Interviews are more than just a Q&A session—they’re a chance to prove your worth. This blog dives into essential Knowledge of Medical Terminology and Disease States interview questions and expert tips to help you align your answers with what hiring managers are looking for. Start preparing to shine!
Questions Asked in Knowledge of Medical Terminology and Disease States Interview
Q 1. Define ‘etiology’ and provide an example.
Etiology refers to the study of the cause or origin of a disease. It’s essentially the detective work of medicine, trying to understand why a disease develops. This understanding is crucial for prevention and treatment.
For example, the etiology of lung cancer can include factors like smoking (a primary cause), exposure to asbestos (an environmental factor), genetics (inherited predispositions), and radon exposure. Understanding the etiology allows doctors to advise patients on risk reduction (like quitting smoking) and to develop targeted therapies.
Q 2. What is the difference between a sign and a symptom?
The difference between a sign and a symptom is key in medical diagnosis. A sign is an objective indication of a disease that can be directly observed or measured by a healthcare professional. A symptom, on the other hand, is a subjective experience reported by the patient. Think of it like this: signs are what the doctor sees or measures, and symptoms are what the patient feels.
For example, a fever (measured temperature above normal) is a sign of infection. A headache (reported by the patient) is a symptom that could be caused by several things, including infection. The doctor uses both signs and symptoms to build a complete clinical picture and reach a diagnosis.
Q 3. Explain the difference between benign and malignant tumors.
Benign and malignant tumors represent the two main classifications of neoplasms (abnormal growths of tissue). The key distinction lies in their behavior and potential for spread.
- Benign tumors are generally slow-growing, encapsulated (meaning they have a distinct border), and do not invade surrounding tissues or metastasize (spread to other parts of the body). They’re usually non-life-threatening, though they can cause problems depending on their location and size. Think of them like a contained, harmless growth.
- Malignant tumors (cancers) are characterized by rapid growth, invasion of surrounding tissues, and the potential to metastasize. They’re life-threatening if not treated appropriately because they can disrupt the function of vital organs and spread throughout the body.
Imagine a garden: a benign tumor is like a well-defined flowerbed, staying in its designated space. A malignant tumor is like a weed aggressively taking over the entire garden, damaging the other plants.
Q 4. What is the significance of the ICD-10 coding system?
The International Classification of Diseases, Tenth Revision (ICD-10) is a system used to code and classify diseases, injuries, and other health conditions. Its significance is multifold:
- Standardized Coding: It provides a universal language for healthcare professionals to communicate effectively about diagnoses and procedures, regardless of location or language.
- Data Collection and Analysis: It enables the collection of consistent, comparable health data on a global scale, which is crucial for epidemiological studies, public health surveillance, and research.
- Healthcare Reimbursement: ICD-10 codes are essential for billing and reimbursement purposes. Insurance companies and healthcare providers use these codes to process claims and track healthcare expenditures.
- Disease Tracking and Monitoring: ICD-10 allows for accurate tracking of disease prevalence and incidence, which helps monitor public health trends and allocate resources effectively.
Q 5. Describe the process of medical transcription.
Medical transcription involves the process of listening to audio recordings (dictations) of healthcare professionals (doctors, nurses, etc.) and converting them into accurate, grammatically correct written reports. These reports include patient history, physical examinations, diagnoses, treatment plans, and other clinical information.
The process usually involves several steps: listening to the audio, typing the information, using specialized medical terminology and correct spelling, ensuring accuracy and completeness, and proofreading the document. Medical transcriptionists need a strong understanding of medical terminology, anatomy, and physiology to produce accurate and meaningful reports. This critical role contributes directly to patient care and ensures clear communication among healthcare providers.
Q 6. What are some common abbreviations used in medical records?
Many abbreviations are used in medical records to save time and space. Some common ones include:
BP: Blood PressureHR: Heart RateRR: Respiratory RateDx: DiagnosisTx: TreatmentRx: Prescriptions.c.: Subcutaneous (under the skin)i.v.: Intravenousp.o.: By mouth
Using abbreviations requires caution; the potential for errors is high. Consistency and careful selection of abbreviations are vital to avoid misinterpretations that could impact patient safety. Clear communication and understanding of abbreviations used are paramount for healthcare professionals.
Q 7. Explain the meaning of ‘prognosis’.
Prognosis refers to the likely course or outcome of a disease. It’s a prediction based on the healthcare professional’s knowledge of the disease, the patient’s overall health, and the response to treatment. It’s important to note that a prognosis is not a guarantee; it is an estimate based on available information.
For instance, a patient with early-stage breast cancer might have a good prognosis if the cancer is effectively treated. However, a patient with advanced-stage cancer may have a less favorable prognosis. The prognosis helps guide treatment decisions, patient counseling, and helps patients and their families understand what they can expect.
