Interviews are more than just a Q&A session—they’re a chance to prove your worth. This blog dives into essential Kidney Transplantation interview questions and expert tips to help you align your answers with what hiring managers are looking for. Start preparing to shine!
Questions Asked in Kidney Transplantation Interview
Q 1. Describe the process of kidney allocation according to UNOS guidelines.
Kidney allocation in the United States is governed by the United Network for Organ Sharing (UNOS), a non-profit organization that manages the Organ Procurement and Transplantation Network (OPTN). The system prioritizes recipients based on several factors, aiming for the fairest and most efficient distribution of scarce organs. It’s a complex process, but the core principle is to give the organ to the patient who will benefit most and has the highest chance of a successful transplant.
The process involves a points-based system that considers medical urgency (how sick the patient is), waiting time, tissue compatibility (HLA matching – discussed in the next question), and geographic proximity to the donor. Patients are listed on a waiting list, and when a suitable donor organ becomes available, the OPTN computer system uses this algorithm to identify the best match. Factors like blood type and HLA compatibility are crucial, but the system balances these with the urgency of the recipient’s need. Imagine it like a complex matching puzzle where many pieces must fit together to find the optimal solution. For example, a patient with a very high Panel Reactive Antibody (PRA) percentage, indicating a heightened risk of rejection, might receive lower priority, unless a suitable organ with limited HLA mismatch is available. Similarly, a patient with end-stage renal disease (ESRD) whose condition is rapidly deteriorating will receive higher priority, even if their HLA match is not perfect.
Q 2. Explain the role of HLA matching in kidney transplantation.
Human Leukocyte Antigens (HLA) are proteins found on the surface of most cells, acting as identification markers. In kidney transplantation, HLA matching between the donor and recipient is critically important because the recipient’s immune system can recognize the donor kidney as foreign tissue, triggering an immune response (rejection). Close HLA matching reduces the risk of rejection.
The closer the match, the lower the likelihood of rejection and the less intense the immunosuppression required. HLA matching involves examining specific HLA genes – HLA-A, HLA-B, and HLA-DR are the most important. A perfect match is rare, but a good match, minimizing the disparity between donor and recipient HLA types, significantly improves transplant success rates. Think of it like a lock and key: the better the key (donor HLA) fits the lock (recipient HLA), the more smoothly the transplanted kidney will function. Partial mismatches can be tolerated, but they necessitate a more rigorous immunosuppressive regimen to manage the risk of rejection.
Q 3. What are the common immunosuppressant medications used post-transplant, and their potential side effects?
Immunosuppressant drugs are essential after kidney transplantation to prevent rejection. These medications suppress the immune system’s ability to attack the foreign kidney. Several classes of drugs are commonly used in combination.
- Calcineurin inhibitors: Tacrolimus (Prograf) and cyclosporine (Sandimmune, Neoral) are potent immunosuppressants. Side effects can include nephrotoxicity (kidney damage), hypertension (high blood pressure), diabetes, and neurotoxicity (nervous system problems).
- Antimetabolites: Mycophenolate mofetil (CellCept) and azathioprine (Imuran) interfere with DNA synthesis, reducing immune cell proliferation. Side effects can include gastrointestinal problems, bone marrow suppression, and increased risk of infection.
- mTOR inhibitors: Sirolimus (Rapamune) and everolimus (Zortress) target the mTOR pathway, further suppressing immune responses. Side effects can include hyperlipidemia (high cholesterol), mouth sores, and impaired wound healing.
- Corticosteroids: Prednisone is often used to reduce inflammation and suppress immune function initially. Long-term use can lead to osteoporosis, increased risk of infection, weight gain, and hyperglycemia.
The specific drugs and dosages are carefully tailored to each patient’s needs and risk profile. Regular blood tests are necessary to monitor drug levels and side effects. It’s a delicate balance: enough immunosuppression to prevent rejection but not so much as to cause debilitating side effects.
Q 4. How do you manage acute rejection episodes in kidney transplant recipients?
Acute rejection is a serious complication after kidney transplantation, characterized by the immune system attacking the transplanted kidney. Early detection is crucial. Symptoms can include decreased urine output, swelling, fever, pain at the transplant site, and rising creatinine levels (indicator of kidney function).
Management involves a rapid increase in immunosuppressive medication dosage, usually including corticosteroids such as methylprednisolone, given intravenously. Close monitoring of kidney function, through blood tests and urine analysis, is essential. In severe cases, additional immunosuppressants may be added, and in rare cases, surgical intervention might be considered. The goal is to rapidly suppress the immune response and preserve kidney function. The frequency and intensity of rejection episodes can vary; some patients experience several, while others remain rejection-free. Each episode is carefully evaluated to determine the optimal course of treatment and to adjust long-term immunosuppressive therapy.
Q 5. Detail the pre-operative assessment for a potential kidney transplant recipient.
Pre-transplant evaluation is a comprehensive process to assess the recipient’s suitability for transplantation. It involves a multidisciplinary team including nephrologists, surgeons, cardiologists, and other specialists.
