Interviews are opportunities to demonstrate your expertise, and this guide is here to help you shine. Explore the essential Medication Monitoring and Interpretation interview questions that employers frequently ask, paired with strategies for crafting responses that set you apart from the competition.
Questions Asked in Medication Monitoring and Interpretation Interview
Q 1. Describe your experience with medication reconciliation.
Medication reconciliation is the process of creating the most accurate list possible of all medications a patient is currently taking. This includes all prescription medications, over-the-counter drugs, herbal remedies, and supplements. It’s crucial to prevent medication errors, adverse drug events, and ensure patient safety. Think of it like a detective carefully reviewing all pieces of a puzzle to build a complete picture of the patient’s medication profile.
My experience involves performing medication reconciliation at various stages of patient care: on admission to a hospital, before surgery, during transitions between care settings (e.g., hospital to rehab), and during routine clinic visits. I’ve developed a systematic approach using standardized forms and electronic health records (EHRs) to compare the patient’s self-reported medication list with their medical records and pharmacy records. This involves clarifying discrepancies through direct patient interviews, reviewing pharmacy records, and collaborating with pharmacists and other healthcare professionals to resolve inconsistencies. For example, I once discovered a patient was taking a duplicate medication due to receiving prescriptions from multiple specialists. Reconciling this prevented a potential overdose.
Q 2. Explain the process of identifying potential drug interactions.
Identifying potential drug interactions requires a detailed understanding of pharmacology and the use of various tools. The process starts with obtaining a complete medication list, including dosages and frequencies. Then, I use several approaches:
- Clinical judgment: I’m familiar with common drug interactions, such as the interaction between warfarin and NSAIDs (Nonsteroidal anti-inflammatory drugs), which can increase bleeding risk. This knowledge informs my initial assessment.
- Electronic tools: Most EHRs and pharmacy systems have built-in drug interaction checkers. These systems compare the medications prescribed and alert the healthcare provider to potential problems. I always carefully review these alerts and assess their clinical significance in the context of the patient’s condition.
- Pharmacist consultation: When dealing with complex medication regimens or uncertain interactions, I consult with pharmacists. They are invaluable resources in this process.
For instance, I recently identified a potential interaction between a patient’s newly prescribed antibiotic and their heart medication. The interaction checker flagged a possible increased risk of arrhythmia. By reviewing the literature and consulting the pharmacist, we decided on an alternative antibiotic that minimized the risk.
Q 3. How do you handle discrepancies in medication records?
Discrepancies in medication records are common and must be addressed systematically. My approach involves:
- Verification: The first step is to verify the discrepancy. Is the information missing, inaccurate, or conflicting? I use multiple sources, including patient interview, medical records, and pharmacy records, to confirm the information.
- Clarification: I directly communicate with the patient to clarify any discrepancies. This involves carefully asking questions about medication names, dosages, frequencies, and routes of administration. Sometimes, patients may forget or inaccurately report their medication history.
- Documentation: I meticulously document all discrepancies and the steps taken to resolve them. This creates a transparent audit trail and ensures accountability.
- Collaboration: If a discrepancy remains unresolved, I collaborate with the prescribing physician and pharmacist to reach a consensus. This collaborative approach reduces errors and ensures patient safety.
For example, a patient’s record showed they were prescribed a specific medication, but the patient denied taking it. Through careful questioning, we discovered a prescription from a different clinic that wasn’t documented in the EHR. Adding this missing information resolved the discrepancy.
Q 4. What are the key components of a comprehensive medication review?
A comprehensive medication review (CMR) is a thorough assessment of a patient’s medications to identify and resolve potential problems. Key components include:
- Collecting medication information: This involves obtaining a complete list of all medications, including prescriptions, OTCs, and supplements.
- Reviewing patient-specific factors: This includes considering the patient’s age, medical conditions, allergies, and other relevant factors that could influence medication use.
- Assessing for drug interactions and adverse effects: This step examines potential interactions and side effects based on the patient’s medication regimen.
- Evaluating medication appropriateness: This involves determining whether the medications are necessary, effective, and at the appropriate dose, route, and frequency for the patient.
- Developing a medication action plan: Based on the review, this outlines strategies for resolving identified issues, such as discontinuing unnecessary medications, adjusting dosages, or adding medications to manage side effects.
- Patient education: Educating the patient about their medications and potential risks and benefits is crucial.