Q 8. Differentiate between acute and chronic conditions.
The terms ‘acute’ and ‘chronic’ describe the duration and onset of a disease or condition. Think of it like this: acute is a sudden, intense flare-up, while chronic is a long-term, ongoing battle.
- Acute conditions develop rapidly and usually have a short duration, often resolving completely. For example, the flu is an acute illness; symptoms appear suddenly, usually last a week or two, and then resolve. Another example would be an acute appendicitis, requiring immediate surgical intervention.
- Chronic conditions develop slowly and persist over a long period, often for life. They may have periods of exacerbation (flares) and remission (improvement). Examples include type 2 diabetes, hypertension (high blood pressure), and asthma. These conditions require ongoing management.
The key difference lies in the timeframe: acute is short-term and often self-limiting, whereas chronic is long-term and usually requires ongoing medical attention.
Q 9. What is the role of a Clinical Documentation Improvement Specialist?
A Clinical Documentation Improvement (CDI) Specialist plays a vital role in ensuring the accuracy and completeness of patient medical records. They act as a bridge between clinicians and coders, focusing on improving the clarity and precision of clinical documentation.
- Reviewing charts: CDI specialists meticulously review patient charts, identifying areas where documentation is unclear, incomplete, or inconsistent with the patient’s overall condition.
- Querying physicians: When ambiguities arise, they formulate specific queries to clarify the clinical picture with the treating physicians. This ensures the medical record accurately reflects the patient’s diagnosis, treatment, and prognosis.
- Improving coding accuracy: By improving the documentation, CDI specialists indirectly help to improve the accuracy of medical codes used for billing and reimbursement. Accurate coding is essential for hospitals and healthcare systems to receive appropriate compensation.
- Ensuring regulatory compliance: Accurate and comprehensive documentation is crucial for meeting regulatory requirements and maintaining the integrity of the patient’s medical record. CDI specialists contribute to this compliance.
In essence, CDI specialists are the quality control specialists for medical records, ensuring accuracy and completeness for optimal patient care and financial operations.
Q 10. Explain the concept of comorbidity.
Comorbidity refers to the presence of one or more additional diseases or disorders co-occurring with a primary disease. Imagine it like this: you’re battling a main illness (the primary disease), and several other smaller battles emerge alongside it (the comorbidities).
For instance, a patient with type 2 diabetes (primary disease) may also have hypertension and hyperlipidemia (high cholesterol) (comorbidities). These additional conditions significantly impact treatment planning, prognosis, and overall patient outcomes. The presence of comorbidities often complicates management and increases the risk of complications.
Understanding comorbidities is crucial for healthcare providers to tailor treatment plans that address all the patient’s health issues comprehensively. It also plays a critical role in predicting patient outcomes and resource allocation within healthcare systems.
Q 11. Describe the stages of a disease process, using an example.
Disease processes typically progress through distinct stages, though the exact stages and their duration vary significantly depending on the specific disease. Let’s use the example of HIV infection.
- Incubation Period: After infection with HIV, there’s an incubation period that can last for years. During this time, the virus replicates but may not cause noticeable symptoms.
- Acute Infection: A flu-like illness might develop, indicating the body’s immune response to the virus. This stage is often transient.
- Clinical Latency (Chronic Infection): This is a long asymptomatic period where the virus continues to replicate, but the immune system largely controls it. This phase can last for many years.
- AIDS (Acquired Immunodeficiency Syndrome): This is the final stage, characterized by a severely compromised immune system, making individuals highly susceptible to opportunistic infections and cancers.
Each stage is clinically significant, requiring different management strategies and clinical interventions. Understanding these stages allows healthcare professionals to provide tailored care and improve patient outcomes.
Q 12. How do you handle unfamiliar medical terms?
Encountering unfamiliar medical terms is a common experience, especially with the ever-expanding medical vocabulary. My approach is multi-pronged:
- Utilize medical dictionaries and online resources: I rely heavily on reputable medical dictionaries, both print and online versions like Stedman’s Medical Dictionary or online medical terminologies, ensuring the information comes from a verified source.
- Break down the term: Many medical terms are constructed using prefixes, suffixes, and root words. Breaking these components down often reveals the meaning. For instance, ‘cardiomegaly’ (cardio-heart, -megaly-enlargement) means an enlargement of the heart.
- Consult colleagues: If I’m still unsure after using resources, I don’t hesitate to consult more experienced colleagues or mentors for clarification. Teamwork enhances understanding and ensures patient safety.
This systematic approach ensures accurate understanding and avoids any potential misinterpretations that could negatively impact patient care.
