintenance: To minimize disruptions, I am proactive in performing regular system maintenance, such as software updates, security patching, and backup verification. Regular backups are particularly crucial to mitigate data loss in case of system failures.
For instance, a recent network outage affecting EHR access required immediate escalation to the IT team to restore network connectivity. Once resolved, I documented the incident and steps taken for future reference and improvement of the system’s robustness.
Q 21. Describe your experience with audit trails and data integrity in EHR systems.
Audit trails and data integrity are paramount in EHR systems. They ensure accountability, maintain data accuracy, and support legal and regulatory compliance. My experience includes:
- Understanding Audit Trail Functionality: I understand how audit trails record user activities within the EHR system. This includes user logins, data modifications, and access permissions. I can effectively use this information to track down data changes or access patterns.
- Data Integrity Checks: I’m proficient in performing data integrity checks to ensure data accuracy and completeness. This involves verifying data consistency across different systems and identifying any discrepancies. Data cleansing and validation are crucial steps in maintaining this integrity.
- Security and Access Control: I’m familiar with security protocols and access control mechanisms that protect EHR data. I understand the importance of role-based access control (RBAC) to ensure that only authorized users have access to specific data and functionalities. I also know how to identify and respond to potential security breaches.
- Compliance and Regulations: I am aware of regulations like HIPAA (Health Insurance Portability and Accountability Act) and understand how audit trails and data integrity contribute to compliance. This includes proper documentation and procedures to ensure data protection and privacy.
For example, an unusual pattern of access to a specific patient’s record triggered an audit trail review. This revealed unauthorized access, allowing us to investigate and take appropriate action to prevent future breaches.
Q 22. What is your experience with using EHR systems for billing and coding?
My experience with EHR systems for billing and coding is extensive. I’m proficient in using EHR functionality to generate accurate claims, ensuring proper coding based on medical documentation. This involves a deep understanding of CPT, HCPCS, and ICD-10 coding systems. I’ve worked with various EHR platforms, such as Epic and Cerner, mastering their respective billing modules.
For example, in my previous role, I streamlined the billing process by implementing a pre-billing audit system within our EHR. This involved creating custom reports to identify coding inconsistencies and missing information before claims were submitted, significantly reducing claim denials. This also involved regular training for our coding staff to ensure everyone was up-to-date on the latest coding guidelines and EHR features. We saw a 15% reduction in denied claims within six months of implementing this system.
Beyond basic billing, I’m also experienced in generating reports to analyze revenue cycles, identify areas for improvement, and manage payer contracts. This includes analyzing denial trends to proactively address recurring issues and improving overall efficiency.
Q 23. Explain your understanding of different data security measures in EHR systems.
Data security in EHR systems is paramount. My understanding encompasses a multi-layered approach involving administrative, physical, and technical safeguards. Administrative safeguards include establishing clear policies and procedures for access control, data breach response, and employee training on HIPAA compliance. Physical safeguards focus on securing the physical location of servers and workstations, controlling access to those areas, and implementing disaster recovery plans.
Technical safeguards form the core of EHR security. This includes:
- Access control: Using role-based access control (RBAC) to limit user access to only the data they need. For example, a nurse should only access patient records relevant to their care, not the entire system.
- Encryption: Protecting data both in transit and at rest using strong encryption algorithms to prevent unauthorized access.
- Auditing: Maintaining comprehensive audit trails that track all user activity within the EHR system. This allows for detection of suspicious activity and investigation of potential breaches.
- Firewall and intrusion detection systems: Protecting the EHR system from external threats through firewalls and intrusion detection systems that monitor network traffic and block malicious activity.
I’m also familiar with the importance of regular security assessments, penetration testing, and vulnerability management to identify and address potential weaknesses proactively.
Q 24. How familiar are you with various EHR reporting tools and functionalities?
I’m highly familiar with various EHR reporting tools and functionalities. My experience spans creating custom reports for various purposes, from tracking key performance indicators (KPIs) to analyzing patient demographics and treatment outcomes. I’m proficient in using both built-in reporting tools and specialized reporting software that integrates with the EHR.
For instance, I’ve used Epic’s reporting workbench to generate reports on medication reconciliation rates, identifying opportunities for improvement in patient safety. I also used Crystal Reports to create customized reports tailored to specific clinical needs, such as analyzing the effectiveness of a new treatment protocol. Understanding the data structure and querying capabilities of each system is crucial for effective reporting.
My skills extend beyond report generation to the interpretation and analysis of the results. I can transform raw data into actionable insights that inform clinical decision-making and support quality improvement initiatives.
