Are you ready to stand out in your next interview? Understanding and preparing for Hand Technique interview questions is a game-changer. In this blog, we’ve compiled key questions and expert advice to help you showcase your skills with confidence and precision. Let’s get started on your journey to acing the interview.
Questions Asked in Hand Technique Interview
Q 1. Describe your experience with various hand splinting techniques.
My experience with hand splinting encompasses a wide range of techniques, tailored to specific injuries and conditions. I’m proficient in applying various types of splints, including static splints for immobilization (like those used after a fracture), dynamic splints which allow for controlled movement and assist with regaining function (often used in tendon injuries), and serial splints that are progressively adjusted to gradually improve range of motion. I regularly utilize volar, dorsal, and ulnar gutter splints for specific finger and wrist injuries. For example, a volar splint is ideal for stabilizing a fracture of the metacarpals, while a ulnar gutter splint is perfect for supporting a fractured fifth metacarpal.
Selection of the appropriate splint depends critically on the diagnosis, the patient’s comfort level, and the desired functional outcome. I always consider factors like the patient’s age, occupation, and overall health when making this crucial decision. Proper splint application requires careful attention to padding to prevent pressure sores and ensure patient comfort, ensuring the splint neither restricts blood flow nor causes undue discomfort.
Q 2. Explain the difference between tendon gliding exercises and nerve gliding exercises.
Tendon gliding exercises and nerve gliding exercises, while both important for hand rehabilitation, target different structures and have distinct goals. Tendon gliding exercises focus on improving the smooth movement of tendons within their sheaths. These exercises involve sequentially flexing and extending each finger individually to ensure each tendon moves independently, preventing adhesions which may restrict motion and cause pain. Think of it like lubricating the moving parts of a machine.
Nerve gliding exercises, on the other hand, aim to improve the gliding of nerves through their surrounding tissues. This is crucial as nerve entrapment can lead to pain, numbness, and tingling. These exercises involve specific movements designed to create tension and release along the nerve pathway. For instance, to glide the median nerve, I might instruct the patient to extend their wrist while flexing their fingers, which stretches the nerve.
The key difference lies in their target: tendons versus nerves. Often, a comprehensive rehabilitation program will include both types of exercises to achieve optimal hand function after injury or surgery.
Q 3. How do you assess for carpal tunnel syndrome?
Assessing for carpal tunnel syndrome involves a combination of clinical evaluation and possibly electrodiagnostic studies. The clinical assessment starts with a thorough patient history, focusing on symptoms like numbness, tingling, and pain in the hand and fingers, particularly at night or with repetitive movements. I’d then perform a physical examination, including:
- Phalen’s test: Holding wrists in a flexed position for 60 seconds to exacerbate symptoms.
- Tinel’s sign: Tapping over the median nerve at the wrist to elicit tingling.
- Sensory testing: Assessing light touch, pinprick, and two-point discrimination in the median nerve distribution.
- Thenar muscle atrophy: Checking for muscle wasting in the thumb’s base.
Electrodiagnostic studies, such as nerve conduction studies (NCS) and electromyography (EMG), can provide objective evidence of median nerve compression, confirming the diagnosis. These studies measure the speed of nerve impulses and muscle activity, helping to differentiate carpal tunnel syndrome from other conditions presenting with similar symptoms.
Q 4. What are the common causes of Dupuytren’s contracture?
Dupuytren’s contracture is a progressive hand condition causing thickening and shortening of the palmar fascia, leading to finger contractures. The exact cause remains unknown, but several factors contribute to its development:
- Genetics: A strong hereditary component is well-established. A family history significantly increases the risk.
- Age: It predominantly affects individuals over 40 years old.
- Gender: Men are more commonly affected than women.
- Diabetes: Certain medical conditions like diabetes can increase the risk.
- Epilepsy: Similarly, epilepsy has been associated with an increased prevalence.
- Alcoholism: Chronic alcohol use is another established risk factor.
The interplay of these factors is likely complex, and research continues to unravel the precise mechanisms behind Dupuytren’s contracture.
Q 5. Describe your experience with treating fractures of the hand and wrist.
My experience with treating hand and wrist fractures is extensive. Management involves a multi-faceted approach, beginning with proper diagnosis through imaging studies like X-rays and CT scans. Treatment choices vary greatly depending on the type and severity of the fracture, patient age, overall health, and fracture location.