- Medical History and Physical Examination: A thorough evaluation of the patient’s overall health, including cardiovascular health, liver function, and other organ systems.
- Blood Tests: Comprehensive blood work to assess kidney function, blood type, HLA typing, and infectious diseases (hepatitis B and C, HIV, CMV).
- Imaging Studies: Ultrasound, CT scans, or MRI to evaluate the vascular system and potential sites for kidney placement.
- Psychological Evaluation: To assess the patient’s readiness and ability to cope with the demands of transplantation and long-term immunosuppression.
- Tissue Typing (HLA): To determine the best possible match with a potential donor.
- Assessment of Comorbidities: Evaluation of other health issues, such as diabetes, hypertension, and cardiovascular disease, which can significantly impact the success of the transplant.
This extensive evaluation helps determine the patient’s suitability for transplantation, identifies potential risks, and optimizes the pre-operative strategy. It’s like a meticulous preparation for a major undertaking; every detail matters.
Q 6. What are the indicators for kidney transplant versus continued dialysis?
The decision to proceed with kidney transplantation versus continued dialysis is complex, depending on several factors.
- Patient’s Health Status: The overall health of the recipient, including the presence of other medical conditions that could affect transplant outcome. Individuals with severely compromised cardiovascular health or other severe comorbidities might be better suited to remain on dialysis.
- Quality of Life: Dialysis, while life-sustaining, significantly impacts quality of life. Transplantation offers the potential for improved health and freedom from the limitations of dialysis.
- Access to Transplantation: Geographical location, availability of organs, and waiting list times play a role. Transplant programs might prioritize patients with severe disease and comorbidities.
- Social Support System: Recipients require significant support for post-transplant care, medication adherence, and lifestyle adjustments.
- Financial Considerations: Transplantation involves significant costs, including surgery, immunosuppressive medications, and long-term monitoring. While insurance coverage can help alleviate some costs, the financial burden should be assessed.
The decision is made collaboratively between the patient, nephrologist, transplant team, and family. It’s a personal decision that should consider the potential benefits and risks of both options.
Q 7. Explain the surgical techniques used in kidney transplantation.
Kidney transplantation is usually performed through an open surgical procedure, though minimally invasive techniques are emerging. The goal is to place the donor kidney in the recipient’s abdomen in such a way that blood supply and drainage is efficient and functional.
The most common technique involves placing the kidney in the iliac fossa (the area in the lower abdomen, near the hip bone). A major artery and vein in the lower abdomen are surgically connected to the donor kidney’s artery and vein. The donor ureter (the tube that carries urine from the kidney to the bladder) is connected to the recipient’s bladder. The surgical approach varies depending on whether it’s a living-donor or deceased-donor transplant. Living donor transplants often use laparoscopic techniques, minimizing the invasiveness and reducing recovery times. In either case, precise microsurgical techniques are used for vascular anastomosis (connecting blood vessels) to ensure proper blood flow to the new kidney. Post-operatively, the patient is monitored closely for complications such as bleeding, infection, rejection, and urine leakage. The process is complex and requires a highly skilled surgical team.
Q 8. How do you monitor graft function post-transplant?
Monitoring graft function after a kidney transplant is crucial for early detection of complications and ensuring long-term success. We employ several key methods:
- Serum Creatinine and eGFR (estimated Glomerular Filtration Rate): These are the cornerstone of graft function assessment. Creatinine, a waste product filtered by the kidneys, rises in the blood when kidney function declines. eGFR calculates how well the kidneys are filtering blood, providing a more comprehensive picture than creatinine alone. Regular blood tests monitoring these values are essential, typically several times a week initially, then tapering to monthly or less frequent intervals depending on stability.
- Urine Output: Adequate urine production indicates the transplanted kidney is functioning. We closely monitor the volume and characteristics of urine. Low urine output can signal problems like rejection or obstruction.
- Ultrasound: Regular ultrasounds help visualize the kidney’s size, blood flow, and detect any structural abnormalities, such as blockages or fluid collections.
- Kidney Biopsy: In cases of suspected rejection or declining graft function, a kidney biopsy may be necessary. This involves taking a small tissue sample for microscopic examination, providing a detailed assessment of the kidney’s health and identifying the cause of any problems.
- Blood Pressure Monitoring: Careful blood pressure monitoring is essential as hypertension can significantly impact graft survival. Well-controlled blood pressure is crucial for long-term graft success.
For example, a patient with a consistently rising serum creatinine and decreasing eGFR despite medication adjustments might warrant a kidney biopsy to investigate potential rejection or other complications.
Q 9. Describe the management of post-transplant complications like infection or bleeding.
Post-transplant complications like infections and bleeding require prompt and aggressive management. Infections are a major concern due to the immunosuppression required to prevent rejection. We typically:
- Rapid Identification and Treatment: Any signs of infection (fever, chills, localized inflammation) are investigated immediately with blood cultures, urine cultures, and imaging as needed. Treatment involves broad-spectrum antibiotics tailored to the specific organism identified.
- Prophylactic Antibiotics: Prophylactic antibiotics may be used perioperatively and in certain high-risk situations to prevent infections.
