Cracking a skill-specific interview, like one for Naloxone Administration, requires understanding the nuances of the role. In this blog, we present the questions you’re most likely to encounter, along with insights into how to answer them effectively. Let’s ensure you’re ready to make a strong impression.
Questions Asked in Naloxone Administration Interview
Q 1. Describe the mechanism of action of Naloxone.
Naloxone is an opioid antagonist, meaning it works by reversing the effects of opioid drugs. Opioids bind to specific receptors in the brain and spinal cord, causing decreased pain sensation and slowed breathing. Naloxone competitively binds to these same receptors, blocking the opioids from binding and therefore reversing their effects. Think of it like a key and a lock: the opioid is the key that opens the lock (receptor), causing the opioid effects. Naloxone is a different key that fits the same lock, but it doesn’t open it; instead, it prevents the opioid key from working.
Specifically, Naloxone primarily acts on mu-opioid receptors, which are the primary receptors responsible for the respiratory depression and other central nervous system effects of opioid overdose. By blocking these receptors, Naloxone rapidly reverses the life-threatening respiratory depression caused by opioids.
Q 2. What are the different routes of Naloxone administration?
Naloxone can be administered through several routes, each with its own advantages and disadvantages:
- Intravenous (IV): This is the fastest and most effective route, providing rapid onset of action. It’s typically used in hospital settings or by paramedics.
- Intramuscular (IM): This route is relatively quick and can be used in pre-hospital settings. It’s a good option when IV access isn’t immediately available.
- Intranasal (IN): This route is increasingly common due to its ease of administration and relatively rapid onset of action. It’s a good choice for first responders and bystanders.
- Subcutaneous (SC): This route provides a slower onset of action compared to IV or IM, but can still be effective. It’s less frequently used in acute overdose situations.
The choice of route depends on the circumstances, the individual administering the naloxone, and the availability of resources.
Q 3. What is the appropriate dose of Naloxone for an adult experiencing an opioid overdose?
The appropriate dose of naloxone for an adult experiencing an opioid overdose is typically 0.4 mg to 2 mg administered intravenously, intramuscularly, or intranasally. This may be repeated every 2-3 minutes as needed, until spontaneous respirations return or the patient shows signs of improvement. It’s crucial to follow local protocols and guidelines, as dosing may vary slightly depending on the specific situation and product. For example, some intranasal formulations have different recommended doses.
Important Note: Dosage and frequency are determined by the patient’s response. It is not a one-size-fits-all approach. Continuous monitoring of the patient’s respiratory status and level of consciousness is paramount.
Q 4. What are the potential side effects of Naloxone administration?
Naloxone administration can cause several side effects, most of which are related to the sudden reversal of opioid effects. These can include:
- Withdrawal symptoms: In opioid-dependent individuals, naloxone can trigger acute withdrawal, characterized by symptoms like agitation, anxiety, muscle aches, nausea, vomiting, and sweating. This is because naloxone abruptly removes the opioid from the receptors.
- Increased heart rate and blood pressure: These are common, but usually resolve spontaneously.
- Nausea and vomiting: Often experienced, especially with rapid administration.
- Restlessness and anxiety: These can be distressing for the patient.
The severity of side effects varies depending on the patient’s level of opioid dependence and the dose of naloxone administered. It’s crucial to monitor the patient closely after administering Naloxone and manage these side effects as needed.
Q 5. How would you assess a patient suspected of an opioid overdose?
Assessing a patient suspected of opioid overdose requires a systematic approach, focusing on the ABCs – Airway, Breathing, and Circulation.
- Assess the Airway: Check for patency (is the airway open?). If the patient is unresponsive, establish an airway using appropriate techniques.
- Assess Breathing: Observe the rate, depth, and quality of respirations. Look for signs of respiratory depression, such as slow or shallow breathing, or the absence of breathing.
- Assess Circulation: Check the patient’s pulse and blood pressure. Look for signs of shock, such as pale, cool, and clammy skin.
- Level of Consciousness: Assess the patient’s responsiveness using the AVPU scale (Alert, Verbal, Painful, Unresponsive).
- Pupil Size: Pinpoint pupils (constricted pupils) are a common sign of opioid overdose.
- Vital Signs: Take vital signs, including heart rate, respiratory rate, blood pressure, and oxygen saturation (SpO2).
Based on this assessment, you can determine the need for Naloxone administration and other emergency interventions.
Q 6. What are the signs and symptoms of opioid overdose?
The signs and symptoms of opioid overdose can vary depending on the type and dose of opioid, but generally include:
- Unresponsiveness: Inability to be awakened.
- Slowed or absent breathing: This is a life-threatening sign.
- Pinpoint pupils: Constricted pupils.
- Blue or gray coloring of the skin (cyanosis): Indicates lack of oxygen.
- Gurgling sounds or snoring: Suggests airway obstruction.
- Slow heart rate (bradycardia): Can be a consequence of respiratory depression.