Q 25. Describe your experience with using EHR data for quality improvement initiatives.
I’ve extensively used EHR data to support quality improvement initiatives. This involves identifying trends, patterns, and areas needing improvement within a healthcare setting. I use data analysis to track key metrics, identify areas of concern and guide interventions designed to optimize patient care.
For example, in a previous role, we used EHR data to analyze readmission rates for patients with heart failure. By identifying high-risk patients and implementing a proactive discharge planning protocol, we were able to reduce readmission rates by 12% within a year. The EHR data was instrumental in this process, allowing us to track patient outcomes and measure the effectiveness of our interventions.
My approach involves a data-driven cycle of Plan-Do-Study-Act (PDSA). The EHR provides the data for the ‘Study’ phase, which informs the next ‘Plan’ iteration. This continuous improvement model, underpinned by EHR data analysis, is essential for optimal patient care and efficient operational management.
Q 26. How do you contribute to a positive and collaborative team environment in an EHR setting?
Contributing to a positive and collaborative team environment in an EHR setting is crucial for success. I believe in open communication, active listening, and mutual respect. I actively participate in team discussions, sharing my knowledge and expertise to support colleagues and foster a spirit of teamwork.
For example, I regularly conduct training sessions for new team members on EHR functionalities, ensuring everyone is comfortable and proficient. I also proactively offer support to colleagues who are facing challenges with the EHR system. I find that a collaborative approach where everyone feels valued and supported leads to a more efficient and productive work environment. This often involves pairing up with others on challenging projects, learning from each other’s expertise.
I strive to create an environment where everyone feels empowered to contribute their ideas and opinions, creating a dynamic and supportive setting that promotes innovation and continuous improvement.
Q 27. Explain your experience with resolving conflicts related to EHR usage or data access.
Resolving conflicts related to EHR usage or data access requires a calm, professional approach that prioritizes data security and patient privacy. My strategy involves active listening to understand all perspectives involved. I then apply my knowledge of EHR policies, procedures, and HIPAA regulations to facilitate a resolution.
In one instance, a dispute arose between two departments regarding access to a specific patient record. By carefully reviewing access privileges and workflows, I determined the appropriate level of access for each department, ensuring both departments had the necessary information without compromising data security. This involved explaining the rationale behind my decision clearly and transparently, ensuring everyone understood the process.
For complex issues, I facilitate mediation between involved parties, promoting clear communication and collaboration to reach a mutually agreeable solution. Documentation is key, ensuring a transparent record of the issue and its resolution.
Q 28. Describe your experience with regulatory compliance and audits related to EHR systems.
Regulatory compliance and audits related to EHR systems are critical. My experience includes ensuring adherence to HIPAA, Meaningful Use, and other relevant regulations. This involves implementing and maintaining robust security measures, conducting regular audits, and staying updated on evolving regulations.
I’ve participated in several internal and external audits, providing documentation and demonstrating compliance with regulatory requirements. I am adept at identifying and addressing potential compliance gaps proactively. For example, I’ve implemented procedures to ensure timely completion of patient record documentation, which is crucial for audit compliance. I also maintain accurate logs of all system changes and security events.
Understanding the nuances of various regulations and their application to our daily EHR usage is critical for maintaining compliance and avoiding penalties. Staying current with updates and best practices is an ongoing process that requires continuous attention to detail.
Key Topics to Learn for Create and Maintain Electronic Health Records (EHR) Interview
- Data Entry and Accuracy: Mastering efficient and accurate data entry practices within the EHR system. Understanding data validation and error correction procedures.
- Patient Charting: Practical application of charting techniques, including documenting patient history, symptoms, diagnoses, treatments, and progress notes. Understanding HIPAA compliance and patient confidentiality.
- Medical Terminology and Abbreviations: Demonstrating proficiency in understanding and using standard medical terminology and abbreviations within the EHR system. This includes accurate documentation and avoiding misinterpretations.
- EHR System Navigation: Proficiency in navigating the specific EHR system used by the potential employer (e.g., Epic, Cerner). Understanding features like scheduling, order entry, and result retrieval.
- Reporting and Analytics: Understanding how to generate reports and extract data from the EHR system for analysis. Familiarity with common reporting requirements.
- Workflow Optimization: Identifying and suggesting improvements to streamline EHR workflows for increased efficiency and accuracy. Understanding the impact of EHR usage on overall clinic/hospital productivity.