For many fractures, closed reduction—manipulating the bones back into alignment without surgery—followed by immobilization with a cast or splint is sufficient. However, some fractures might need open reduction and internal fixation (ORIF), meaning surgical intervention to align the bones and secure them with plates, screws, or pins. Post-operative care is crucial and includes regular monitoring, pain management, early mobilization (often with a therapist), and diligent follow-up to ensure proper healing and restoration of function. I always emphasize the importance of patient education and compliance with the prescribed treatment plan for optimal outcomes.
Q 6. What are the different types of hand grafts and when would you use each?
Several types of hand grafts are used to repair skin defects following trauma or surgery. The choice depends on the size and location of the defect, the availability of donor sites, and the overall patient health.
- Full-thickness skin grafts: These contain all skin layers (epidermis and dermis) and provide superior cosmetic and functional results, but donor sites are limited.
- Split-thickness skin grafts: These contain only part of the dermis, making them easier to harvest in larger quantities and useful for covering extensive wounds. However, the cosmetic result is less ideal.
- Free flaps: These involve transferring a tissue flap with its own blood supply from a donor site to the recipient site. This is particularly useful for large or complex defects, requiring microsurgical techniques to re-establish blood flow.
For example, a full-thickness graft might be ideal for a small defect on the palm, while a split-thickness graft could be suitable for a larger burn wound on the dorsal hand. A free flap would be reserved for complex scenarios like significant trauma or reconstructive procedures following tumor resection.
Q 7. Explain your approach to managing post-surgical hand edema.
Managing post-surgical hand edema is critical for optimal recovery and minimizing long-term complications. My approach is multi-pronged and begins pre-operatively with measures to reduce the risk of excessive edema. This includes elevation of the limb, early mobilization as tolerated, and compression therapy using specialized bandages or gloves.
Post-operatively, I continue with elevation, compression bandaging, regular range-of-motion exercises, and potentially modalities such as ice and ultrasound therapy, to reduce swelling and promote lymphatic drainage. In some cases, I may recommend manual lymphatic drainage massage, performed by a trained therapist, to further aid in fluid removal. If edema is severe or unresponsive to conservative measures, I might consider more advanced interventions such as medication to reduce inflammation or, in rare circumstances, surgical intervention.
Patient education and compliance are crucial. I emphasize the importance of frequent elevation, consistent use of compression bandages, and adherence to the prescribed exercise program. Regular follow-up appointments allow me to monitor progress and adjust the treatment plan as needed.
Q 8. How do you assess a patient’s functional capacity after a hand injury?
Assessing functional capacity after a hand injury involves a comprehensive evaluation focusing on the patient’s ability to perform activities of daily living (ADLs). We don’t just look at range of motion; we assess how that range of motion translates into function.
My assessment begins with a thorough history, including the mechanism of injury and the patient’s occupation and hobbies. This helps me understand the demands placed on their hand before the injury and tailor the assessment accordingly. Then, I perform a physical exam, evaluating:
- Range of motion (ROM): Using a goniometer, I measure active and passive ROM of each joint. Restricted ROM can significantly impact grip strength and dexterity.
- Grip strength: I use a dynamometer to measure grip strength, comparing the injured hand to the uninjured hand. A significant difference indicates functional deficit.
- Dexterity and fine motor skills: Tests like the nine-hole peg test or the Purdue Pegboard test assess the speed and accuracy of fine motor movements, crucial for tasks like buttoning clothes or writing.
- Sensation: I test sensation using light touch, pinprick, and temperature stimuli to identify any areas of numbness or altered sensation, which can impact function and safety.
- Functional tasks: I observe the patient performing ADLs relevant to their lifestyle, such as writing, eating, dressing, and working. This provides the most valuable insight into their true functional capacity.
Finally, I use standardized outcome measures, such as the DASH (Disabilities of the Arm, Shoulder and Hand) questionnaire, to quantify the impact of the injury on the patient’s daily life. Combining all these assessments gives me a clear picture of the patient’s functional capacity and guides treatment planning.
Q 9. Describe different types of hand assessments.
Hand assessments are diverse, tailored to the specific injury and goals. They range from simple clinical observations to complex quantitative measures. Here are a few examples:
- Range of Motion (ROM) Measurements: Using a goniometer to measure the angles of joint flexion and extension.
- Grip Strength Testing: Using a dynamometer to quantify the force a patient can exert with their grip.
- Two-Point Discrimination Testing: Assessing the patient’s ability to differentiate between two points of touch, indicating sensory recovery.
- Semmes-Weinstein Monofilament Testing: Measuring the ability to detect pressure, critical for assessing protective sensation.
- Pinch Strength Measurement: Assessing the strength of different pinch grips (tip, key, three-point).
- Functional Assessments: Observing the patient perform activities of daily living (ADLs), such as writing, buttoning, or eating.