CMRs are crucial for improving medication safety and effectiveness, especially in older adults and patients with multiple comorbidities.
Q 5. Describe your understanding of medication adherence and strategies to improve it.
Medication adherence refers to the extent to which patients take their medications as prescribed. Poor adherence is a significant problem, leading to ineffective treatment and increased healthcare costs. Understanding the reasons behind non-adherence is crucial.
Strategies to improve adherence include:
- Patient education: Providing clear, concise information about the medication’s purpose, dosage, side effects, and potential interactions in a language the patient understands.
- Simplified regimens: Prescribing fewer medications and adjusting the dosing schedule to make it easier for patients to follow.
- Medication reminders: Using pill organizers, alarms, or mobile apps to remind patients to take their medications.
- Addressing barriers: Identifying and addressing any barriers to adherence, such as cost, side effects, or lack of transportation.
- Collaborative care: Involving family members, caregivers, and pharmacists in supporting medication adherence.
For example, I worked with a patient struggling with adherence due to complex medication timing. By simplifying the regimen and providing a pill organizer, we dramatically improved their adherence.
Q 6. How do you verify the accuracy of medication orders?
Verifying the accuracy of medication orders is paramount to patient safety. My approach involves multiple layers of verification:
- Comparing the order to the medication profile: I always check the new order against the patient’s existing medication list to identify potential drug interactions or duplications.
- Checking for allergies and contraindications: Thorough review of the patient’s allergy and contraindication history is vital to ensure the ordered medication is safe for the individual.
- Verifying the dose, route, and frequency: I carefully check if the prescribed dose, route of administration, and frequency are appropriate for the patient and the medication.
- Utilizing the EHR’s clinical decision support systems: I rely on the built-in alerts and warnings in the EHR to catch potential errors.
- Double-checking with the prescriber if necessary: If any ambiguities or concerns arise during verification, I immediately contact the prescribing physician for clarification.
A simple oversight, like a decimal point error in the dose, can have severe consequences. Therefore, careful and meticulous verification is crucial at every stage.
Q 7. Explain your knowledge of different medication administration routes.
Medication administration routes refer to the method by which medication is introduced into the body. Different routes have different advantages and disadvantages.
- Oral: The most common route, where medications are swallowed. It’s convenient but can be affected by factors such as gastric absorption.
- Sublingual/Buccal: Medications are placed under the tongue or between the cheek and gum, allowing rapid absorption.
- Intravenous (IV): Administered directly into a vein, providing rapid onset and precise control of drug levels. However, it requires skilled administration and carries a risk of infection and other complications.
- Intramuscular (IM): Injected into a muscle, providing slower absorption than IV but faster than subcutaneous.
- Subcutaneous (SC): Injected under the skin, suitable for slow-release medications.
- Topical: Applied to the skin or mucous membranes. Absorption varies depending on the area and formulation.
- Inhalation: Administered through inhalation, primarily used for respiratory medications.
- Rectal: Administered via the rectum, often used when oral administration is difficult or impractical.
Choosing the appropriate route is determined by several factors, including the medication’s properties, the patient’s condition, and the desired speed of onset. For example, in emergency situations where rapid effect is crucial, IV administration is preferred. Conversely, for medications requiring slow and sustained release, SC or oral administration might be suitable.
Q 8. What are the common side effects of [Specific Medication Class] and how would you monitor for them?
Let’s discuss the common side effects of ACE inhibitors, a common class of medications used to treat hypertension and heart failure. These drugs work by blocking the production of angiotensin II, a hormone that constricts blood vessels. Common side effects often stem from this mechanism.
- Dry Cough: This is perhaps the most frequently reported side effect, occurring in roughly 10-20% of patients. It’s due to a build-up of bradykinin in the lungs. Monitoring involves regular patient check-ins, asking about cough onset, severity, and impact on daily life. If significant, alternative medications may be considered.
- Hypotension (low blood pressure): ACE inhibitors can cause a drop in blood pressure, particularly upon initiation or dose increases. Monitoring involves checking blood pressure regularly, especially at the start of treatment and after dose adjustments. Patients should be educated on signs of hypotension (dizziness, lightheadedness) and advised to change positions slowly.
- Hyperkalemia (high potassium levels): ACE inhibitors can impair potassium excretion by the kidneys. Monitoring involves periodic blood tests to measure potassium levels. Patients with pre-existing kidney disease or those on potassium-sparing diuretics are at higher risk and require closer monitoring.