- Antiviral and Antifungal Medications: As needed, depending on the infection.
Bleeding complications can occur at the surgical site or internally. Management strategies include:
- Close Monitoring: Close observation of vital signs and surgical site for any signs of bleeding.
- Blood Transfusions: If significant blood loss occurs.
- Surgical Intervention: In some cases, surgery may be needed to control bleeding.
- Medication Adjustments: Careful adjustment of anticoagulation medications (if prescribed).
For instance, a patient presenting with fever and leukocytosis (high white blood cell count) post-transplant would undergo a thorough investigation to identify and treat the infection. Similarly, a patient with a decreasing hemoglobin level and evidence of internal bleeding would require immediate intervention, possibly including blood transfusion and surgical exploration.
Q 10. What are the long-term risks associated with kidney transplantation?
Kidney transplantation offers a significant improvement in quality of life but carries long-term risks. These include:
- Graft Rejection: The body’s immune system may attack the transplanted kidney, potentially leading to graft failure. Immunosuppressive medications help prevent rejection but carry their own risks.
- Infection: Immunosuppression increases susceptibility to infections, ranging from minor illnesses to life-threatening sepsis.
- Malignancy: Immunosuppressive drugs increase the risk of certain cancers, particularly skin cancers and lymphomas.
- Cardiovascular Disease: Transplant recipients have a higher risk of heart disease, hypertension, and stroke.
- Diabetes: The risk of developing or worsening diabetes mellitus is increased.
- Drug-induced Nephrotoxicity: Some immunosuppressants can cause damage to the kidneys over time.
- Chronic Kidney Disease Recurrence: If the original kidney disease was chronic, it might recur in the transplanted kidney.
The long-term risk profile highlights the importance of careful monitoring and managing associated conditions like hypertension and diabetes, as well as adherence to the immunosuppression regimen.
Q 11. How do you counsel patients about the risks and benefits of transplantation?
Counseling patients about transplantation is a crucial part of the process. We engage in a shared decision-making approach, thoroughly discussing the:
- Benefits: Improved quality of life, increased life expectancy, independence from dialysis.
- Risks: As detailed above, including rejection, infection, malignancy, cardiovascular disease, and the need for lifelong immunosuppression.
- Lifestyle Changes: Adherence to medication regimen, regular follow-up appointments, dietary restrictions, and lifestyle adjustments (e.g., avoiding crowds to minimize infection risk).
- Financial Implications: Costs associated with the transplant procedure, medications, and ongoing care.
- Alternative Options: Dialysis remains a viable option, and we discuss its advantages and disadvantages relative to transplantation.
We use clear and simple language, avoiding medical jargon, and tailor our approach to the patient’s individual circumstances, educational level, and emotional state. We encourage questions and provide opportunities for the patient and family to discuss their concerns. For example, if a patient expresses anxieties about potential side effects of immunosuppressive medications, we provide a detailed explanation of each medication’s benefits, risks, and potential side effects, offering strategies for managing these side effects.
Q 12. Explain the role of a transplant coordinator in the process.
The transplant coordinator plays a vital role, acting as the central point of contact and providing comprehensive support throughout the entire transplantation process. Their responsibilities include:
- Patient Education and Counseling: Educating patients and families about the process, risks, benefits, and post-transplant care.
- Pre-transplant Assessment and Workup: Coordinating various tests and evaluations necessary before transplantation.
- Organ Procurement and Allocation: Working with the transplant team to identify suitable donors and manage the organ allocation process.
- Scheduling and Logistics: Coordinating appointments, hospital admissions, and post-transplant care.
- Medication Management and Education: Assisting patients in understanding and managing their medication regimen.
- Post-transplant Monitoring and Support: Providing ongoing support to patients and families after the transplant.
- Advocacy and Resource Coordination: Connecting patients with necessary resources, such as financial assistance programs or support groups.
In essence, the transplant coordinator ensures a seamless and well-coordinated process, minimizing stress for the patient and their family and maximizing the chance of a successful transplant.
Q 13. Describe the process of living donor kidney transplantation.
Living donor kidney transplantation involves a healthy individual donating one of their kidneys to a recipient. The process involves several crucial steps:
- Extensive Evaluation of Both Donor and Recipient: Both undergo rigorous medical and psychological evaluations to ensure compatibility and suitability. The donor’s health and the recipient’s overall health and suitability are assessed.
- HLA Typing: Human Leukocyte Antigen (HLA) typing is performed to determine the compatibility between the donor and recipient’s immune systems. Close matching reduces the risk of rejection.
- Surgical Procedure: Laparoscopic or open surgery is performed to remove one of the donor’s kidneys. The recipient undergoes surgery to receive the transplanted kidney.
- Post-Operative Care: Both donor and recipient require close monitoring and post-operative care.
- Ethical Considerations: Strict ethical guidelines and regulations ensure the donor’s well-being and informed consent.
The living donor transplantation process is more complex than deceased donor transplantation, requiring careful consideration of the donor’s health and well-being. For example, a thorough assessment ensures the donor has sufficient kidney function remaining to maintain their health post-donation.