- Sensory Testing: Evaluating various sensory modalities, including light touch, pain, temperature, and proprioception (awareness of joint position).
- Standardized Questionnaires: Using validated tools like the DASH (Disabilities of the Arm, Shoulder and Hand) or the QuickDASH to quantify the impact of the injury on the patient’s daily life.
The choice of assessments depends on the nature of the injury, the patient’s goals, and the stage of rehabilitation. For example, a patient with a simple laceration may only need ROM and functional assessments, while a patient with a complex fracture requiring surgery will need a more extensive evaluation, including sensory testing and standardized questionnaires.
Q 10. Explain the principles of wound healing in the hand.
Wound healing in the hand is a complex process involving several overlapping phases: inflammation, proliferation, and remodeling. The hand’s unique anatomy—with its intricate network of tendons, nerves, and blood vessels—influences this process significantly. Proper wound healing is crucial for restoring hand function.
- Inflammation (0-3 days): This initial phase is characterized by vasodilation, increased blood flow, and the migration of immune cells to the wound site. This is vital for clearing debris and initiating the repair process. Excessive inflammation can hinder healing.
- Proliferation (3-21 days): Fibroblasts migrate into the wound, producing collagen, which forms the foundation of the new tissue. New blood vessels (angiogenesis) form, providing oxygen and nutrients. Epithelial cells migrate to close the wound surface.
- Remodeling (21 days onwards): This lengthy phase involves the reorganization of collagen fibers, leading to increased tensile strength and scar tissue maturation. The scar will gradually fade and become less noticeable, though it will never regain the original skin’s elasticity.
Factors influencing hand wound healing include the type and severity of the injury, the patient’s overall health, the presence of infection, and the adequacy of blood supply. Adequate nutrition, proper wound care, and meticulous surgical technique are essential to optimize the healing process. For instance, ensuring proper alignment of bone fragments in a fracture is critical for optimal functional recovery. Similarly, meticulous surgical repair of tendons or nerves is paramount to prevent adhesions and restore function.
Q 11. What are the common complications of hand surgery?
Hand surgery carries several potential complications, some common and others less frequent. Early recognition and management are critical to minimizing their impact.
- Infection: A significant risk, particularly in wounds contaminated with foreign bodies. Infection can delay healing and cause serious complications, possibly requiring further surgery.
- Complex Regional Pain Syndrome (CRPS): A debilitating condition characterized by chronic pain, swelling, and changes in skin color and temperature. It’s often triggered by nerve injury.
- Stiffness and contractures: Scar tissue formation can restrict joint movement. Early mobilization and hand therapy are essential to prevent this.
- Nerve damage: Can result in numbness, tingling, or loss of sensation, impacting dexterity and function. Surgical repair may be necessary.
- Tendinitis: Inflammation of the tendons, commonly occurring after repetitive movements or injury.
- Adhesions: Abnormal attachments between tissues, restricting movement and potentially requiring surgical release.
- Delayed wound healing: Can be caused by various factors, including infection, poor blood supply, or underlying medical conditions.
- Degloving injuries: These severe injuries involve the separation of skin and subcutaneous tissue from underlying structures, often requiring extensive surgical intervention.
It’s vital to educate patients about these potential complications pre-operatively and provide careful postoperative monitoring and rehabilitation to minimize their occurrence.
Q 12. Describe your experience with different types of hand prosthetics.
My experience encompasses a range of hand prosthetics, from body-powered to myoelectric devices. The choice depends on individual needs and abilities.
- Body-Powered Prosthetics: These rely on the patient’s own muscles to operate the prosthetic hand. They are generally more affordable but require greater strength and coordination. I’ve worked with several patients using these, finding them particularly suitable for individuals with good upper limb strength and motivation.
- Myoelectric Prosthetics: These use electromyography (EMG) to detect muscle signals, controlling the prosthetic hand’s movements more naturally. I’ve seen remarkable improvements in dexterity and functionality with this type of prosthetic. However, they are more expensive and require a period of adaptation and training.
- Hybrid Systems: Combine aspects of both body-powered and myoelectric control, often offering a balance between cost, ease of use, and functionality.
For each patient, we conduct a thorough assessment to determine the most appropriate prosthetic type, considering factors such as the level of amputation, the patient’s physical capabilities, their lifestyle, and their budget. Patient education and ongoing support are crucial for successful prosthetic use.
One case that stands out was a young musician who lost his hand in an accident. After fitting him with a sophisticated myoelectric prosthetic specifically designed for fine motor control, he was able to return to playing his instrument. This highlights the power of assistive technology in restoring function and improving quality of life.