Q 13. What resources do you use to stay current with medical terminology?
Staying current with medical terminology and disease states is paramount in my field. I use a variety of resources to accomplish this:
- Professional medical journals: Reading peer-reviewed articles in journals such as JAMA, The Lancet, and The New England Journal of Medicine helps keep me abreast of the latest research and advancements.
- Medical conferences and webinars: Attending conferences and participating in online webinars allows me to learn from experts in the field and network with other professionals.
- Continuing medical education (CME) courses: Regularly pursuing CME courses is essential for maintaining licensure and expanding my knowledge base.
- Professional organizations: Membership in professional organizations provides access to resources, publications, and continuing education opportunities.
Continuous learning ensures I maintain a high level of expertise and provide the best possible care.
Q 14. Explain the importance of accurate medical coding.
Accurate medical coding is absolutely critical for several reasons. It’s the backbone of healthcare finance and quality improvement.
- Accurate reimbursement: Correct coding ensures healthcare providers receive appropriate payment for services rendered. Inaccurate coding can lead to underpayment or even penalties.
- Public health data: Accurate coding contributes to the collection of reliable data used for public health surveillance, research, and resource allocation. This informs policy decisions and improves healthcare systems.
- Quality improvement initiatives: Accurate coding facilitates the tracking of disease prevalence, treatment effectiveness, and outcomes. This information is essential for identifying areas for improvement in patient care.
- Legal and regulatory compliance: Accurate coding is crucial for complying with federal and state regulations related to healthcare billing and reimbursement.
In short, accurate medical coding isn’t just about billing; it’s about ensuring the financial stability of healthcare organizations, advancing medical research, and improving overall patient care.
Q 15. What are the potential consequences of incorrect medical coding?
Incorrect medical coding has serious consequences, impacting both patient care and financial stability of healthcare organizations. It can lead to:
- Underpayment or denial of claims: If codes don’t accurately reflect the services provided, insurance companies may reject or underpay claims, resulting in financial losses for providers. For example, using a less specific code for a complex procedure could lead to reimbursement for a simpler, cheaper one.
- Delayed or inaccurate patient care: Incorrect coding can lead to incomplete or misleading information in a patient’s medical record, hindering effective treatment. Imagine a patient with a history of allergies, where the allergy is incorrectly coded—this could result in dangerous medication errors.
- Audits and penalties: Healthcare providers are subject to regular audits. Inaccurate coding can trigger investigations, resulting in significant fines, penalties, and legal repercussions. This can severely damage a healthcare provider’s reputation and financial standing.
- Compliance violations: Incorrect coding can violate federal regulations such as HIPAA, leading to further penalties and legal action. This also affects the trust patients place in their healthcare providers.
- Fraud and abuse: In extreme cases, incorrect coding can be intentional and constitute fraud, resulting in criminal charges and severe penalties. This might involve upcoding (billing for a more expensive service than provided) or unbundling (billing separately for services normally included in a single procedure).
Therefore, accurate coding is crucial for efficient healthcare operations and ensuring high-quality patient care.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Describe your experience with different medical record systems.
Throughout my career, I’ve gained extensive experience with a variety of medical record systems, from legacy systems to modern, cloud-based Electronic Health Record (EHR) platforms. I’m proficient in using systems like Epic, Cerner, and Meditech, each with its unique interface and functionalities.
My experience includes:
- Data entry and management: I’m adept at accurately entering and managing patient data, ensuring data integrity and completeness.
- Query resolution: I’m skilled in identifying and resolving discrepancies or missing information within medical records.
- Report generation: I can generate various reports based on the specific needs of the healthcare setting, such as billing reports, quality metrics reports, or patient summaries.
- System troubleshooting: I am able to troubleshoot common issues and report system malfunctions to relevant IT personnel.
- Data migration: I’ve been involved in transitioning between different EHR systems, ensuring a smooth transition and minimal data loss.
My experience with these diverse systems has equipped me with a broad understanding of best practices in medical record management and data security.
Q 17. How do you ensure the confidentiality of patient information?
Protecting patient confidentiality is paramount. I adhere strictly to HIPAA regulations and all internal policies regarding data privacy. My approach encompasses several key strategies:
- Access control: I only access patient records when absolutely necessary for my job duties, and I always log out securely when finished. I understand and comply with the principle of least privilege.
- Data encryption: I am familiar with the use of encryption technologies to protect sensitive patient data both in transit and at rest.
- Secure data disposal: I follow established procedures for the secure disposal of any paper or electronic documents containing patient information.
- Password security: I utilize strong, unique passwords and follow all organizational guidelines for password management.
- Awareness training: I regularly participate in HIPAA compliance training to stay updated on the latest regulations and best practices. This ensures I’m always aware of emerging threats and potential vulnerabilities.