Q 14. How do you manage a patient experiencing delayed graft function?
Delayed graft function (DGF) refers to the transplanted kidney’s inability to function immediately after transplantation. It’s a significant complication requiring prompt management. We typically approach DGF with:
- Intensive Monitoring: Close monitoring of serum creatinine, eGFR, urine output, and electrolytes.
- Supportive Care: Dialysis may be necessary to support the patient’s renal function until the transplanted kidney begins to function adequately. Fluid and electrolyte balance must be closely controlled.
- Investigation of Cause: We investigate potential causes, such as ischemia-reperfusion injury (damage during the transplant process), acute tubular necrosis (damage to the kidney tubules), or rejection. This might involve further investigations like kidney biopsy.
- Medication Adjustments: Careful adjustment of immunosuppressants to minimize rejection. If the cause is related to tubular injury, certain medications may help with the healing process.
- Close Follow-Up: Close monitoring of the kidney’s recovery, with frequent creatinine and eGFR measurements.
Successful management of DGF hinges on early detection, appropriate supportive care, and addressing the underlying cause. The prognosis for recovery varies depending on the severity of DGF and the underlying etiology. For example, if a patient with DGF presents with high creatinine and low urine output, we initiate dialysis immediately while we further investigate the underlying cause, which may necessitate a kidney biopsy to rule out rejection.
Q 15. What are the ethical considerations related to kidney transplantation?
Kidney transplantation, while a life-saving procedure, presents a complex web of ethical considerations. The most prominent is the allocation of scarce organs. Determining who receives a transplant involves balancing medical urgency, compatibility, and the potential for successful long-term outcomes. This often leads to difficult decisions, particularly when multiple patients are in need of a transplant.
Another key area is informed consent. Patients must fully understand the risks, benefits, and potential complications of transplantation, including the need for lifelong immunosuppression and the possibility of rejection. They must also be mentally capable of making such a significant decision.
Furthermore, the source of the kidney raises ethical questions. Live donation necessitates careful evaluation of the donor’s health and well-being, ensuring they are fully informed and not coerced. Organ procurement from deceased donors involves intricate legal and ethical frameworks to guarantee appropriate consent and prevent exploitation.
Finally, issues of equity and access arise. Disparities in access to transplantation based on socioeconomic status, race, or geographic location are a major concern, highlighting the need for just and equitable organ allocation systems.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Discuss the impact of comorbidities on kidney transplantation outcomes.
Comorbidities, or co-existing medical conditions, significantly impact kidney transplant outcomes. These conditions can increase the risk of complications, affect graft survival, and reduce the overall quality of life post-transplant. For example, diabetes increases the risk of both early and late graft failure. Patients with diabetes often experience accelerated atherosclerosis, increasing their chances of cardiovascular events. This can damage the transplanted kidney, even if the initial transplant was successful.
Hypertension, another common comorbidity, also negatively influences transplant success. Poorly controlled blood pressure can accelerate damage to the newly transplanted kidney and increase the risk of cardiovascular disease. Similarly, heart failure or chronic lung disease can lead to increased post-operative mortality and morbidity, creating additional challenges in the recovery process.
The presence of comorbidities usually requires a more intensive approach to pre- and post-transplant management, often involving multiple specialists. Careful assessment and management of these conditions before and after transplantation are critical to improving overall outcomes. This highlights the importance of a multidisciplinary team approach to transplantation.
Q 17. How do you assess the psychosocial well-being of transplant candidates?
Assessing the psychosocial well-being of transplant candidates is crucial for successful transplantation. It’s not just about physical health; a candidate’s emotional and mental state significantly impacts their ability to adhere to the rigorous post-transplant regimen and cope with the challenges of living with a transplanted organ.
Assessment usually involves several methods, including psychological interviews, questionnaires to assess depression, anxiety, and coping mechanisms, and social worker evaluations to determine support systems and adherence capacity. We look for factors like a candidate’s understanding of the treatment process, their commitment to following medications and lifestyle changes, and their access to adequate support networks (family, friends, social services).
A comprehensive evaluation identifies potential risks, such as non-compliance with medication or a lack of social support, which may compromise transplant success. Addressing these issues beforehand, through counseling or support services, enhances the likelihood of positive outcomes both physically and mentally. For instance, a candidate with a history of poor medication adherence may be offered strategies to improve adherence before transplant.
Q 18. Explain the role of immunosuppression in preventing rejection.
Immunosuppression is the cornerstone of preventing transplant rejection. The transplanted kidney is recognized by the recipient’s immune system as foreign tissue, triggering an immune response aimed at its destruction. Immunosuppressive drugs work by suppressing the activity of the immune system, reducing the likelihood of this rejection.
These drugs act in different ways, targeting various components of the immune system. Some drugs, like calcineurin inhibitors (e.g., cyclosporine, tacrolimus), block the activation of T cells, which are key players in the immune response. Others, such as corticosteroids (e.g., prednisone), have broader anti-inflammatory effects. Still others, like mTOR inhibitors (e.g., sirolimus, everolimus), inhibit the proliferation of T cells.