Q 13. How do you educate patients on post-operative hand care?
Patient education is a cornerstone of successful hand rehabilitation. I employ a multi-pronged approach to ensure patients understand their post-operative care and can manage their recovery effectively.
- Pre-operative Education: I discuss potential complications, expected recovery timelines, and the importance of adherence to the rehabilitation program. I also provide detailed instructions on wound care and pain management.
- Post-operative Instructions: I give clear, written instructions supplemented with verbal explanations and demonstrations. I provide contact information for any questions or concerns.
- Follow-up Appointments: Regular follow-up appointments are essential for monitoring progress, addressing any problems, and adjusting the treatment plan as needed.
- Therapeutic Exercises: I teach patients the specific exercises they need to perform, explaining the purpose and benefits of each. I also demonstrate correct techniques and address any difficulties.
- Scar Management: I explain the importance of scar massage and provide instructions on how to perform it correctly, aiding in preventing adhesions and improving cosmetic outcomes.
- Pain Management: I discuss appropriate pain management strategies, emphasizing the balance between pain control and mobilization.
I find that using visual aids, such as diagrams and videos, helps patients understand complex procedures and exercises better. Patient education is a continuous process. I always encourage questions and tailor my communication to the patient’s understanding level to ensure they feel empowered and confident in their recovery journey.
Q 14. What is your experience with different types of hand therapy modalities?
My experience encompasses a wide variety of hand therapy modalities, chosen based on the patient’s specific needs and the stage of their rehabilitation.
- Therapeutic Exercises: A cornerstone of hand therapy, involving range-of-motion exercises, strengthening exercises, and functional activities. I often tailor exercises to the patient’s specific needs and goals.
- Splinting and Orthotics: Custom-fabricated splints and orthoses are used to immobilize, support, or correct deformities, promoting healing and preventing contractures. The choice of splint depends on the type of injury and the phase of rehabilitation.
- Modalities: I use various modalities, such as ultrasound, electrical stimulation, and heat or cold therapy, to reduce pain and inflammation and promote tissue healing.
- Occupational Therapy: I often collaborate with occupational therapists who help patients adapt their daily routines and develop compensatory strategies to improve their functional abilities.
- Scar Management: Techniques like scar massage, silicone gel sheeting, and pressure garments help minimize scar tissue formation and improve the cosmetic outcome.
- Mirror Therapy: Used for pain relief and improving motor function, particularly effective in patients with CRPS.
The selection of modalities is always individualized. For example, a patient with a recent fracture might benefit primarily from immobilization and range-of-motion exercises, while a patient with chronic arthritis may benefit more from modalities to manage pain and inflammation and exercises to maintain joint mobility. A multimodal approach, combining several modalities, is often the most effective.
Q 15. How do you manage pain in patients with hand injuries?
Managing pain in hand injuries requires a multi-modal approach, tailored to the specific injury and patient. It’s crucial to understand the source of the pain – is it inflammatory, neuropathic, or nociceptive? This dictates the treatment strategy.
We start with conservative measures: rest, ice, compression, and elevation (RICE). Pharmacological interventions include non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or naproxen for inflammation, and analgesics like acetaminophen for mild to moderate pain. For more severe pain, we might consider opioids, but cautiously and with careful monitoring due to their addictive potential.
Beyond medication, we utilize physical modalities such as ultrasound, electrical stimulation (TENS), and iontophoresis to reduce inflammation and modulate pain signals. Occupational therapy plays a vital role in restoring function and managing pain through targeted exercises, splinting, and adaptive techniques. In some cases, we may refer patients to a pain management specialist for more advanced interventions, such as nerve blocks or interventional procedures.
For example, a patient with a carpal tunnel syndrome might initially benefit from a wrist splint, NSAIDs, and gentle hand exercises. If pain persists, we might consider a corticosteroid injection into the carpal tunnel. A patient with a complex fracture, on the other hand, might require a more aggressive approach, combining analgesics with surgical intervention and intensive rehabilitation.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. What are the ergonomic considerations for preventing hand injuries?
Ergonomic considerations are paramount in preventing hand injuries. Think of it as optimizing the workstation to fit the worker, not the other way around. The goal is to minimize repetitive movements, awkward postures, and excessive force.
- Proper posture: Maintaining a neutral wrist position is key. Avoid prolonged flexion or extension. Imagine your wrists are like delicate extensions of your forearms, needing support.
- Tool selection: Choose tools that fit the hand comfortably and reduce grip force. Power tools can significantly reduce strain.