- Reporting breaches: I understand the importance of reporting any suspected or actual breaches of patient data immediately to the appropriate authorities.
In short, maintaining patient confidentiality is not just a policy—it’s a professional responsibility I take very seriously.
Q 18. How do you prioritize tasks in a fast-paced healthcare environment?
Prioritizing tasks in a fast-paced healthcare environment requires a structured and flexible approach. I employ a combination of methods:
- Urgency and Importance Matrix (Eisenhower Matrix): I categorize tasks based on urgency and importance, focusing on high-impact, time-sensitive tasks first. This ensures that critical issues are addressed promptly.
- Workflow optimization: I identify bottlenecks and inefficiencies in my workflow and work to streamline processes to improve efficiency. This might involve using automation tools or collaborating with colleagues to better distribute tasks.
- Time management techniques: I use techniques like time blocking and the Pomodoro Technique to manage my time effectively, enhancing focus and productivity.
- Communication and collaboration: I communicate clearly and proactively with colleagues to ensure coordination and avoid duplication of effort.
- Flexibility and adaptability: In healthcare, priorities can shift quickly. I am adept at adapting to changing circumstances and re-prioritizing tasks as needed. For instance, a patient’s sudden deterioration might necessitate immediate attention and adjustment of the workflow.
This multi-faceted approach helps me remain organized, efficient, and responsive to the ever-changing demands of the healthcare setting.
Q 19. Explain the importance of medical terminology in patient care.
Medical terminology is the cornerstone of effective patient care. It ensures accurate and concise communication among healthcare professionals, minimizes errors, and ultimately improves patient outcomes.
Its importance lies in:
- Precision in diagnosis and treatment: Using precise medical terms ensures everyone involved understands the condition and treatment plan. Using the wrong term could lead to delays or incorrect procedures. For example, knowing the difference between ‘bradycardia’ and ‘tachycardia’ is crucial for appropriate treatment of heart conditions.
- Clear communication among healthcare professionals: Standardized terminology facilitates seamless communication between physicians, nurses, technicians, and other healthcare personnel involved in the patient’s care. This prevents misinterpretations and ensures everyone is on the same page. A simple example is the need for clear communication regarding medication dosages.
- Accurate documentation: Precise medical terminology ensures complete and accurate documentation in patient charts. This is critical for tracking progress, making informed decisions, and avoiding medical errors.
- Patient safety: Accurate medical terminology prevents misunderstandings and contributes directly to patient safety. Any ambiguity in communication could have serious consequences for the patient. The accurate use of terminology can help avoid potentially dangerous medication errors.
- Improved legal protection: Thorough and accurate documentation utilizing correct medical terminology helps protect healthcare providers from potential legal liability.
Without consistent use of accurate medical terminology, patient safety and the quality of care are significantly compromised.
Q 20. What is your understanding of HIPAA regulations?
HIPAA (Health Insurance Portability and Accountability Act) is a US federal law designed to protect the privacy and security of Protected Health Information (PHI). My understanding of HIPAA encompasses:
- Privacy Rule: This rule establishes national standards to protect individuals’ medical records and other health information. It sets limits and conditions on the uses and disclosures allowed without patient authorization. I understand the various permitted disclosures such as those for treatment, payment, and healthcare operations.
- Security Rule: This rule establishes national standards for the security of electronic protected health information. It mandates administrative, physical, and technical safeguards to protect electronic PHI against unauthorized use or disclosure. I understand how to apply these rules to prevent security breaches.
- Breach Notification Rule: This rule outlines requirements for notifying individuals and government authorities in the event of a data breach. I understand the reporting procedures and timelines.
- Enforcement: I understand that violations of HIPAA can result in significant civil and criminal penalties. This underscores the importance of strict adherence.
I am committed to complying with all aspects of HIPAA to safeguard patient privacy and maintain the highest ethical standards in my work.
Q 21. How do you handle conflicting information in medical records?
Handling conflicting information in medical records requires a methodical and careful approach. My strategy involves:
- Identification and Documentation: The first step is to clearly identify the conflicting information and document it meticulously. This documentation should include the source of the conflicting information, the dates, and any relevant context.
- Verification and Reconciliation: I would attempt to verify the accuracy of each piece of conflicting information. This might involve consulting with other healthcare professionals, reviewing supporting documentation, or contacting the patient to clarify the information. I aim to resolve the conflict through evidence-based reconciliation.
- Prioritization and Resolution: If reconciliation isn’t possible, I would prioritize the most reliable source of information. This usually involves using the most recent and well-documented information from credible sources. If both sources are credible but conflicting, I will note the discrepancy clearly in the record and consult with a senior colleague for guidance.