- Renal dysfunction: In patients with pre-existing kidney disease, ACE inhibitors can further impair renal function. Monitoring involves regular assessment of kidney function through blood tests (creatinine, GFR).
Effective monitoring is crucial and requires a proactive approach combining patient education, regular check-ups including blood pressure and blood tests, and careful consideration of potential drug interactions.
Q 9. Describe a situation where you identified a potential medication error. How did you resolve it?
I once identified a potential medication error involving a patient prescribed warfarin, a blood thinner. The patient’s electronic health record indicated a significantly increased dose of warfarin without any documented reason for the change. Furthermore, the patient’s INR (international normalized ratio), a measure of blood clotting time, was markedly elevated in the latest lab results, indicating a risk of excessive bleeding.
My immediate action involved verifying the medication order with the prescribing physician’s notes and the pharmacy dispensing records. I found a discrepancy: the new, higher dose was entered incorrectly into the EHR. The physician’s original order reflected the previous, safer dose.
I then immediately contacted the physician to clarify the discrepancy. Once confirmed, I worked with the pharmacy to correct the order, ensuring the patient received the correct dose. The patient’s INR was closely monitored afterward. The incident prompted a review of our EHR order entry procedures to prevent similar mistakes in the future. This highlighted the critical importance of careful order verification and the use of multi-layered safety checks.
Q 10. How familiar are you with electronic health record (EHR) systems and their role in medication management?
I am highly familiar with EHR systems and their vital role in medication management. EHRs provide a centralized, electronic repository of patient health information, including medication lists, allergies, and lab results. This streamlined access is crucial for effective medication monitoring and preventing medication errors. For example, many EHR systems now incorporate clinical decision support systems (CDSS) that alert clinicians to potential drug interactions, contraindications, and dosage errors before the medication is prescribed or administered. They also allow for better tracking of medication adherence and patient education.
However, EHR systems also present challenges. The sheer volume of data can be overwhelming, and issues with data entry accuracy and interoperability can occur. Therefore, thorough training and a robust quality control process are essential to maximize the benefits of EHRs in medication management. The successful use of these systems demands a high degree of proficiency and a focus on continuous improvement.
Q 11. Explain your understanding of medication storage and handling procedures.
Medication storage and handling are critical for maintaining medication efficacy and patient safety. Improper storage can lead to degradation, rendering medications ineffective or even harmful. Proper storage requires adherence to specific temperature and humidity conditions as indicated by the medication labeling. This often involves storing medications in a cool, dry place, away from direct sunlight and sources of heat or moisture.
Handling procedures involve careful attention to hygiene to prevent contamination. Gloves should be worn when handling certain medications. Medication should be dispensed according to the prescribed dosages and schedules, with clear labeling and accurate record-keeping. Expired medications should be disposed of properly to prevent accidental ingestion or environmental contamination. Following established guidelines and utilizing appropriate storage containers are essential for maintaining medication integrity and ensuring patient safety.
Q 12. How do you communicate effectively with patients about their medications?
Effective communication with patients about their medications is paramount. I use a simple, clear, and patient-centered approach. I begin by ensuring the patient understands the medication’s purpose, dosage, and administration instructions using plain language, avoiding medical jargon. I actively encourage patients to ask questions and address any concerns or misunderstandings.
I provide written instructions supplementing the verbal explanation, and I confirm their understanding before concluding the discussion. For patients with specific needs, such as visual or cognitive impairments, I adapt my communication style and utilize appropriate aids, like large-print instructions or visual aids. I also involve family members or caregivers, if appropriate, to enhance understanding and support medication adherence. Finally, I provide a mechanism for follow-up questions and concerns, ensuring they feel supported throughout the medication process.
Q 13. How do you educate patients about potential adverse drug reactions?
Educating patients about potential adverse drug reactions (ADRs) is a crucial aspect of medication safety. I begin by explaining that while medications are generally safe, there’s always a possibility of experiencing side effects. I discuss the common ADRs associated with the specific medication, emphasizing the severity and likelihood of each. This includes providing clear descriptions of what to watch out for and when to seek immediate medical attention.
I also emphasize the importance of reporting any unusual symptoms, even if they seem minor. I use examples and analogies to illustrate the importance of proactive reporting and early intervention. I provide patients with written materials outlining potential ADRs and instructions on how to contact their healthcare provider or pharmacist to report them. Regular follow-up appointments help reinforce the education and address any concerns the patient may have.