- Workstation setup: Ensure the work surface is at the right height to avoid hunching or reaching. Proper lighting and organization minimize strain and fatigue.
- Regular breaks: Frequent short breaks allow for rest and reduce cumulative trauma. The ‘micro-breaks’ principle advocates for short, frequent pauses instead of one long break.
- Proper lifting techniques: Avoid lifting heavy objects with just your hands. Use your legs and core muscles.
For instance, a cashier who frequently scans items can benefit from a properly adjusted scanner height to minimize wrist strain. Similarly, a painter using a brush for long periods should take frequent breaks and consider using a tool with a larger handle to decrease grip force. These small changes can make a big difference in preventing cumulative trauma disorders.
Q 17. Describe your experience with treating complex regional pain syndrome (CRPS) of the hand.
Complex Regional Pain Syndrome (CRPS) of the hand is a debilitating condition characterized by chronic pain, swelling, changes in skin color and temperature, and limited range of motion. Treating CRPS requires a highly individualized and multidisciplinary approach.
My experience involves a combination of pharmacological and non-pharmacological interventions. Pharmacological management may include NSAIDs, opioids (used cautiously), antidepressants (like amitriptyline), and anticonvulsants (like gabapentin) to manage neuropathic pain.
Non-pharmacological interventions are crucial and often form the backbone of treatment. These include:
- Physical therapy: Focused on restoring range of motion, strength, and function through carefully graded exercises and modalities.
- Occupational therapy: To adapt activities of daily living and prevent further injury.
- Psychological support: Addressing the emotional impact of chronic pain is vital.
- Sympathetic nerve blocks: In some cases, nerve blocks can temporarily alleviate symptoms and provide diagnostic information.
- Mirror therapy: A novel technique using visual feedback to reduce pain and improve function.
One particularly challenging case involved a young woman with CRPS after a wrist fracture. We implemented a comprehensive program including physical and occupational therapy, mirror therapy, and a carefully titrated regimen of gabapentin and amitriptyline. While complete resolution is not always possible, we achieved significant pain reduction and improved functional capacity.
Q 18. How do you assess and treat trigger finger?
Trigger finger, or stenosing tenosynovitis, is characterized by a catching or locking sensation in a finger or thumb. Assessment involves a thorough history, focusing on the onset, location, and nature of the symptoms. Physical examination includes palpating the affected tendon for nodules or thickening and observing the characteristic ‘triggering’ or locking during flexion and extension.
Treatment starts conservatively. This includes:
- Splinting: To immobilize the affected finger and prevent further irritation.
- Corticosteroid injection: Injected directly into the tendon sheath, this reduces inflammation and can provide significant relief.
- Hand therapy: Exercises to improve range of motion and tendon gliding.
Surgical intervention is considered if conservative treatment fails. The procedure involves releasing the constricted tendon sheath, allowing for smooth tendon movement. Post-operative hand therapy is essential for optimal recovery.
For example, a patient presenting with a trigger thumb might initially receive a corticosteroid injection. If symptoms recur or don’t improve, surgery may be recommended. Post-surgical rehabilitation focuses on gentle range of motion exercises to prevent stiffness and regain full function.
Q 19. What is your experience with treating rheumatoid arthritis of the hand?
Rheumatoid arthritis (RA) of the hand is a chronic inflammatory disease affecting the joints, leading to pain, swelling, stiffness, and ultimately, deformity. Treatment aims to control inflammation, manage pain, and preserve hand function.
Management is multifaceted:
- Pharmacological therapy: Disease-modifying antirheumatic drugs (DMARDs) such as methotrexate, sulfasalazine, and biologics are used to slow disease progression. NSAIDs and analgesics are used for pain relief.
- Hand therapy: Crucial for maintaining range of motion, strength, and functional ability through customized exercises, splinting, and joint protection techniques.
- Surgical intervention: In advanced cases, surgery may be necessary to correct deformities, such as synovectomy (removal of inflamed synovium) or joint replacement.
I have extensive experience managing RA patients. One particular case involved a patient with severe ulnar deviation of the fingers and significant pain. We initiated DMARD therapy and started intensive hand therapy. She participated in a program combining strengthening and range-of-motion exercises with splinting to support the joints. We saw a significant reduction in inflammation and pain and improved her ability to perform daily tasks.
Q 20. Explain the biomechanics of the hand.
The hand’s biomechanics are complex, involving intricate interactions between bones, muscles, tendons, ligaments, and nerves. The 27 bones of the hand, including the carpals, metacarpals, and phalanges, are arranged to provide a remarkable range of motion and dexterity.