- Documentation of Resolution: Regardless of the outcome, the entire process of identifying, verifying, and resolving the conflict needs to be meticulously documented in the medical record. This ensures transparency and accountability.
- Communication: If the conflict relates to critical patient care information, I would inform the relevant healthcare professionals involved in the patient’s treatment.
Handling conflicting information carefully and systematically ensures accuracy in the medical record, contributing to the overall safety and quality of patient care.
Q 22. Describe your experience with medical billing and insurance processes.
My experience with medical billing and insurance processes is extensive, encompassing both the clinical and administrative sides. I’ve worked directly with various insurance providers, understanding their specific coding requirements, claim submission processes, and reimbursement methodologies. This includes navigating different payer types, such as Medicare, Medicaid, and private insurance plans, each with unique protocols. I’m proficient in identifying and resolving claim denials, understanding the reasons for rejection (e.g., incorrect coding, missing documentation, or pre-authorization issues), and implementing corrective actions to ensure timely payment. My understanding extends to the intricacies of medical billing software and Electronic Health Records (EHR) systems, facilitating accurate data entry, coding, and claim submission. I’m also familiar with the importance of compliance with regulatory guidelines, such as HIPAA, to maintain patient confidentiality and data security throughout the billing cycle. For instance, I successfully resolved a complex denial for a patient’s lengthy hospital stay by meticulously reviewing the medical record and providing detailed supplementary documentation that justified the charges according to the insurance plan’s guidelines.
Q 23. What is your experience with different types of medical imaging?
My experience with medical imaging encompasses a wide range of modalities, including X-ray, CT scans, MRI, ultrasound, and nuclear medicine. I understand the fundamental principles of each imaging technique, its strengths and limitations, and its appropriate clinical applications. For instance, I know that X-rays are excellent for visualizing bone fractures, while MRI provides superior soft tissue detail, crucial for diagnosing ligament tears or brain tumors. Furthermore, I understand the importance of image quality and interpretation, recognizing artifacts and their potential impact on diagnosis. I have hands-on experience reviewing images, recognizing key anatomical structures, and identifying pathological findings which aids in clinical decision making. For example, in one instance, I identified a subtle pneumothorax (collapsed lung) on a chest X-ray that was initially overlooked, contributing to timely intervention and improved patient outcome. My experience also includes working with PACS (Picture Archiving and Communication Systems) for image management and storage.
Q 24. Describe a time you had to interpret complex medical information.
A particularly challenging case involved interpreting a patient’s complex cardiac arrhythmia based on an ECG and Holter monitor data. The ECG showed irregular heartbeats, but the pattern wasn’t immediately clear. The Holter monitor, which records heart rhythm over 24 hours, revealed intermittent episodes of both supraventricular and ventricular tachycardia. To interpret this, I systematically reviewed the ECG waveforms, focusing on intervals like PR and QT, and meticulously analyzed the Holter data for frequency, duration, and associated symptoms documented by the patient. I then correlated this information with the patient’s medical history, including a recent viral infection. This careful analysis allowed me to determine the likely diagnosis of post-viral myocarditis (inflammation of the heart muscle) leading to the arrhythmias, a conclusion confirmed by the cardiologist. This case highlighted the importance of detailed analysis, considering all available data, and appreciating the interplay of various factors in diagnosing complex conditions.
Q 25. How would you explain a complex medical diagnosis to a patient?
Explaining a complex diagnosis to a patient requires empathy, clear communication, and tailoring the information to their level of understanding. I start by using plain language, avoiding medical jargon. I would begin by asking the patient what they already understand or what concerns they have. Then, I’d explain the diagnosis in simple terms, using analogies where appropriate. For example, if explaining heart failure, I might compare the heart to a pump that’s not working efficiently. I’d then explain the implications of the diagnosis in terms of the patient’s daily life and the treatment options available. I’d involve the patient in the decision-making process, allowing them to ask questions and express their concerns. Throughout the process, I would maintain a calm and reassuring demeanor, emphasizing hope and the potential for positive outcomes. For example, with a cancer diagnosis, I’d discuss treatment options and their potential benefits, focusing on the patient’s overall well-being and support systems.
Q 26. What are some common errors in medical coding, and how can they be avoided?
Common errors in medical coding include incorrect selection of codes, missing codes, or using outdated codes. These errors can lead to claim denials, delayed payments, and even legal repercussions. For example, using a code for a symptom instead of the underlying diagnosis is a common mistake. Another frequent error is failing to code for all services provided, leading to underpayment. To avoid these errors, it’s crucial to follow established coding guidelines and utilize comprehensive resources like the ICD (International Classification of Diseases) and CPT (Current Procedural Terminology) manuals. Regular updates and training on the latest coding conventions are critical. Furthermore, using advanced EHR systems with built-in coding assistance and employing quality assurance measures, like auditing claims before submission, can dramatically reduce coding errors and ensure accuracy.