The specific regimen of immunosuppressants varies depending on the individual patient, their medical history, and the risk of rejection. The goal is to find the right balance: suppressing the immune system enough to prevent rejection but not so much that it compromises the body’s ability to fight infections. This delicate balance is a crucial aspect of post-transplant care, requiring careful monitoring and adjustments.
Q 19. Describe different types of kidney transplant rejection.
Kidney transplant rejection can be categorized into several types, primarily based on timing and the mechanisms involved.
- Hyperacute rejection: This is a rare but devastating form of rejection that occurs within minutes or hours of transplantation. It’s caused by pre-existing antibodies in the recipient’s blood that immediately attack the transplanted kidney.
- Acute rejection: This is the most common type, typically occurring within the first few months post-transplant. It is an immune response mediated by T cells and other immune cells attacking the transplanted kidney, leading to inflammation and damage.
- Chronic rejection: This occurs gradually over months or years, characterized by progressive scarring and fibrosis of the transplanted kidney, eventually leading to graft failure. It’s often a complex interplay of immune and non-immune mechanisms.
The types of rejection may overlap, and the clinical presentation varies. Diagnosis requires careful evaluation using clinical symptoms, blood tests (measuring creatinine levels and immune markers), and sometimes kidney biopsy.
Q 20. What are the early warning signs of transplant rejection?
Early warning signs of transplant rejection are often subtle and can easily be overlooked. They may include:
- Decreased urine output: A sudden reduction in the amount of urine produced can indicate that the transplanted kidney is not functioning properly.
- Weight gain: Fluid retention is a common sign of rejection and can lead to significant weight gain.
- Increased blood pressure: Rejection can cause hypertension as the kidney struggles to function effectively.
- Fever: While not always indicative of rejection, a fever can signal inflammation in the transplanted kidney.
- General malaise: Feeling unwell, fatigued, or experiencing nausea and vomiting are also possible indicators.
It’s essential to emphasize that any of these symptoms, especially if occurring in combination, warrants immediate medical attention. Prompt diagnosis and treatment of rejection are crucial for preserving graft function. A change in kidney function tests, such as rising serum creatinine, is a key laboratory indicator needing immediate attention.
Q 21. What are the common causes of graft failure?
Graft failure, the loss of function of the transplanted kidney, can stem from several factors.
- Rejection: As discussed earlier, both acute and chronic rejection are major causes of graft failure.
- Infection: Immunosuppressive drugs, while necessary to prevent rejection, leave the recipient vulnerable to infections, which can severely damage the transplanted kidney.
- Recurrence of the original kidney disease: In some cases, the underlying disease that led to kidney failure can recur in the transplanted kidney, leading to its eventual failure.
- Medication toxicity: Some immunosuppressive drugs have side effects that can damage the kidneys over time.
- Cardiovascular disease: Patients with kidney disease are at increased risk of cardiovascular events, which can impact graft survival.
- Non-compliance with medication: Failure to consistently take immunosuppressants significantly increases the risk of rejection and subsequent graft failure.
Understanding these causes is crucial for developing preventive strategies and improving long-term outcomes. Multidisciplinary management, including nephrologists, transplant surgeons, infectious disease specialists, and cardiologists, is often necessary to address the various factors contributing to graft failure.
Q 22. How do you differentiate between rejection and other complications post-transplant?
Differentiating between rejection and other post-transplant complications requires a holistic approach, combining clinical presentation, laboratory findings, and imaging studies. Kidney transplant rejection, essentially the recipient’s immune system attacking the new kidney, presents with a range of symptoms, from subtle changes in kidney function (e.g., rising creatinine levels) to more overt signs like fever, pain at the transplant site, and decreased urine output. However, these symptoms aren’t exclusive to rejection; infections, medication side effects, and other complications can mimic them.
For instance, a urinary tract infection (UTI) can cause fever and pain, while certain immunosuppressant medications can lead to increased creatinine levels. The key is to systematically investigate each potential cause. A rising creatinine level, for example, needs further evaluation through imaging and biopsy to determine if the cause is rejection or another problem like acute tubular necrosis (ATN), a form of kidney injury often seen post-transplant.
- Rejection: Often involves a gradual or sudden decline in kidney function, accompanied by signs of inflammation (e.g., tenderness over the transplanted kidney).
- Infection: May manifest with fever, chills, localized pain depending on the infection site (e.g., pneumonia, UTI), and altered white blood cell counts.
- Medication Side Effects: Can vary widely but may include nausea, vomiting, hypertension, or changes in blood counts.
Ultimately, a thorough workup that includes blood tests, urine analysis, imaging studies, and potentially a kidney biopsy is crucial to establish a precise diagnosis and guide treatment.
Q 23. Discuss the role of imaging (ultrasound, CT scan) in kidney transplantation.
Imaging plays a crucial role in assessing the anatomy and function of the transplanted kidney and detecting complications. Ultrasound is often the initial imaging modality because it’s non-invasive, readily available, and relatively inexpensive. It allows us to assess kidney size, shape, and perfusion (blood flow), looking for signs of obstruction or fluid collections around the kidney (e.g., urinoma, lymphocele). A urinoma is a collection of urine, while a lymphocele is a collection of lymph fluid.