Q 14. What is your experience with managing high-risk medications?
I have extensive experience managing high-risk medications, such as those with narrow therapeutic indices (e.g., warfarin, digoxin), medications that can cause life-threatening adverse effects (e.g., chemotherapy agents), and opioids. Managing these medications requires meticulous attention to detail and adherence to strict protocols. This includes careful monitoring of lab values (e.g., INR for warfarin), close observation for adverse effects, and frequent communication with the prescribing physician.
My approach involves utilizing all available resources, including EHR systems with CDSS, to identify and mitigate potential risks. I maintain a high level of vigilance to prevent medication errors, including double-checking dosages, administering medications safely, and promptly reporting any discrepancies or adverse events. Continuous professional development in medication safety is essential to maintain expertise in this complex area.
Q 15. Describe your experience with managing controlled substances.
Managing controlled substances requires meticulous adherence to regulations and protocols. My experience includes ensuring accurate dispensing, careful documentation, and strict inventory control, all in compliance with relevant state and federal laws. This involves verifying prescriptions, properly storing medications under lock and key, and regularly conducting inventory checks to identify any discrepancies. For instance, I’ve been involved in developing and implementing procedures for tracking opioid prescriptions, including the use of electronic prescribing and automated dispensing cabinets to mitigate diversion and ensure patient safety. I’m proficient in recognizing potential signs of abuse or diversion and know how to report suspected violations promptly. My experience extends to working with patients on controlled substance treatment plans, educating them about safe usage and potential risks of misuse.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. What resources do you utilize to stay current with medication information?
Staying current on medication information is crucial in this field. I regularly utilize several resources, including:
- Micromedex: This comprehensive database provides detailed drug information, including adverse effects, contraindications, and interactions.
- Lexicomp: Another excellent drug information resource offering similar detail to Micromedex, with a user-friendly interface.
- DailyMed (FDA): The official FDA website, providing access to drug labels, package inserts, and updates on medication safety alerts.
- Professional Journals: I subscribe to and regularly read journals like the Annals of Internal Medicine and the New England Journal of Medicine to stay abreast of the latest research and clinical guidelines.
- Continuing Education Courses: I participate in continuing education courses and webinars to maintain and update my knowledge of new medications and treatment approaches.
By combining these resources, I ensure that my medication knowledge remains up-to-date and accurate, enabling me to provide the best possible care to my patients.
Q 17. How do you handle patient inquiries about medication side effects?
When a patient has questions about medication side effects, I approach the situation with empathy and thoroughness. First, I actively listen to their concerns and try to understand their specific experience. Then, I review their medication list and the known side effects of each drug. If the reported side effect is consistent with the medication’s profile, I explain its likelihood, severity, and possible management strategies. For example, if a patient complains of nausea from a new medication, I may suggest strategies like taking it with food or adjusting the dosage under the guidance of their physician. If the side effect is severe or unexpected, I always recommend they contact their prescribing physician immediately. I document the conversation thoroughly, recording the patient’s concerns, my response, and any actions taken.
Imagine a patient experiencing dizziness from a blood pressure medication. I’d explain that dizziness is a common side effect, offer reassurance, and emphasize the importance of following the physician’s instructions. However, if the dizziness is severe, I’d immediately advise contact with their doctor to assess the need for a medication change or adjustment.
Q 18. What is your process for documenting medication administration?
My medication administration documentation process is rigorous and follows established standards. It always includes:
- Patient identification: Using two identifiers, such as name and date of birth, to ensure the correct patient receives the medication.
- Medication name and dosage: Clearly stating the name, dose, and route of administration of the medication.
- Time of administration: Recording the precise time the medication was given.
- Route of administration: Specifying whether the medication was given orally, intravenously, intramuscularly, etc.
- Patient response: Noting any observed patient reactions or responses to the medication, both positive and negative.
- Signature/Initials: My signature or initials confirming administration.
All documentation is done electronically using a secure electronic health record system to ensure accuracy, legibility, and easy access. This system allows for easy tracking and review of medication administration history.
Q 19. How do you assess a patient’s understanding of their medication regimen?
Assessing a patient’s understanding of their medication regimen is crucial for ensuring medication adherence and safety. I use a combination of strategies, including:
- Teach-back method: After explaining the medication regimen, I ask the patient to explain it back to me in their own words. This helps identify any gaps in understanding.