Q 27. How do you handle stress and pressure in a healthcare setting?
Handling stress and pressure in healthcare is paramount. My approach involves a combination of strategies: effective time management to prioritize tasks, utilizing organizational tools, and maintaining clear communication with colleagues to prevent misunderstandings and ensure workload balance. I also practice mindfulness and stress-reduction techniques like deep breathing exercises or short meditations to manage overwhelming situations. Regular breaks and prioritizing self-care, including sufficient sleep and exercise, are essential for maintaining well-being and preventing burnout. Furthermore, actively seeking support from colleagues or supervisors when facing particularly demanding situations fosters a collaborative environment and reduces individual stress. Creating a healthy work-life balance is key to long-term resilience in a high-pressure field.
Q 28. Describe your experience working with diverse healthcare professionals.
I have extensive experience collaborating with a diverse range of healthcare professionals, including physicians, nurses, pharmacists, therapists, and administrative staff. I recognize the importance of effective teamwork, clear communication, and mutual respect to achieve optimal patient outcomes. My communication style is adaptable; I can adjust my approach based on the individual’s role, personality, and communication preferences. I actively listen to others’ perspectives, value their input, and contribute to a collaborative atmosphere where everyone feels comfortable sharing ideas and concerns. For example, in one instance, I worked closely with a multidisciplinary team to manage a patient with complex diabetes. By effectively communicating with the physician, nurse, and dietitian, we developed a comprehensive care plan that addressed the patient’s individual needs and resulted in improved glycemic control.