- Security and Compliance: Understanding HIPAA regulations, data security protocols, and maintaining patient privacy within the EHR environment. Knowing how to handle potential security breaches.
- Problem-solving & Troubleshooting: Demonstrating the ability to troubleshoot common EHR issues, such as system errors, data inconsistencies, and technical difficulties.
Next Steps
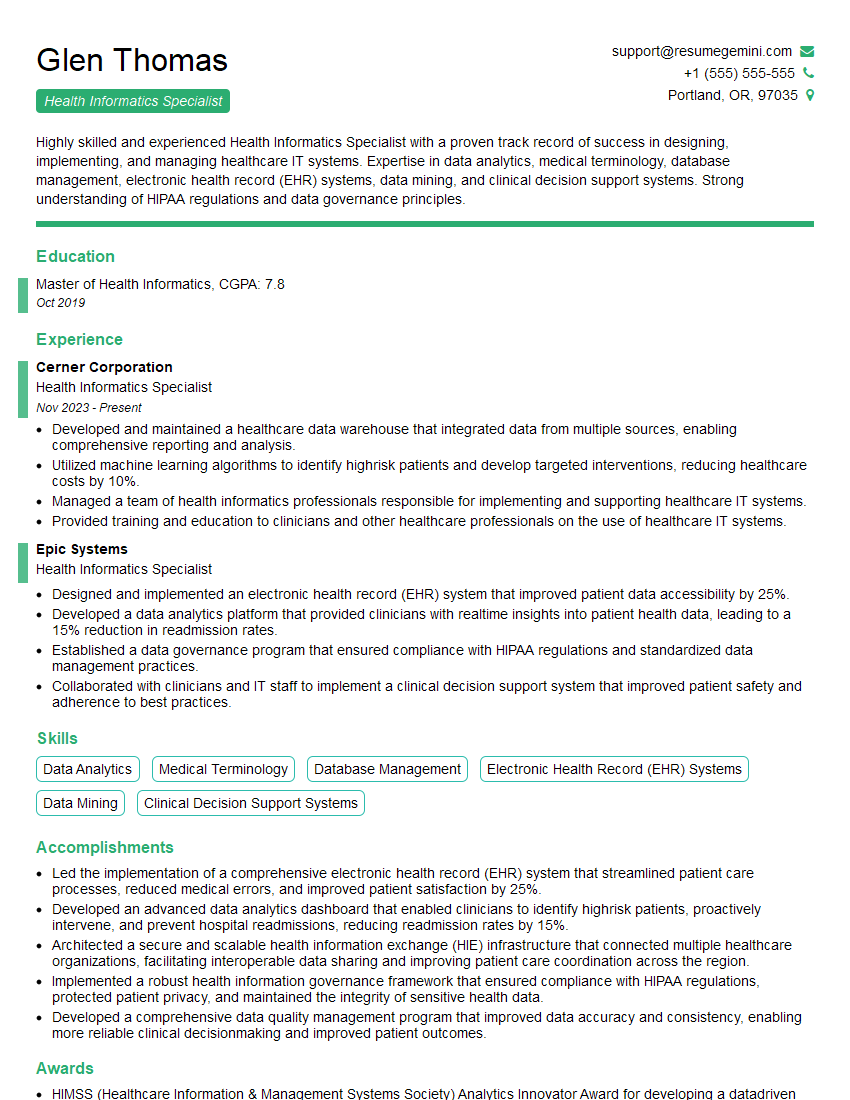
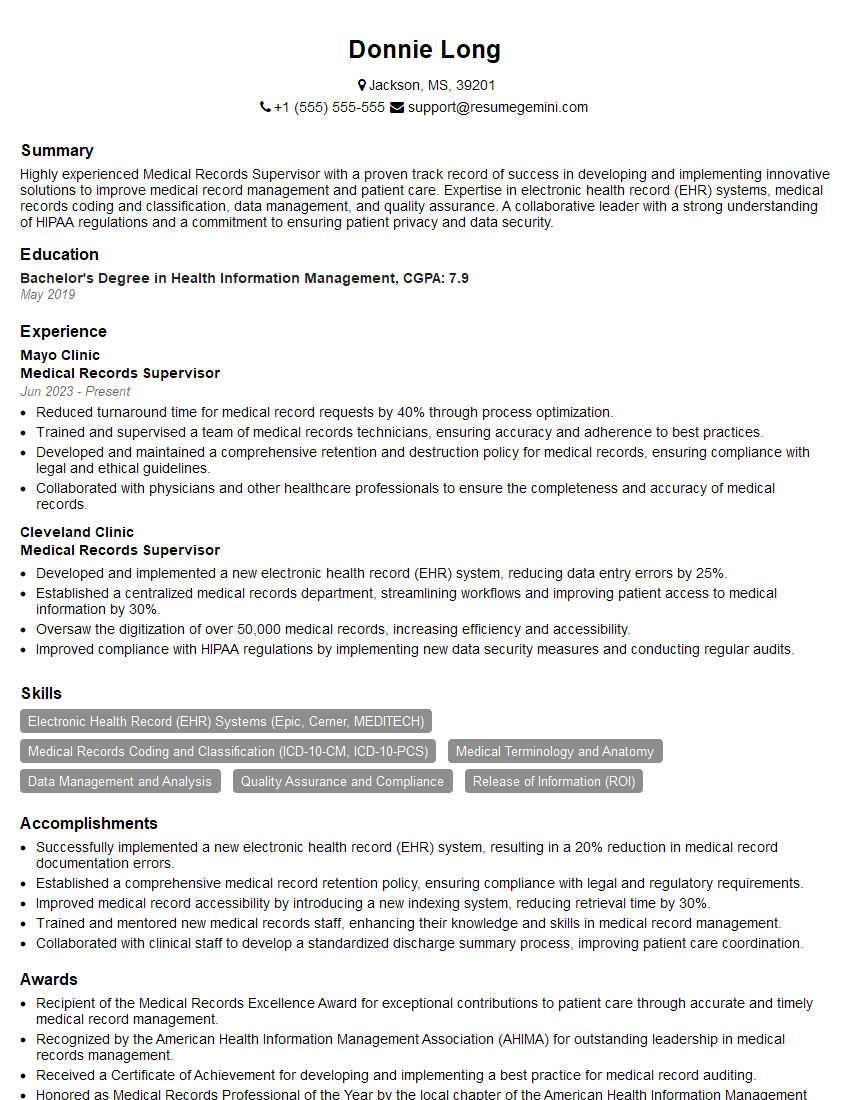
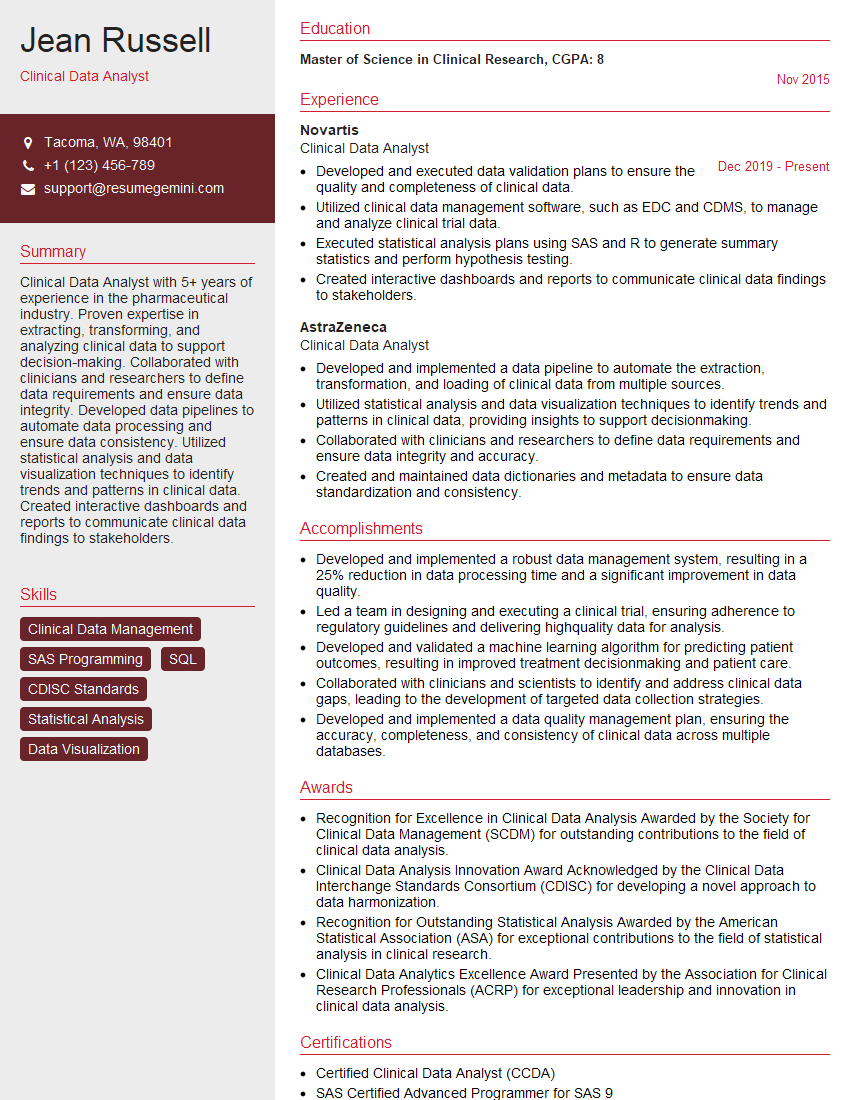