- Open-ended questions: I ask questions like “What concerns do you have about this medication?” or “How will you remember to take your medication?” to elicit information about the patient’s comprehension and potential barriers to adherence.
- Visual aids: Using pill organizers, medication charts, or diagrams can help patients visualize their regimen.
- Written instructions: Providing clear and concise written instructions, in a language and literacy level appropriate for the patient.
- Follow-up: Scheduling follow-up appointments or calls to review the medication regimen and address any questions or concerns.
For example, I might use a teach-back method after explaining a complex regimen of multiple medications taken at different times. If the patient struggles to recall the schedule, I’ll provide written instructions and a pill organizer.
Q 20. What strategies do you employ to minimize medication errors?
Minimizing medication errors requires a multi-faceted approach. My strategies include:
- Five Rights of Medication Administration: Rigorously checking the right patient, right medication, right dose, right route, and right time.
- Double-checking: Always double-checking medication orders and dosages before administering medications.
- Bar code scanning: Utilizing bar code scanning technology to verify medication and patient identity.
- Automated dispensing cabinets: Utilizing automated dispensing cabinets to manage medication inventory and reduce manual dispensing errors.
- Medication reconciliation: Regularly reconciling medication lists to identify discrepancies and prevent errors.
- Reporting and learning from errors: Promptly reporting any medication errors and participating in root cause analysis to identify and address contributing factors.
A simple example is using the ‘five rights’ when administering medication. I would verify the patient’s identity using two identifiers before administering any medication. This seemingly small step prevents potentially fatal errors.
Q 21. Describe your understanding of pharmacokinetics and pharmacodynamics.
Pharmacokinetics describes what the body does to a drug, while pharmacodynamics describes what the drug does to the body. Pharmacokinetics involves the processes of absorption, distribution, metabolism, and excretion (ADME).
- Absorption refers to how a drug enters the bloodstream.
- Distribution involves the drug’s movement throughout the body.
- Metabolism is the process by which the body breaks down the drug, often in the liver.
- Excretion is how the drug and its metabolites are eliminated from the body, usually through the kidneys.
Pharmacodynamics focuses on the drug’s effects on the body, including its mechanism of action, dose-response relationship, and therapeutic effects and side effects. For example, a drug’s efficacy might be related to its ability to bind to a specific receptor, triggering a cellular response. Understanding ADME and pharmacodynamics helps clinicians select the appropriate dose, route of administration, and monitoring plan for a medication, maximizing therapeutic benefits while minimizing adverse events.
Consider a patient prescribed an antibiotic. Pharmacokinetics would guide us in choosing the dosage and timing to ensure sufficient drug levels are reached in the target tissue. Pharmacodynamics would help us predict the drug’s effects on the bacteria and its potential side effects on the patient, allowing us to tailor treatment effectively and safely.
Q 22. How do you interpret laboratory results relevant to medication monitoring?
Interpreting lab results in medication monitoring involves assessing how a patient’s physiology responds to a drug. We’re not just looking at raw numbers; we’re looking for trends and how those numbers relate to the patient’s clinical picture and the medication’s therapeutic range. For example, a therapeutic drug monitoring (TDM) blood test for vancomycin might show a trough level (lowest concentration) too low, indicating insufficient dosing and a risk of treatment failure, or too high, increasing the risk of toxicity (nephrotoxicity in this case). We consider factors like the patient’s age, kidney function (creatinine clearance), and liver function.
Let’s say we’re monitoring a patient on lithium for bipolar disorder. We’d look at their serum lithium level. A level within the therapeutic range (generally 0.6-1.2 mEq/L) indicates effective treatment. However, levels outside this range – too low or too high – require dosage adjustment to optimize efficacy and minimize adverse effects like tremors, nausea, or even neurological problems. We might also examine other relevant lab markers like thyroid function tests, as lithium can affect thyroid function. The interpretation always involves a holistic consideration of the patient’s condition and response to medication. It’s not just about the numbers but about what those numbers tell us about the patient’s health in the context of their medication regimen.
Q 23. What are the legal and ethical considerations related to medication administration?
Legal and ethical considerations in medication administration are paramount. Legally, we must adhere to all applicable laws and regulations, including those concerning prescription writing, controlled substances, and patient confidentiality (HIPAA in the US). Ethically, our actions must always prioritize patient safety, autonomy, and well-being. This involves informed consent – patients need to understand their medications, their potential benefits and risks, and have the autonomy to refuse treatment.