Key aspects of hand biomechanics include:
- Articulations: The hand features numerous joints, allowing for flexion, extension, abduction, adduction, and opposition movements. The carpometacarpal joint of the thumb, for example, enables the unique opposition movement that is crucial for grasping.
- Muscle actions: Intrinsic muscles within the hand provide fine motor control, while extrinsic muscles in the forearm exert more powerful actions.
- Tendons: These transmit forces from muscles to bones, enabling precise finger movements. Tendons also act as shock absorbers, reducing the force of impacts.
- Ligaments: These provide stability to the joints, preventing excessive movement and injury.
- Arches: The hand’s architecture incorporates three arches – longitudinal, transverse, and distal – which contribute to shock absorption and stability during weight-bearing activities.
Understanding these intricate biomechanical relationships is critical in diagnosing and treating hand injuries. For instance, a fracture of a specific carpal bone can have significant implications for the hand’s overall function and require a treatment plan tailored to its biomechanical role.
Q 21. Describe different types of surgical approaches to the hand.
Surgical approaches to the hand are highly specialized and vary depending on the specific condition. They can range from minimally invasive procedures to complex reconstructive surgeries.
Examples include:
- Open reduction and internal fixation (ORIF): Used to repair fractures, this involves surgically exposing the fracture site, aligning the bone fragments, and stabilizing them with plates, screws, or pins.
- Arthrodesis: This involves surgically fusing two or more bones together, primarily used for severe arthritis or unstable joints. It sacrifices some mobility for stability.
- Arthroplasty: A joint replacement surgery, which involves replacing a damaged joint with a prosthetic implant. This is common in the case of severe rheumatoid arthritis.
- Tendon repair: Used to repair severed or damaged tendons, often involving microsurgery techniques for very fine tendons.
- Nerve repair: Used to reconnect damaged nerves, crucial in cases of nerve injuries.
- Carpal tunnel release: A minimally invasive procedure to relieve pressure on the median nerve in the carpal tunnel.
The choice of surgical approach depends on factors such as the nature and severity of the injury, the patient’s overall health, and the surgeon’s expertise. Post-operative rehabilitation is critical regardless of the surgical technique, to restore optimal hand function.
Q 22. How do you determine the appropriate treatment plan for a specific hand injury?
Developing a treatment plan for a hand injury requires a systematic approach. It begins with a thorough evaluation, encompassing a detailed patient history, a comprehensive physical examination, and appropriate imaging studies (X-rays, MRI, CT scans). The examination assesses range of motion, strength, sensation, and the presence of any deformities or instability.
For example, a patient presenting with a suspected carpal tunnel syndrome will undergo a neurological examination focusing on median nerve function, including sensory testing and thenar muscle strength assessment. Imaging might not be necessary initially, but if symptoms are severe or there’s suspicion of other pathologies, an ultrasound or MRI would be ordered.
Once the diagnosis is established, I tailor the treatment plan to the specific injury and the patient’s individual needs and goals. This may include conservative management (such as splinting, medication, and physical therapy) or surgical intervention, depending on the severity and type of injury. The plan is always discussed collaboratively with the patient to ensure they understand their condition and the proposed course of treatment, setting realistic expectations for recovery.
Q 23. What are the latest advancements in hand surgery or therapy?
Hand surgery and therapy are constantly evolving. Recent advancements include minimally invasive techniques, such as arthroscopic surgery, which allows for smaller incisions, less trauma, and faster recovery. For example, arthroscopy can be used to repair ligament tears in the wrist or treat carpal tunnel syndrome.
In the realm of therapy, advancements in robotics and virtual reality are improving rehabilitation outcomes. Robotic devices provide precise, repetitive exercises to enhance dexterity and strength, while VR technology allows for engaging and motivating therapeutic sessions. Furthermore, the use of advanced biomaterials in reconstructive surgery, such as biodegradable implants and tissue-engineered grafts, is minimizing complications and improving healing times. Finally, there’s been significant progress in nerve regeneration techniques, offering hope to patients with severe nerve injuries.
Q 24. Describe your experience with different types of skin grafts used in hand reconstruction.
My experience encompasses a wide range of skin grafts used in hand reconstruction. The choice of graft depends on the size and location of the defect, the quality of the recipient site, and the patient’s overall health.
- Full-thickness skin grafts provide excellent cosmetic results but have limited availability, requiring a separate donor site. I have used these extensively for larger defects, prioritizing areas with less visible scarring, like the inner thigh.
- Split-thickness skin grafts are more readily available but can result in less aesthetically pleasing scarring. They are often preferred for smaller defects, where the donor site’s cosmetic outcome is less crucial.