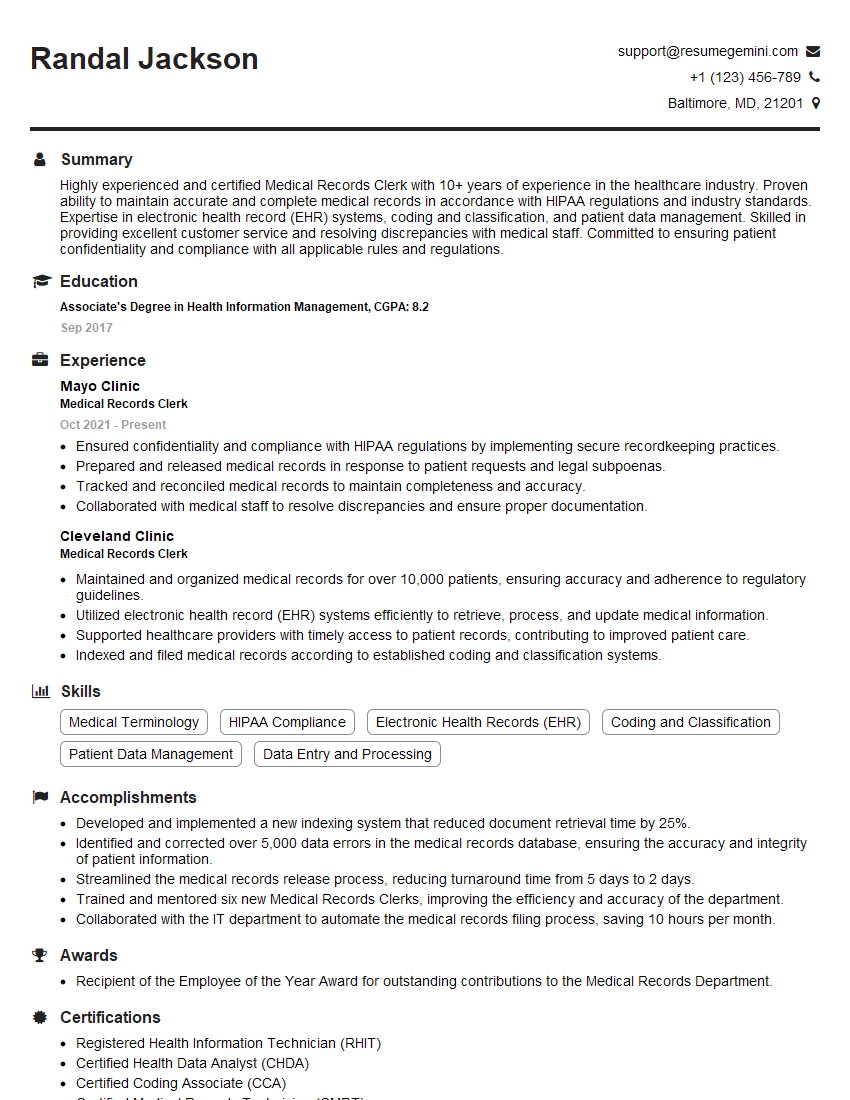
Mastering the creation and maintenance of Electronic Health Records is crucial for career advancement in healthcare. A strong understanding of EHR systems demonstrates valuable skills and significantly increases your marketability to potential employers. To maximize your chances of landing your dream role, it’s essential to create an ATS-friendly resume that highlights your key skills and experiences. ResumeGemini is a trusted resource to help you build a professional and impactful resume that catches the eye of recruiters. Examples of resumes tailored to Create and Maintain Electronic Health Records (EHR) roles are available to guide you through the process.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Interesting Article, I liked the depth of knowledge you’ve shared.
Helpful, thanks for sharing.
Hi, I represent a social media marketing agency and liked your blog
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?