- Low blood pressure (hypotension): Can occur due to circulatory compromise.
- Oversedation: Extreme drowsiness or unresponsiveness.
The presence of multiple of these signs strongly suggests an opioid overdose requiring immediate medical attention.
Q 7. What is the proper technique for administering Naloxone via intramuscular injection?
Administering Naloxone via intramuscular injection requires careful technique to ensure safety and effectiveness:
- Prepare the injection site: Clean the chosen injection site (typically the outer thigh or deltoid muscle) with an antiseptic wipe.
- Select the injection site: Choose a muscle with adequate muscle mass to ensure the medication is properly absorbed.
- Aspirate: Before injecting, aspirate (draw back slightly on the plunger) to ensure you are not in a blood vessel. This step isn’t always done with pre-filled syringes, but it’s considered good practice if possible.
- Inject the medication: Insert the needle at a 90-degree angle into the muscle and slowly inject the medication.
- Remove the needle: Gently remove the needle and apply pressure to the injection site with a sterile gauze pad.
- Dispose of the needle appropriately: Use a sharps container to safely dispose of the needle and syringe.
- Monitor the patient: Closely monitor the patient’s respiratory status and level of consciousness after administering the medication.
It is extremely important that this procedure be performed by someone with proper training and certification. Improper intramuscular injection can cause complications.
Q 8. What is the proper technique for administering Naloxone via intranasal spray?
Administering naloxone intranasally is straightforward but requires precision. First, ensure the patient is lying on their back, or sitting upright if that’s more comfortable and safe. Then, gently tilt their head back slightly. Next, insert the nasal spray tip into one nostril, aiming slightly upwards and towards the back of the nose. Do not obstruct the nostril.
Firmly and steadily depress the spray mechanism, releasing the full dose into the nostril. Repeat the process in the other nostril if the product instructions indicate this.
Important Considerations: Avoid forceful insertion of the applicator which can cause discomfort and bleeding. Observe the patient closely for any signs of respiratory improvement. If there’s no improvement after 2-3 minutes, consider alternative routes of administration (if qualified and appropriate) or seek immediate advanced medical assistance. Remember, always follow the specific instructions provided with the naloxone product.
Q 9. How would you determine the appropriate dose of Naloxone for a pediatric patient?
Determining the appropriate naloxone dose for a pediatric patient is critical and requires careful consideration. There’s no single, universal pediatric dose; it depends on the child’s weight and the severity of the suspected opioid overdose.
Generally, pediatric doses are significantly lower than adult doses. The dose is usually calculated based on weight in kilograms (kg). Always refer to the product-specific instructions and the guidance of local EMS protocols or your medical director. In many cases, emergency medical services (EMS) should be contacted and will determine the dose based on their assessment. Never attempt to guess the dose – an incorrect dose could have serious consequences.
Example: Imagine a 20kg child. A 0.1mg/kg dose would be 2mg of naloxone. However, this is just an example, and the actual dose should be determined by the prescribing physician or as part of a standing order or EMS protocol.
Q 10. What should you do if a patient experiences withdrawal symptoms after receiving Naloxone?
Withdrawal symptoms after naloxone administration are expected in patients who have developed opioid dependence. These symptoms can range from mild discomfort to severe distress. They can include nausea, vomiting, agitation, anxiety, muscle aches, and increased heart rate.
Management: The goal is to provide supportive care and comfort. This might involve providing a calm and reassuring environment, administering antiemetics for nausea, and offering fluids. Severe withdrawal may require further medical intervention, potentially including medications to manage withdrawal symptoms. In some cases, transfer to a specialized facility for detoxification may be necessary.
Important Note: Carefully monitor the patient’s vital signs and respiratory status, as withdrawal can sometimes exacerbate underlying medical conditions. It is imperative to carefully explain to the patient that what they are experiencing is a normal part of opioid withdrawal.
Q 11. How would you document Naloxone administration?
Documentation of naloxone administration is crucial for legal and medical reasons. The documentation should be clear, concise, and accurate. It should include:
- Date and time of administration
- Route of administration (e.g., intranasal, intramuscular)
- Dose administered
- Patient’s response to naloxone (e.g., improved respiratory rate, level of consciousness)
- Any observed withdrawal symptoms
- Vital signs before and after administration
- The name and contact information of the person who administered the naloxone
This information is essential for tracking the effectiveness of the treatment, and to ensure continuity of care should the patient require further medical attention.
Example: In a medical record, it might be documented as: “07/26/2024 14:35: 2mg of Naloxone administered intranasally. Patient’s respiratory rate improved from 6 breaths per minute to 16 breaths per minute. Mild withdrawal symptoms noted, including agitation and diaphoresis.”
Q 12. What are the contraindications for Naloxone administration?
While naloxone is generally safe, there are certain contraindications to consider. There is no absolute contraindication but there are situations where it may not be indicated or requires careful consideration.
- Hypersensitivity: Patients with a known allergy to naloxone should not receive it.