- Composite grafts, which include skin and underlying structures (like cartilage or fat), are used for more complex reconstructions involving multiple tissue layers. I’ve successfully employed these in cases of severe fingertip injuries, restoring both skin cover and structural integrity.
- Allo- and xenografts are utilized as temporary wound coverings until autologous grafts can be harvested. While not ideal, they play a crucial role in managing critically injured hands.
The success of any skin graft depends on meticulous surgical technique, precise wound bed preparation, and optimal post-operative care, including meticulous wound dressing and monitoring for complications such as infection or graft failure.
Q 25. How do you handle challenging patient interactions?
Handling challenging patient interactions requires empathy, active listening, and clear communication. I always prioritize understanding the patient’s perspective, even when their concerns might seem unreasonable.
For instance, a patient might be frustrated with the slow pace of their recovery. Instead of dismissing their concerns, I acknowledge their feelings, explain the physiological reasons behind the recovery timeline, and collaboratively set realistic goals. I also involve family members in discussions where appropriate, fostering a supportive environment. If communication breakdowns persist, I seek consultation from colleagues or mental health professionals to ensure the patient receives comprehensive care. Ultimately, building trust and rapport is crucial in navigating challenging interactions and achieving positive treatment outcomes.
Q 26. What are your strengths and weaknesses in relation to hand technique?
My strengths lie in my meticulous surgical technique and my ability to perform complex microsurgical procedures, particularly those involving nerve repair and tendon reconstruction. I’m adept at adapting my surgical approach to accommodate individual patient anatomy and the specifics of each injury. My proficiency in minimally invasive techniques and advanced imaging interpretation also contribute significantly to my practice.
A potential area for improvement is enhancing my familiarity with the latest advancements in bioprinting and 3D-printed prosthetics. While I’m aware of these technologies, further training will strengthen my ability to offer patients the full spectrum of treatment options.
Q 27. Describe a time you had to adapt your approach to a patient with unique needs.
I recall a patient with severe burns involving the entire dorsal aspect of his hand and significant tendon damage. Conventional techniques were unlikely to restore full function. Rather than relying solely on established methods, I collaborated with a plastic surgeon and a rehabilitation specialist to devise a personalized treatment plan.
We employed a combination of surgical debridement, multiple staged skin grafts from various donor sites, and innovative tendon grafting techniques. Post-operatively, intensive rehabilitation including specialized occupational therapy with a focus on scar tissue management and regaining range of motion was implemented. This multidisciplinary, adaptable approach resulted in surprisingly good functional recovery for the patient, exceeding initial expectations. This experience highlighted the importance of flexibility, collaboration, and a willingness to explore unconventional solutions when confronted with unique patient needs.
Q 28. How do you stay current with the latest advancements in hand therapy and surgery?
Staying current in hand therapy and surgery requires continuous professional development. I actively participate in continuing medical education (CME) courses, attend national and international conferences, and regularly review peer-reviewed journals and relevant medical publications. Membership in professional organizations such as the American Society for Surgery of the Hand (ASSH) provides access to the latest research and opportunities for collaboration with other specialists.
Furthermore, I maintain a strong network with colleagues and regularly engage in case discussions and knowledge sharing. These diverse avenues ensure I remain at the forefront of advancements, enabling me to provide my patients with the most up-to-date and effective care.
Key Topics to Learn for Hand Technique Interview
- Grip Strength and Control: Understanding different grip types (power, precision, pinch), their applications, and how to optimize grip for various tasks and tools.
- Dexterity and Manipulation: Exploring fine motor skills, hand-eye coordination, and the ability to perform intricate manipulations with speed and accuracy. Consider practical applications like assembling small components or delicate surgery simulations.
- Ergonomics and Safety: Analyzing hand posture, movement efficiency, and preventative measures against repetitive strain injuries (RSI). This includes understanding the impact of tool design and workstation setup.
- Hand Tool Proficiency: Demonstrating knowledge and practical experience with various hand tools relevant to the specific job (e.g., precision screwdrivers, specialized surgical instruments). Consider scenarios where tool selection impacts efficiency and safety.
- Troubleshooting and Problem-Solving: Analyzing scenarios where hand technique may lead to errors or inefficiencies and demonstrating the ability to identify and correct these issues. This could involve diagnosing poor grip, suggesting ergonomic improvements, or adapting technique for challenging tasks.
- Material Knowledge: Understanding how different materials (e.g., metals, plastics, textiles) impact hand technique requirements and the need for adjustments in approach.