Key Topics to Learn for Knowledge of Medical Terminology and Disease States Interview
- Medical Terminology Prefixes, Suffixes, and Root Words: Understanding the building blocks of medical terms allows for rapid comprehension of complex medical information and efficient communication with healthcare professionals. Practice breaking down unfamiliar terms into their components.
- Common Disease States and Pathophysiology: Focus on understanding the mechanisms underlying major disease categories (e.g., cardiovascular, respiratory, neurological). Be prepared to discuss the progression, symptoms, and potential treatments of common conditions.
- Diagnostic and Therapeutic Procedures: Familiarize yourself with common diagnostic tests (e.g., blood tests, imaging techniques) and therapeutic interventions (e.g., medications, surgeries) used in the management of different disease states. Consider their applications and limitations.
- Pharmacology Basics: Gain a foundational understanding of drug classifications, mechanisms of action, and common side effects. This is crucial for interpreting medical records and treatment plans.
- Interpreting Medical Records and Reports: Practice analyzing medical reports to extract key information such as diagnoses, treatment plans, and patient history. This demonstrates practical application of your knowledge.
- Ethical Considerations in Healthcare: Understand the ethical implications of medical decisions and patient care. Be prepared to discuss scenarios involving informed consent, patient confidentiality, and end-of-life care.
Next Steps
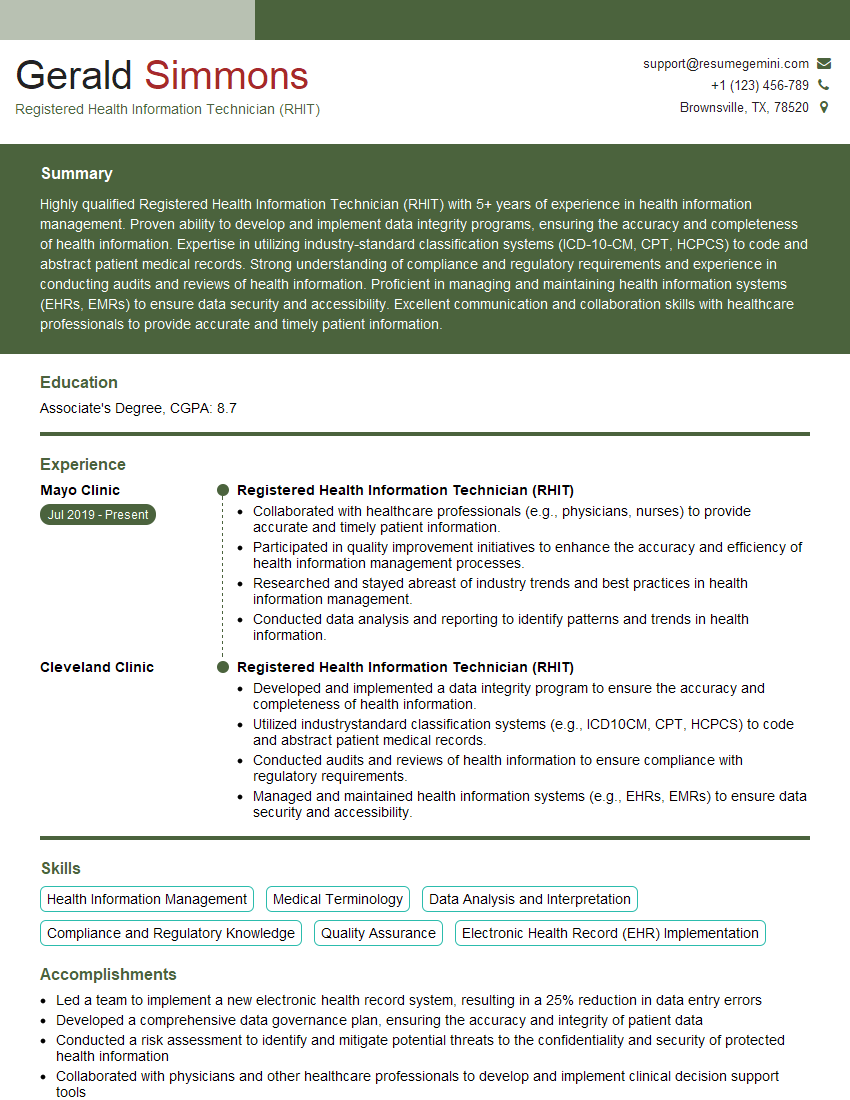
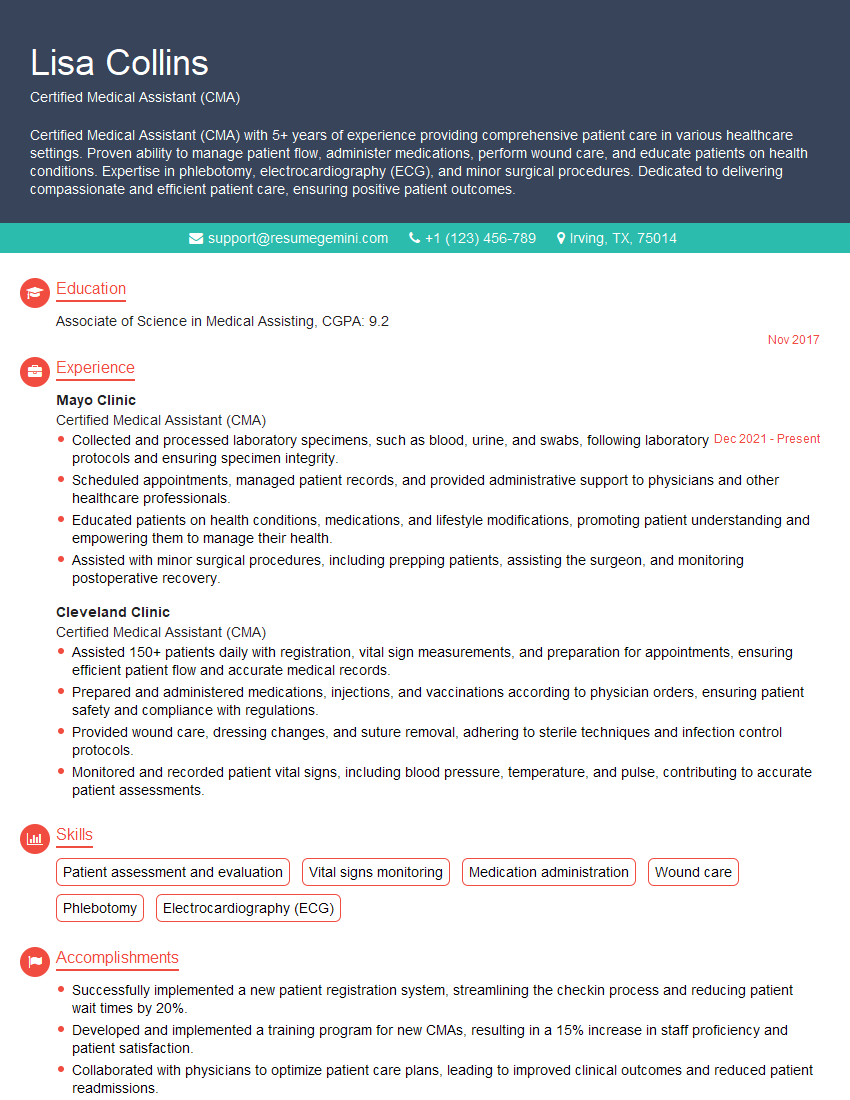
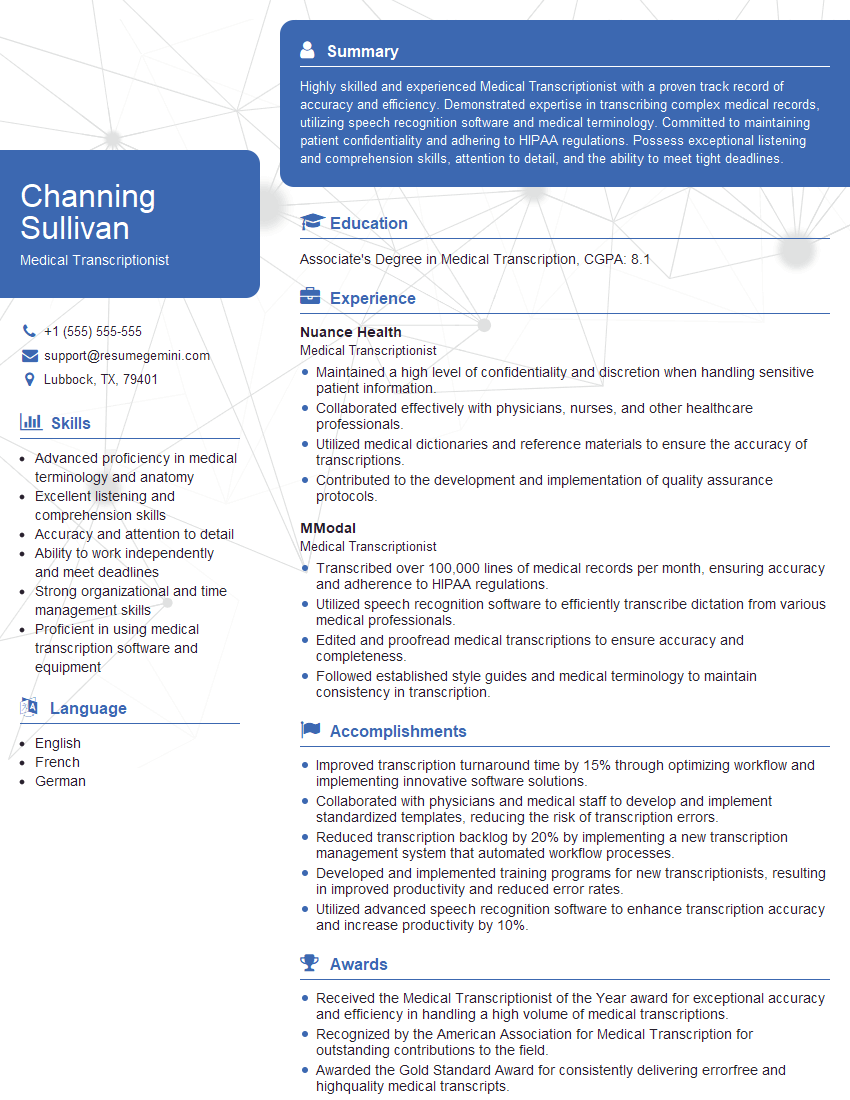