- Uncertain Diagnosis: It is important to carefully consider the likelihood of opioid overdose versus other causes of respiratory depression; use only if opioid overdose is highly suspected
- Severe Cardiovascular Disease: Naloxone withdrawal can result in increased heart rate and blood pressure, therefore, use caution in patients with severe cardiac issues.
In situations where a serious medical problem is suspected, a careful risk-benefit analysis is required before administering naloxone.
Q 13. How would you manage a patient who has received Naloxone but continues to exhibit signs of respiratory depression?
If a patient continues to exhibit signs of respiratory depression despite naloxone administration, it’s a critical situation requiring immediate advanced medical intervention. This could indicate a very large opioid overdose, the presence of other medical issues contributing to respiratory depression, or the need for repeated doses of naloxone.
Actions:
- Maintain Airway: Ensure the airway is patent; begin positive pressure ventilation (PPV) with supplemental oxygen, if needed and trained to do so.
- Repeat Naloxone: Follow appropriate protocols for repeating naloxone doses, if the medication’s instructions and your training allows.
- Activate EMS: Immediately contact Emergency Medical Services (EMS) or other advanced medical support.
- Continuous Monitoring: Closely monitor vital signs, especially heart rate, blood pressure, and respiratory rate.
- Advanced Life Support: Be prepared to initiate advanced cardiac life support (ACLS) if necessary.
This scenario emphasizes the importance of teamwork and rapid response by EMS or other advanced medical personnel.
Q 14. Explain the importance of post-Naloxone administration monitoring.
Post-naloxone administration monitoring is paramount because the effects of naloxone are temporary and the patient’s condition can change rapidly.
Importance:
- Respiratory Status: Continuously monitor respiratory rate, depth, and effort for at least 1-2 hours or longer, depending on the patient’s response and the severity of the overdose.
- Level of Consciousness: Track the patient’s level of consciousness and mental status for any fluctuations.
- Vital Signs: Regularly monitor heart rate, blood pressure, oxygen saturation, and temperature.
Effective post-administration monitoring could save a patient’s life by catching a relapse of respiratory depression before it becomes life-threatening. Continuous observation provides invaluable data for medical professionals in ensuring the patient’s safety and recovery.
Q 15. What are the legal implications of administering Naloxone?
The legal implications of administering naloxone are generally quite favorable, particularly in situations involving suspected opioid overdose. Most jurisdictions have ‘Good Samaritan’ laws or similar legislation that protects individuals from civil liability when they administer naloxone in good faith to someone experiencing an apparent opioid overdose. These laws recognize the urgency of the situation and aim to encourage bystanders to intervene. However, it’s crucial to act responsibly and within the scope of your training. This means administering the naloxone correctly, following established protocols, and seeking immediate medical attention after administration. While legal protection is generally afforded, reckless or negligent administration could still lead to legal repercussions. It’s always advisable to call emergency services immediately after administering naloxone, documenting the situation accurately, and following the instructions provided by the emergency responders. Further, some jurisdictions may require reporting the administration of naloxone to relevant authorities. Consulting with a legal professional is recommended if you have any specific concerns regarding the legal aspects of naloxone administration in your area.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. What is the role of bystanders in assisting with Naloxone administration?
Bystanders play a vital role in saving lives during opioid overdoses. Their quick actions can bridge the gap until professional medical help arrives. Bystanders can recognize the signs of an opioid overdose (unresponsiveness, pinpoint pupils, slow or absent breathing, etc.), call emergency services (911 or your local equivalent), and, if trained, administer naloxone. Even if they aren’t trained in naloxone administration, their presence can offer crucial support and comfort to the individual experiencing an overdose and potentially reassure them. They can provide information about the person’s medical history to paramedics, if known, and help maintain the airway (by positioning the person on their side to prevent choking) until emergency responders arrive. Proper training in CPR and basic first aid can greatly enhance a bystander’s ability to assist. Remember that even the simple act of calling emergency services is a critical first step in a potential overdose situation.
Q 17. Describe your experience administering Naloxone in a real-world scenario.
During my time working as a paramedic, I responded to a call involving a young man who had overdosed on heroin. He was unresponsive, his breathing was shallow and slow, and his pupils were constricted. I immediately assessed the situation, confirming the suspected opioid overdose. My partner called for backup and an ambulance while I prepared and administered a dose of naloxone via intramuscular injection. Within minutes, his respiratory rate improved significantly, and he regained consciousness. He was confused and disoriented, but clearly responding to stimuli. I continued monitoring his vital signs and provided supportive care until the ambulance arrived. This experience reinforced the critical importance of timely naloxone administration and the potential life-saving impact it can have in emergency situations. Post-naloxone administration, it was essential to stay vigilant as the effects of naloxone are temporary, and the patient may relapse. We transported him to the hospital for further observation and treatment.
Q 18. How do you ensure patient safety during and after Naloxone administration?