Next Steps
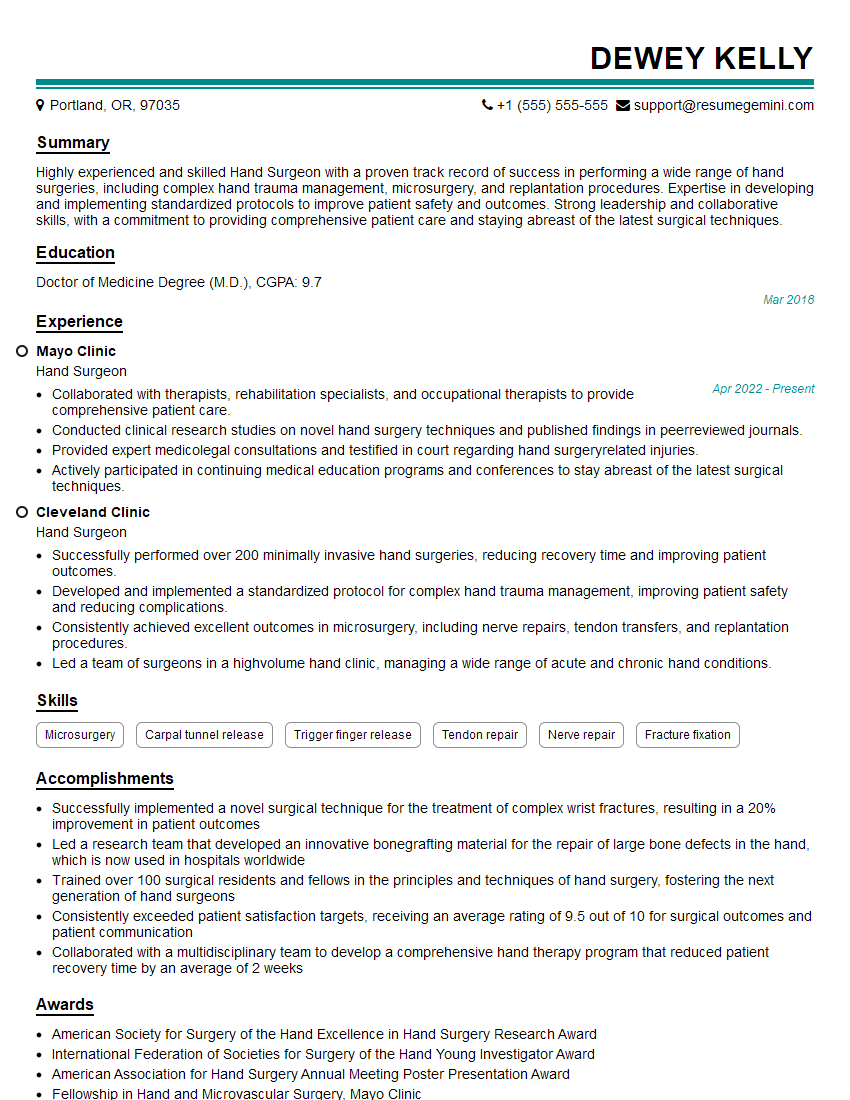
Mastering hand technique is crucial for career advancement in many fields, significantly impacting efficiency, precision, and safety. A strong understanding of these principles demonstrates professionalism and a commitment to excellence. To maximize your job prospects, it’s vital to create an ATS-friendly resume that effectively highlights your skills and experience. ResumeGemini is a trusted resource to help you build a professional and impactful resume that catches the eye of recruiters. We offer examples of resumes tailored specifically to Hand Technique roles to help you get started.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
hello,
Our consultant firm based in the USA and our client are interested in your products.
Could you provide your company brochure and respond from your official email id (if different from the current in use), so i can send you the client’s requirement.
Payment before production.
I await your answer.
Regards,
MrSmith
hello,
Our consultant firm based in the USA and our client are interested in your products.
Could you provide your company brochure and respond from your official email id (if different from the current in use), so i can send you the client’s requirement.
Payment before production.
I await your answer.
Regards,
MrSmith
These apartments are so amazing, posting them online would break the algorithm.
https://bit.ly/Lovely2BedsApartmentHudsonYards
Reach out at [email protected] and let’s get started!
Take a look at this stunning 2-bedroom apartment perfectly situated NYC’s coveted Hudson Yards!
https://bit.ly/Lovely2BedsApartmentHudsonYards
Live Rent Free!
https://bit.ly/LiveRentFREE
Interesting Article, I liked the depth of knowledge you’ve shared.
Helpful, thanks for sharing.
Hi, I represent a social media marketing agency and liked your blog
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?