Mastering medical terminology and disease states is paramount for career advancement in healthcare. A strong grasp of these concepts demonstrates your clinical acumen and ability to effectively communicate within a medical setting. To stand out to potential employers, crafting an ATS-friendly resume is crucial. A well-structured resume optimized for Applicant Tracking Systems (ATS) significantly increases your chances of getting noticed. ResumeGemini can be a valuable resource in building a professional and effective resume that highlights your skills and experience. ResumeGemini provides examples of resumes tailored to the Knowledge of Medical Terminology and Disease States field, allowing you to create a powerful document that showcases your expertise. Take the next step towards a successful career in healthcare by creating a standout resume.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
hello,
Our consultant firm based in the USA and our client are interested in your products.
Could you provide your company brochure and respond from your official email id (if different from the current in use), so i can send you the client’s requirement.
Payment before production.
I await your answer.
Regards,
MrSmith
hello,
Our consultant firm based in the USA and our client are interested in your products.
Could you provide your company brochure and respond from your official email id (if different from the current in use), so i can send you the client’s requirement.
Payment before production.
I await your answer.
Regards,
MrSmith
These apartments are so amazing, posting them online would break the algorithm.
https://bit.ly/Lovely2BedsApartmentHudsonYards
Reach out at [email protected] and let’s get started!
Take a look at this stunning 2-bedroom apartment perfectly situated NYC’s coveted Hudson Yards!
https://bit.ly/Lovely2BedsApartmentHudsonYards
Live Rent Free!
https://bit.ly/LiveRentFREE
Interesting Article, I liked the depth of knowledge you’ve shared.
Helpful, thanks for sharing.
Hi, I represent a social media marketing agency and liked your blog
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?