- Confidentiality: Protecting patient information is vital and a breach can have serious legal consequences.
- Competence: Administrators must be properly trained and qualified to safely administer medications.
- Documentation: Accurate and thorough documentation of medication administration is crucial for legal and clinical reasons. Any errors or deviations must be documented transparently.
- Refusal of Treatment: Respecting a patient’s right to refuse medication is a fundamental ethical principle, even if it might negatively affect their health. Documentation of this refusal is important.
A real-world example is the importance of following established protocols for administering narcotics. Failing to do so could lead to serious consequences for both the patient and the healthcare professional, including disciplinary action or legal repercussions.
Q 24. Explain your understanding of medication-related quality indicators.
Medication-related quality indicators (MRQIs) are measures used to assess the quality and safety of medication use processes. They help identify areas for improvement within healthcare systems. Examples include the rate of medication errors, medication reconciliation accuracy, the percentage of patients receiving appropriate medication therapy management, the rate of adverse drug events, and the adherence rate to medication administration guidelines. MRQIs can be used to track performance over time, compare different healthcare facilities, or evaluate the effectiveness of interventions aimed at improving medication safety.
Think of MRQIs as ‘check-engine’ lights for medication management. A high rate of medication errors suggests a system-wide problem that needs attention. Similarly, low adherence rates might point to challenges in patient education or access to medications. By tracking these indicators, we can identify vulnerabilities and proactively work towards creating a safer and more effective medication use system.
Q 25. How do you use clinical decision support systems in medication management?
Clinical Decision Support Systems (CDSS) are invaluable tools in medication management. These systems use computerized algorithms and clinical knowledge bases to provide clinicians with real-time guidance and alerts during the medication use process. They can help prevent medication errors by identifying potential drug interactions, allergies, contraindications, and inappropriate dosages. Some CDSS can personalize medication recommendations based on patient-specific data, like age, comorbidities, and genetic factors.
For example, a CDSS might flag a potential interaction between two medications a physician is prescribing, prompting them to consider an alternative or make adjustments to the dosage regimen. Or it might alert a nurse to a potential allergy before administering a medication. The integration of CDSS with Electronic Health Records (EHRs) streamlines the workflow and facilitates better medication decision-making. Effectively using a CDSS requires understanding its capabilities and limitations, and clinicians need to critically evaluate the advice provided by the system, making sure it’s suitable for the individual patient.
Q 26. Describe your experience with medication reconciliation using different EHR systems.
Medication reconciliation is the process of comparing a patient’s current medication list with their medication orders at each transition of care (e.g., admission to hospital, transfer between units, discharge). This crucial step helps to ensure accuracy and prevent medication discrepancies that could lead to ADEs. My experience involves using various EHR systems, each with different workflows and interfaces. The core principle remains the same, but the specifics vary. Some EHRs have automated reconciliation tools, while others require more manual data entry and comparison.
For instance, in one system, I utilized an automated tool that imported the patient’s medication list from their previous provider, flagging any potential discrepancies, such as missing medications, dosage changes, or duplicate entries. In another system, reconciliation was more manual, involving comparing the patient’s self-reported list with the medication orders and reviewing each medication meticulously. Regardless of the system used, a systematic approach, involving thorough review and verification, is always necessary. Effective medication reconciliation requires attention to detail, accuracy, and clear communication with the patient and other healthcare professionals.
Q 27. Explain how you would identify and respond to an adverse drug event (ADE).
Identifying and responding to an Adverse Drug Event (ADE) requires a systematic approach. First, we need to establish a temporal relationship between the medication and the event. This involves carefully reviewing the patient’s medical history, medication list, and the timeline of events leading up to the ADE. Symptoms need to be analyzed to determine if they are consistent with known side effects of the medications involved. Second, we need to assess the severity of the ADE using standardized scales. Then, we consider the plausibility of the medication as the cause, considering other potential factors.
For example, a patient develops a rash after starting a new antibiotic. We’d review the medication’s known side effects (rash being a common one for some antibiotics) and consider other factors that could have caused the rash (e.g., other medications, infections). If we determine the ADE is likely medication-related, we need to take immediate action. This might involve stopping the medication, providing supportive care, and notifying the physician. Depending on severity, reporting to regulatory agencies might be necessary. Detailed documentation of the ADE, including the actions taken, is essential for continuous monitoring and learning from adverse events. A thorough investigation helps to understand the cause and prevent similar incidents in the future. A post-hoc analysis of the ADE might reveal systematic factors that contributed to it, prompting changes in protocols or training.