CT scans provide higher resolution images and are particularly useful in identifying complex anatomical issues, such as vascular complications (e.g., thrombosis, stenosis), masses, or abscesses. CT scans can also be used to guide interventional procedures, like drainage of fluid collections. In a case where I suspected a ureteral stricture (narrowing of the tube carrying urine from the kidney to the bladder), a CT urogram would be particularly useful.
For example, a patient presenting with decreased urine output post-transplant might undergo an ultrasound, revealing hydronephrosis (swelling of the kidney due to urine blockage). A subsequent CT scan could then pinpoint the location of the obstruction, guiding appropriate management (e.g., stent placement).
Q 24. Describe the process of biopsy interpretation in relation to transplant rejection.
Kidney biopsy is an invaluable tool for diagnosing transplant rejection. The process involves a small needle biopsy of the transplanted kidney, which is then analyzed by a pathologist under a microscope. The pathologist assesses various features to determine the type and severity of rejection. This includes evaluating the level of inflammation, the extent of damage to the kidney tissue (tubules, glomeruli, interstitium), and the presence of immune cells.
Biopsy interpretation is crucial for determining the type of rejection (e.g., antibody-mediated rejection (AMR), T-cell mediated rejection (TCMR)) which influences treatment decisions. For example, a biopsy showing evidence of AMR will necessitate a different treatment approach compared to one showing TCMR. The severity of rejection, usually graded on a Banff scale, informs the intensity of treatment. A Banff grade of 3 or more generally indicates more aggressive rejection that requires stronger immunosuppression.
Imagine a scenario where a patient shows declining kidney function, but ultrasound and other blood markers are inconclusive. A biopsy showing cellular rejection (TCMR) with a Banff grade 2 would confirm the diagnosis and guide us to a course of increased immunosuppressants. In contrast, a biopsy revealing no signs of rejection would prompt a search for other potential causes.
Q 25. Explain the role of blood tests in monitoring kidney transplant function.
Blood tests are essential for monitoring kidney transplant function and detecting complications. The most important test is the serum creatinine level, a marker of kidney function. An increase in creatinine indicates declining kidney function, potentially signaling rejection, infection, or other complications. Other tests that regularly monitor kidney function and other vital parameters include:
- Blood Urea Nitrogen (BUN): Another marker of kidney function. Elevated BUN along with creatinine suggests kidney dysfunction.
- Estimated Glomerular Filtration Rate (eGFR): Calculates the filtering capacity of the kidney, a better indicator than creatinine alone for kidney function. A decreasing eGFR suggests declining kidney function.
- Electrolytes: Monitoring electrolytes like potassium, sodium, and calcium is crucial since kidney function is vital in maintaining electrolyte balance.
- Complete Blood Count (CBC): Assesses the blood cell counts which may show signs of infection or medication side effects.
- Immunosuppressant drug levels: Monitoring levels of immunosuppressants (e.g., tacrolimus, cyclosporine) ensures that therapeutic levels are maintained while minimizing toxicity.
Regular monitoring of these tests allows for early detection of problems, enabling prompt intervention and improving patient outcomes. For instance, a sudden increase in creatinine in a patient on stable immunosuppressants will prompt a thorough investigation, including imaging and possible biopsy.
Q 26. How do you manage a patient with a suspected case of cytomegalovirus infection post-transplant?
Cytomegalovirus (CMV) infection is a common complication after kidney transplant, given the immunosuppression needed to prevent rejection. Suspected CMV infection warrants prompt evaluation and treatment. Diagnosis usually involves detecting CMV DNA in the blood using PCR. Clinical presentation may be subtle, with fatigue, fever, and mild abnormalities in liver function tests. More severe cases can involve pneumonitis (lung inflammation), colitis (inflammation of the colon), or hepatitis.
Management involves antiviral medications, primarily ganciclovir or valganciclovir. The duration of treatment depends on the severity of the infection and the patient’s response. In addition to antiviral therapy, supportive care such as managing fever and maintaining adequate hydration is important. Close monitoring of blood counts and organ function is essential throughout treatment.
For instance, if a patient presents with fever and fatigue post-transplant, and the blood test reveals CMV DNA, treatment with ganciclovir will be initiated. Regular monitoring of CMV DNA levels will guide us on the duration of the therapy and help us evaluate treatment efficacy. In severe cases, intravenous ganciclovir might be necessary.
Q 27. Discuss the importance of patient education in kidney transplant care.
Patient education is paramount in kidney transplant care. It’s not just about imparting information; it’s about empowering patients to actively participate in their care and improve their chances of long-term success. Comprehensive education should cover various aspects, including:
- Medication regimen: Detailed explanations of each medication, including its purpose, dosage, side effects, and the importance of adhering to the prescribed schedule.
- Signs and symptoms of rejection and infection: Educating patients on what to look for and when to seek immediate medical attention is crucial for early detection and intervention.