Ensuring patient safety during and after naloxone administration requires a multi-faceted approach. Before administration, confirming the suspected opioid overdose through a thorough assessment is critical. Administering the naloxone according to the manufacturer’s instructions and appropriate training is paramount. After administration, the patient needs to be closely monitored for several crucial reasons: the effects of naloxone are temporary, the patient may relapse into overdose, and withdrawal symptoms can be severe. Continuous monitoring of vital signs, such as respiration, heart rate, and blood pressure, is crucial. The patient should be positioned to prevent choking (recovery position). Being aware of the potential for aggressive behavior or agitation due to withdrawal is important as well; patient should be approached calmly and with respect. It’s imperative to promptly contact emergency medical services and transport the patient to the hospital for ongoing evaluation and care. Finally, ensuring proper documentation of the entire event is critical for medical and legal purposes.
Q 19. What training and certifications do you possess related to Naloxone administration?
I possess extensive training in advanced cardiac life support (ACLS), basic life support (BLS), and advanced emergency medical technician (AEMT) certifications. My training explicitly covers the recognition, assessment, and management of opioid overdose, including the proper techniques for naloxone administration. I have completed multiple continuing education courses specifically focused on opioid overdose management, naloxone administration, and the implications of Good Samaritan laws. My experience spans numerous real-world scenarios where I’ve successfully administered naloxone and provided post-administration care.
Q 20. Describe a situation where you had to make a quick decision regarding Naloxone administration.
I once encountered a situation where a patient’s breathing was significantly labored, and they were exhibiting signs consistent with an opioid overdose, yet they were only semi-responsive. I had to make a quick decision: while I believed a full overdose was likely given the circumstances, administering naloxone could potentially trigger dangerous withdrawal symptoms due to the patient’s semi-responsive state. After rapid assessment, weighing the potential risks, I elected to administer a small dose of naloxone intravenously. I carefully monitored the response and gave a subsequent dose only after careful evaluation. The immediate response was positive, with respiratory improvement. This highlighted the importance of carefully assessing each patient’s individual presentation and adapting treatment plans based on the severity of the overdose and the patient’s response. Subsequent hospital care confirmed this strategy was effective.
Q 21. What resources do you utilize to stay current on best practices for Naloxone administration?
To stay updated on best practices for naloxone administration, I utilize several key resources. I actively participate in continuing medical education (CME) programs and attend relevant conferences and workshops focusing on emergency medicine and opioid overdose management. I regularly consult peer-reviewed medical journals and publications (such as the Journal of the American Medical Association and the New England Journal of Medicine) which often feature updates and research in this field. I also utilize resources from reputable organizations like the Centers for Disease Control and Prevention (CDC) and the Substance Abuse and Mental Health Services Administration (SAMHSA) which provide guidelines and recommendations on best practices. Staying abreast of these resources is crucial to delivering the most effective and safe care.
Q 22. Explain the difference between Naloxone and other opioid antagonists.
Naloxone is a specific type of opioid antagonist, meaning it reverses the effects of opioid drugs. While other opioid antagonists exist, Naloxone distinguishes itself primarily through its potency, rapid onset of action, and specific targeting of opioid receptors. Other antagonists, like naltrexone, are used for different purposes, such as long-term addiction treatment, and have a slower onset and longer duration of action. Think of it like this: if opioids are a lock, Naloxone is a very strong, fast-acting key designed specifically to unlock it, whereas other antagonists might be weaker keys, or keys that work on a slightly different lock. For example, while nalmefene is another opioid antagonist, it’s used to treat alcohol dependence, not acute opioid overdose, highlighting their distinct roles.
Q 23. How would you respond to a patient or family member’s concerns regarding Naloxone administration?
Addressing concerns about Naloxone administration requires empathy, patience, and clear communication. I would begin by validating their feelings, acknowledging that administering a medication to a loved one can be scary and stressful. Then, I’d explain that Naloxone is a life-saving medication specifically designed to reverse the effects of an opioid overdose; it’s not a cure for addiction, but rather a bridge to medical care. I’d clearly outline the administration process, emphasizing its safety and ease of use (depending on the formulation). Finally, I’d provide resources for addiction treatment and support, reassuring them that help is available. It’s vital to emphasize that administering Naloxone is an act of saving a life, not a judgment on the individual’s choices.
Q 24. What are the storage requirements for Naloxone?
Naloxone storage is crucial for maintaining its effectiveness. Generally, it should be stored at room temperature, protected from light and moisture. The specific storage instructions will depend on the formulation (e.g., nasal spray, auto-injector). Always check the product packaging for precise instructions. Improper storage can degrade the medication, rendering it ineffective in an emergency. Think of it like storing milk—if you don’t keep it cool, it spoils. Similarly, heat and light can damage Naloxone.
Q 25. How would you handle a situation where you suspect a patient is faking an overdose?