Key Topics to Learn for Medication Monitoring and Interpretation Interview
- Pharmacokinetics and Pharmacodynamics: Understanding how drugs are absorbed, distributed, metabolized, and excreted, and how these processes affect drug action and efficacy.
- Medication Interactions: Analyzing potential interactions between medications, including drug-drug, drug-food, and drug-disease interactions, and their clinical significance. Practical application: Identifying potential adverse events based on a patient’s medication list.
- Adverse Drug Reactions (ADRs): Recognizing common and serious ADRs, understanding their mechanisms, and implementing appropriate interventions. Practical application: Case study analysis of ADRs and appropriate reporting procedures.
- Therapeutic Drug Monitoring (TDM): Interpreting laboratory results to optimize medication dosages and ensure therapeutic efficacy while minimizing toxicity. Practical application: Calculating therapeutic ranges and assessing patient response to medication adjustments.
- Electronic Health Records (EHR) Systems: Navigating and interpreting medication-related information within EHRs, including medication reconciliation and order entry. Practical application: Demonstrating proficiency in extracting relevant information from EHR systems.
- Legal and Ethical Considerations: Understanding medication regulations, patient confidentiality, and professional responsibilities related to medication management. Practical application: Analyzing ethical dilemmas in medication management scenarios.
- Patient Education and Counseling: Communicating medication information clearly and effectively to patients and their families. Practical application: Developing patient education materials and strategies.
Next Steps
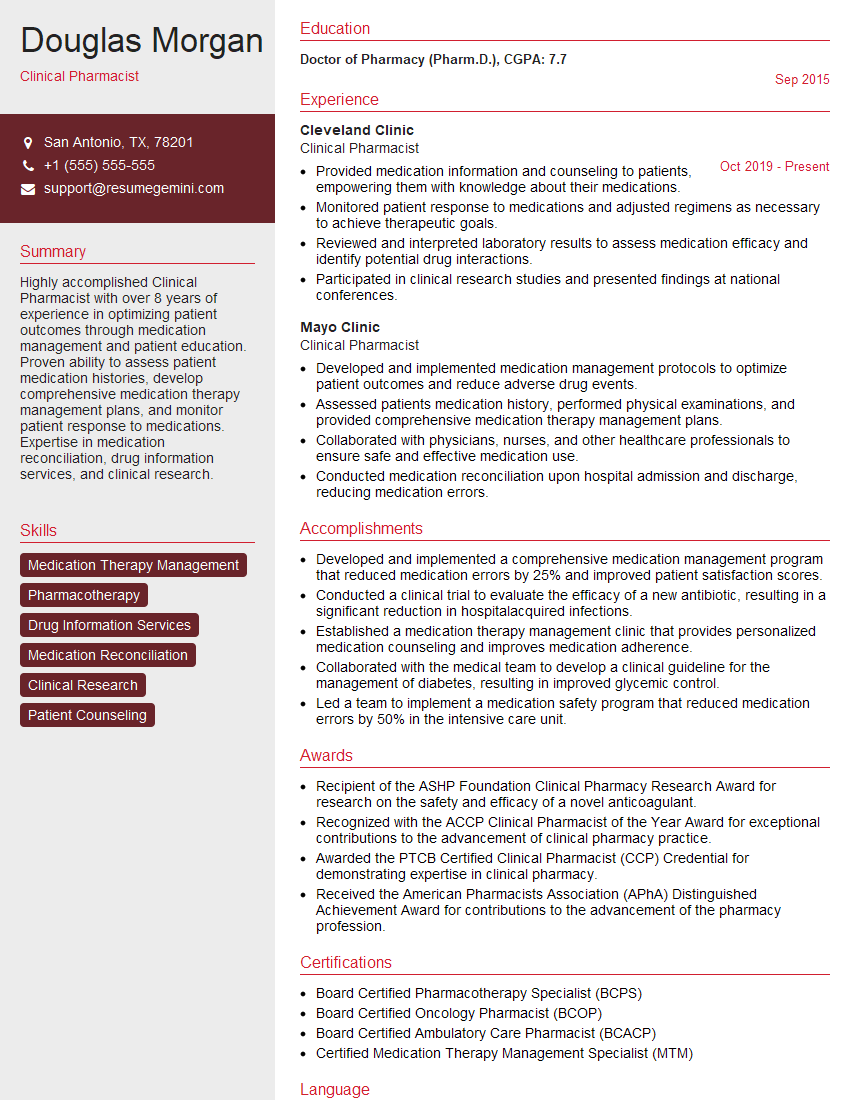
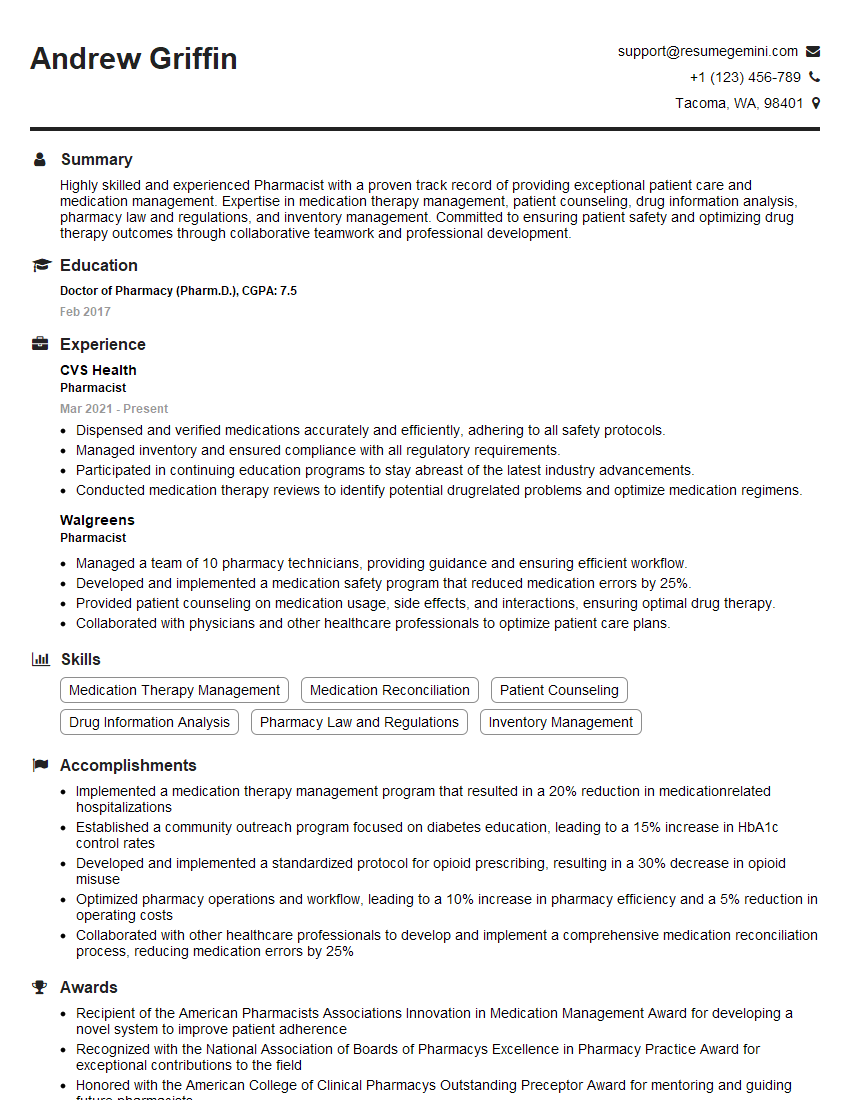
Mastering Medication Monitoring and Interpretation opens doors to exciting career advancements in healthcare, offering opportunities for increased responsibility, specialization, and higher earning potential. To maximize your job prospects, creating a strong, ATS-friendly resume is crucial. ResumeGemini is a trusted resource that can help you build a professional resume that highlights your skills and experience effectively. Examples of resumes tailored to Medication Monitoring and Interpretation are available through ResumeGemini to help you craft a compelling application.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Take a look at this stunning 2-bedroom apartment perfectly situated NYC’s coveted Hudson Yards!
https://bit.ly/Lovely2BedsApartmentHudsonYards
Live Rent Free!
https://bit.ly/LiveRentFREE
Interesting Article, I liked the depth of knowledge you’ve shared.
Helpful, thanks for sharing.
Hi, I represent a social media marketing agency and liked your blog
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?