- Lifestyle modifications: Guidance on diet, exercise, avoiding smoking and excessive alcohol consumption, and maintaining a healthy weight are essential for optimizing kidney function and overall health.
- Follow-up appointments: Emphasizing the importance of attending all scheduled appointments for blood tests and other evaluations.
- Disease management: Providing the patient with information on potential long-term complications and their management.
We use various tools to enhance education, including printed materials, videos, group sessions, and individual counseling. A strong emphasis is placed on addressing patient’s concerns and ensuring that information is presented in a clear, understandable way. For example, providing visual aids and checklists related to medication schedules can improve adherence.
Q 28. What are some strategies for improving patient adherence to medication regimens?
Improving medication adherence is critical for successful transplant outcomes. Strategies include:
- Simplified regimens: Consolidating medications into fewer pills or using once-daily formulations whenever possible.
- Medication organizers: Providing pill organizers with labeled compartments to facilitate tracking of medications.
- Reminders: Utilizing text message reminders or mobile applications to prompt medication intake.
- Patient support: Providing access to support groups and trained healthcare professionals who can address questions and provide guidance.
- Addressing barriers: Identifying and resolving barriers to adherence, such as financial constraints, lack of transportation, or cognitive impairment.
- Shared decision-making: Involving the patient in treatment decisions and tailoring the medication regimen to their individual needs and preferences.
For instance, for a patient struggling to remember multiple medications, we might switch to once-daily formulations. If cost is a barrier, we explore options for financial assistance. Active listening and addressing concerns are key to fostering a collaborative approach to medication management. Regularly reinforcing the importance of medication compliance is also crucial.
Key Topics to Learn for Kidney Transplantation Interview
- Immunology of Transplantation: Understanding HLA matching, immunosuppression protocols (calcineurin inhibitors, mTOR inhibitors, etc.), and the mechanisms of rejection (hyperacute, acute, chronic).
- Surgical Techniques: Familiarize yourself with different surgical approaches (e.g., laparoscopic, robotic), graft placement, and vascular anastomosis.