Suspecting someone is faking an overdose is a serious consideration, but it shouldn’t deter administering Naloxone if there is any suspicion of opioid involvement. Naloxone is a safe medication, and its administration will not harm someone who doesn’t need it. The potential consequences of not administering Naloxone when it’s needed far outweigh the risk of administering it when it’s not. Therefore, my approach would be to err on the side of caution and administer Naloxone. Simultaneously, I would continue to observe the individual, monitoring for signs of true medical distress. If there is no response, I would seek appropriate medical attention, where the situation can be further assessed and clarified by professionals.
Q 26. What steps would you take if you experience an adverse reaction while administering Naloxone?
Adverse reactions to Naloxone are rare but can include withdrawal symptoms in opioid-dependent individuals (such as nausea, vomiting, restlessness, and increased heart rate). If I were to observe an adverse reaction, my first step would be to ensure the patient’s airway is clear and they are breathing adequately. I would then carefully monitor their vital signs, paying close attention to their respiratory rate and heart rate. Depending on the severity of the reaction, I would provide supportive care as needed, which may include oxygen supplementation and managing any pain or discomfort. I would immediately seek medical assistance, providing a detailed account of the situation to the emergency medical responders.
Q 27. Discuss the ethical considerations involved in administering Naloxone.
Administering Naloxone involves several ethical considerations. The primary ethical imperative is the preservation of life. It’s a duty to act when someone is in a life-threatening situation, even if it means intervening without their explicit consent. However, respect for autonomy should also be considered. While saving a life is paramount, after stabilizing the patient, exploring their reasons for opioid use and offering appropriate support, rather than judgment, is crucial. In the case of minors, parental consent is usually required before medical intervention, but in a life-threatening situation, saving their life is a priority. Confidentiality must also be maintained, adhering to all privacy laws and guidelines.
Q 28. How do you remain calm and focused during a high-pressure situation involving an opioid overdose?
Maintaining composure during a high-pressure situation like an opioid overdose requires preparation and training. I rely on systematic approaches and pre-planned protocols. Having a clear mental checklist of steps to follow helps streamline the process, ensuring nothing is missed. Deep breathing exercises can help manage stress and anxiety. Communicating clearly and calmly with the patient, bystanders, and emergency medical services is crucial. Remember that focusing on the immediate task—administering Naloxone and ensuring the person’s safety—keeps my actions centered and avoids being overwhelmed by the stressful environment.
Key Topics to Learn for Naloxone Administration Interview
- Understanding Opioid Overdose: Recognizing the signs and symptoms of an opioid overdose, differentiating between opioid overdose and other medical emergencies.
- Naloxone Pharmacology: Mechanism of action, onset of effect, duration of action, potential side effects and their management.
- Administration Routes and Techniques: Intranasal, intramuscular, intravenous administration – proper techniques, dosages, and considerations for each route.
- Patient Assessment and Monitoring: Performing a rapid assessment of the patient’s respiratory status, level of consciousness, and vital signs before, during, and after Naloxone administration.
- Post-Administration Care: Monitoring the patient for recurrence of symptoms, ensuring appropriate medical follow-up, and documenting the entire event.
- Legal and Ethical Considerations: Understanding the legal implications of administering Naloxone, maintaining patient confidentiality, and adhering to relevant regulations and guidelines.
- Recognizing Contraindications and Precautions: Identifying situations where Naloxone administration might be contraindicated or require careful consideration.
- Emergency Response and Teamwork: Effective communication and collaboration with emergency medical services (EMS) and other healthcare professionals.
- Documentation and Reporting: Accurate and complete documentation of the Naloxone administration event, including patient response and any complications.