- Pre- and Post-transplant Management: Mastering the assessment of potential recipients, including evaluating their medical history, and managing post-transplant complications (infection, rejection, drug toxicity).
- Dialysis and its Role: Understanding the different types of dialysis and their role in preparing patients for transplantation and bridging them to transplant.
- Ethical Considerations: Be prepared to discuss ethical dilemmas related to organ allocation, informed consent, and end-of-life care.
- Patient Education and Counseling: Knowing how to effectively communicate with patients and families about the transplantation process, risks, benefits, and post-transplant care.
- Data Analysis and Interpretation: Ability to interpret laboratory results (e.g., creatinine, BUN, eGFR), imaging studies (ultrasound, CT scans), and biopsy reports.
- Current Research and Advancements: Staying updated on the latest advancements in immunosuppression, surgical techniques, and organ preservation.
- Troubleshooting and Problem-solving: Develop the ability to identify and address common complications associated with kidney transplantation.
Next Steps
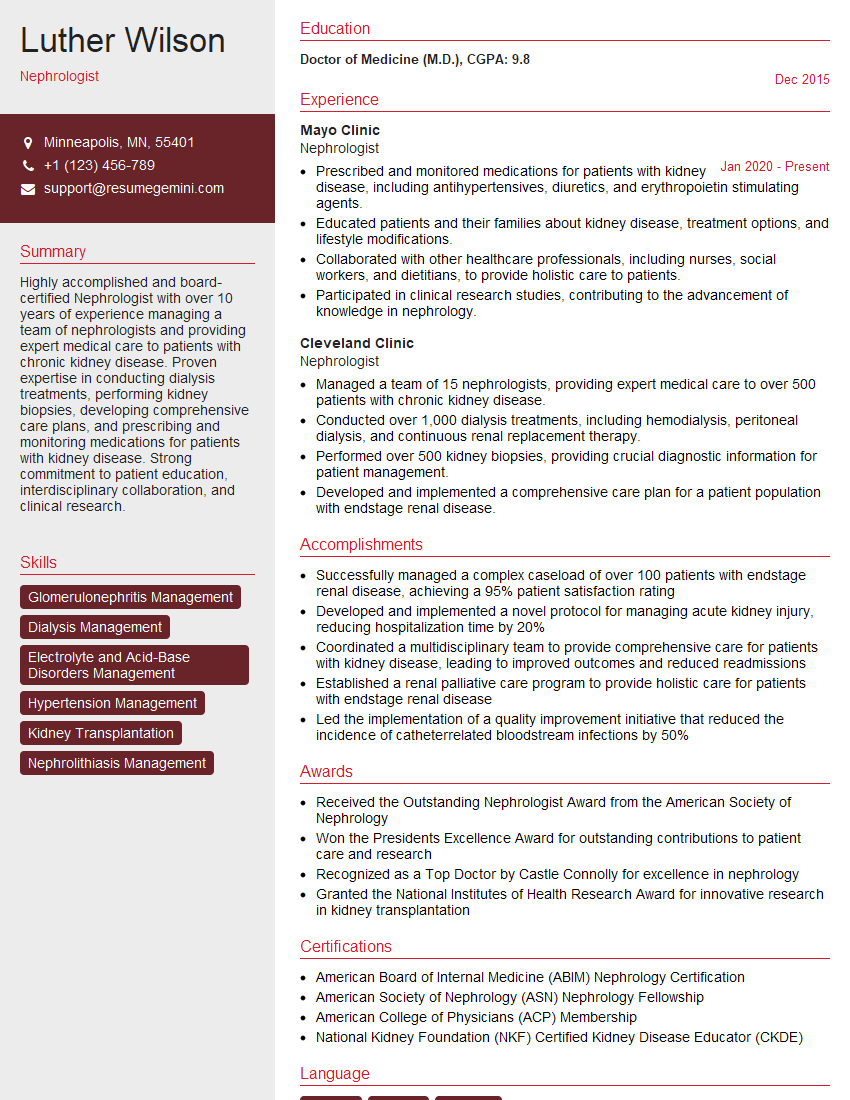
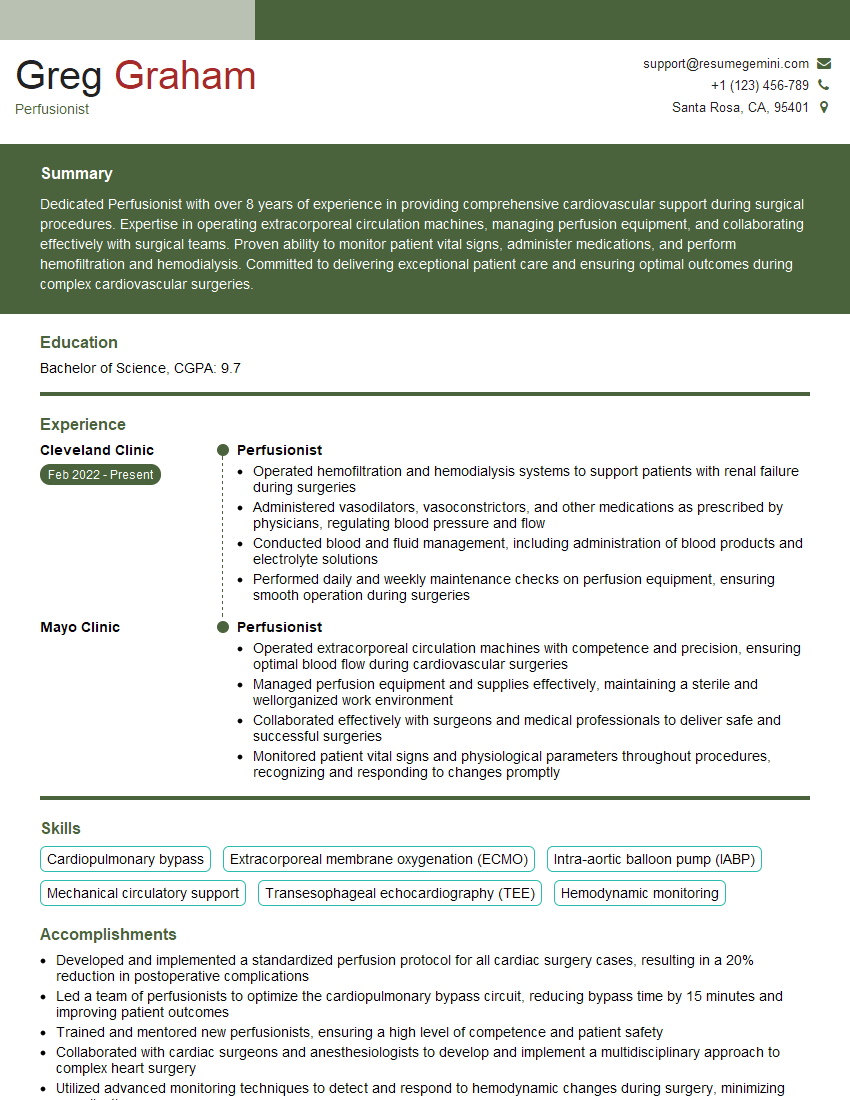
Mastering the intricacies of kidney transplantation significantly enhances your career prospects in nephrology, surgery, or related fields. A strong understanding of these concepts demonstrates expertise and commitment, leading to increased competitiveness in a demanding job market. To further boost your job search, creating an ATS-friendly resume is crucial. An optimized resume increases your chances of getting noticed by recruiters and landing interviews. We highly recommend using ResumeGemini to build a professional and effective resume. ResumeGemini offers a user-friendly platform and provides examples of resumes tailored to Kidney Transplantation to help you showcase your skills and experience effectively.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Take a look at this stunning 2-bedroom apartment perfectly situated NYC’s coveted Hudson Yards!
https://bit.ly/Lovely2BedsApartmentHudsonYards
Live Rent Free!
https://bit.ly/LiveRentFREE
Interesting Article, I liked the depth of knowledge you’ve shared.
Helpful, thanks for sharing.
Hi, I represent a social media marketing agency and liked your blog
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?