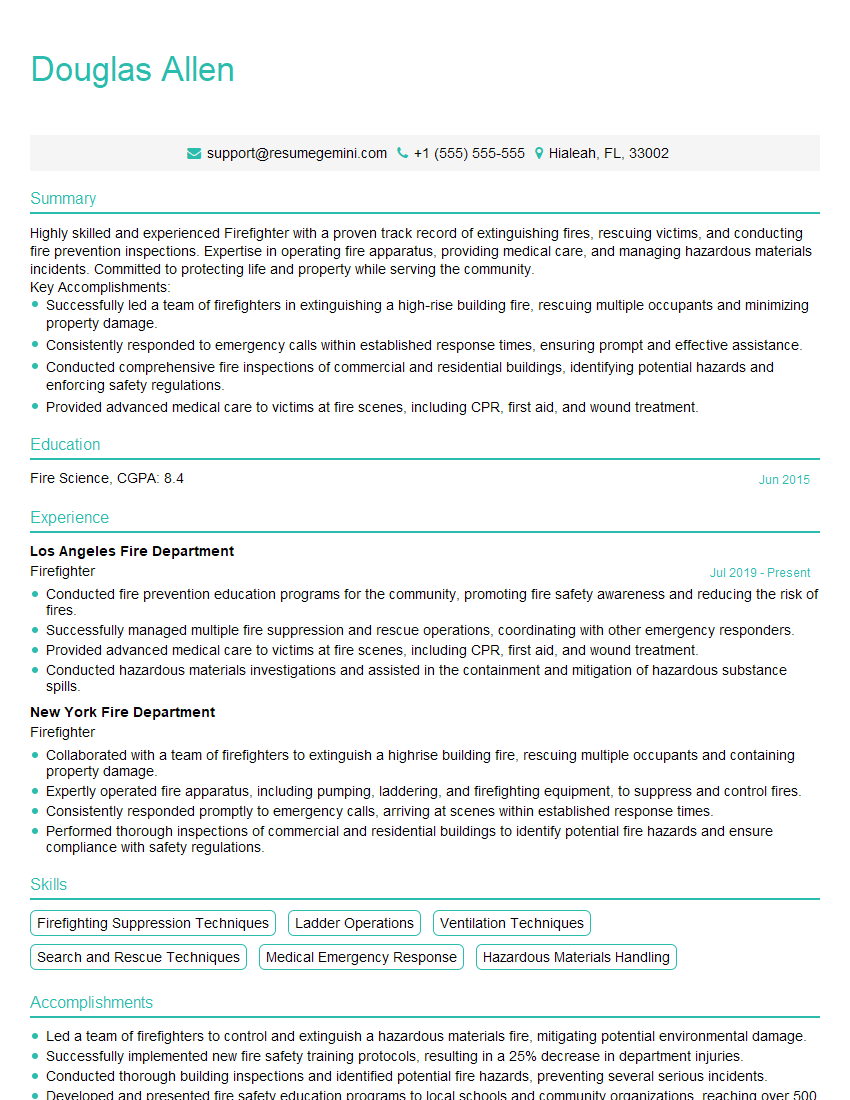
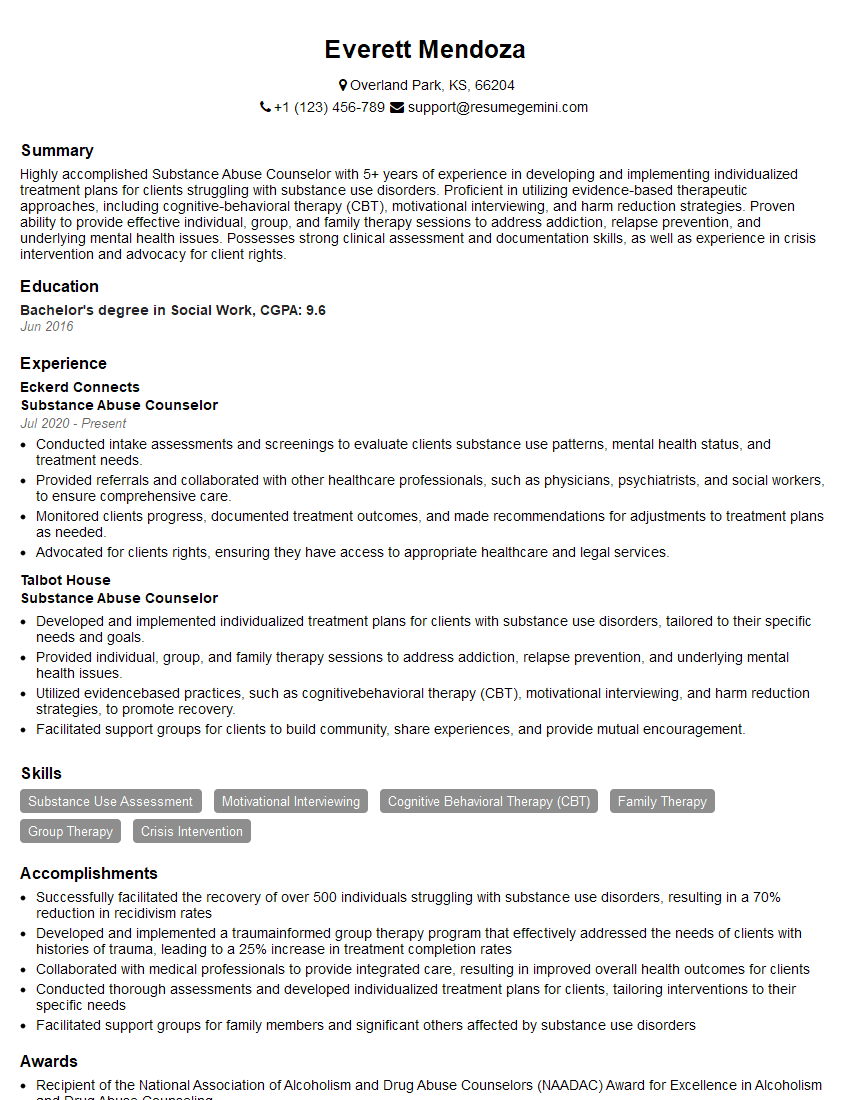
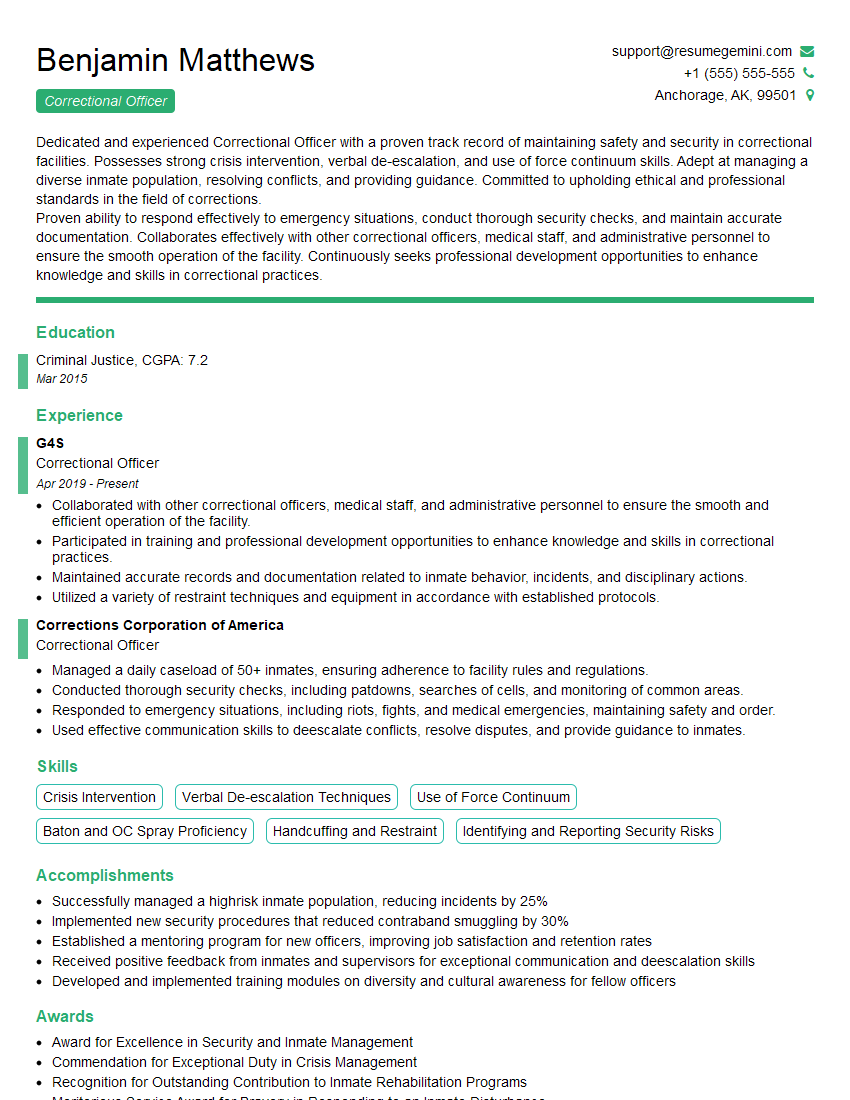
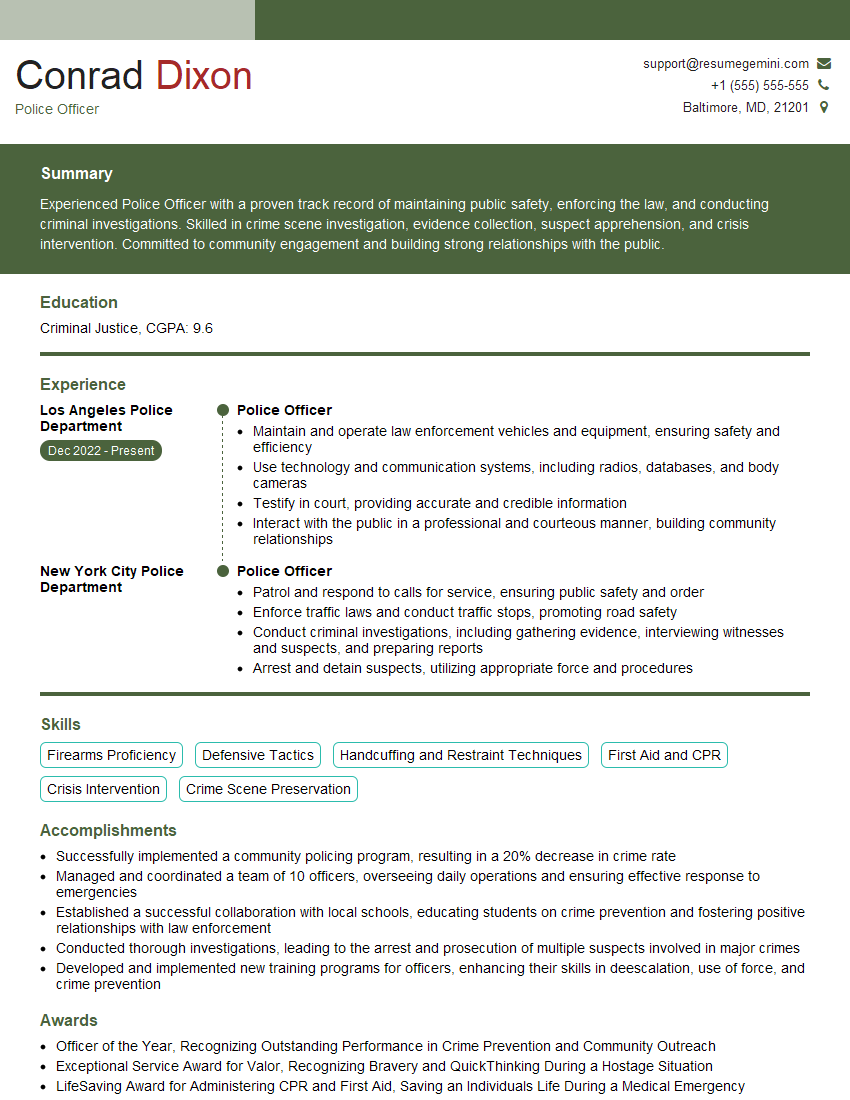
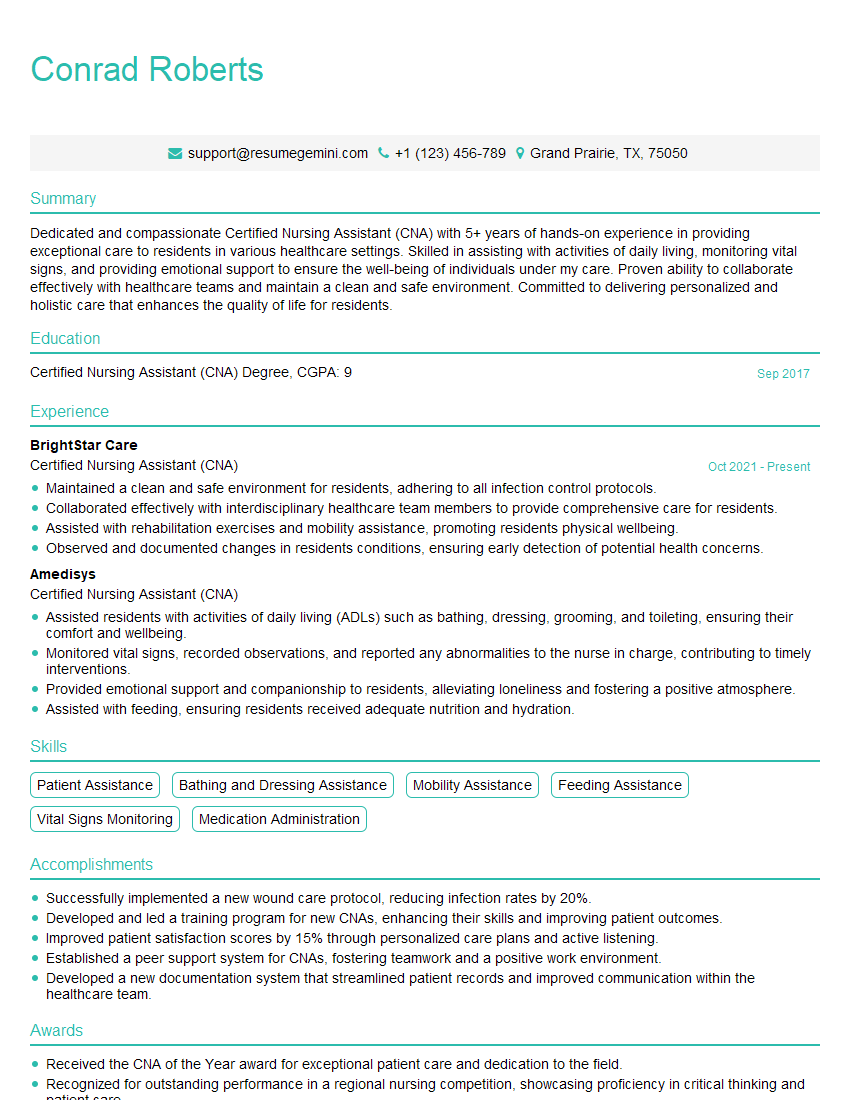
Next Steps
Mastering Naloxone administration demonstrates a crucial skillset highly valued in today’s healthcare landscape, opening doors to diverse and rewarding career opportunities. A strong resume is essential to showcasing this expertise effectively. Creating an ATS-friendly resume increases your chances of getting your application noticed. To help you build a compelling and professional resume, we recommend using ResumeGemini, a trusted resource for crafting impactful career documents. Examples of resumes tailored to Naloxone Administration are available to guide you.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Interesting Article, I liked the depth of knowledge you’ve shared.
Helpful, thanks for sharing.
Hi, I represent a social media marketing agency and liked your blog
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?