Interviews are opportunities to demonstrate your expertise, and this guide is here to help you shine. Explore the essential Patient Interaction and Confidentiality interview questions that employers frequently ask, paired with strategies for crafting responses that set you apart from the competition.
Questions Asked in Patient Interaction and Confidentiality Interview
Q 1. Explain the importance of maintaining patient confidentiality.
Maintaining patient confidentiality is paramount for several reasons. It’s a cornerstone of ethical medical practice, building trust between patients and healthcare providers. This trust encourages patients to be open and honest about their health, leading to more accurate diagnoses and effective treatment. Without confidentiality, individuals might hesitate to seek care, fearing their private information will be misused or disclosed inappropriately. Legally, breaching confidentiality can have serious consequences, including lawsuits and loss of professional license.
- Protecting Privacy: Sensitive medical information, including diagnoses, treatments, and personal details, must be shielded from unauthorized access.
- Building Trust: Patients are more likely to share crucial information when they feel confident their privacy will be respected.
- Legal Compliance: Various regulations, such as HIPAA in the US, mandate the protection of patient data.
Imagine a patient hesitant to disclose a sensitive mental health issue because they fear their employer might find out. Confidentiality ensures they feel safe sharing this crucial information.
Q 2. Describe your understanding of HIPAA regulations.
HIPAA, the Health Insurance Portability and Accountability Act of 1996, is a US law designed to protect the privacy and security of patients’ health information. It establishes strict guidelines for the use, disclosure, and safeguarding of Protected Health Information (PHI). PHI includes any individually identifiable health information, such as medical records, billing information, and even conversations about a patient’s health. HIPAA outlines specific requirements for covered entities, including healthcare providers, health plans, and healthcare clearinghouses.
- Privacy Rule: Sets limits on the use and disclosure of PHI and gives patients rights over their health information.
- Security Rule: Requires covered entities to implement administrative, physical, and technical safeguards to protect electronic PHI.
- Breach Notification Rule: Specifies how covered entities must handle and report breaches of unsecured PHI.
For example, under HIPAA, a doctor cannot disclose a patient’s HIV status to their family without the patient’s consent, unless legally required. This highlights the stringent regulations around protecting sensitive health data.
Q 3. How would you handle a situation where a patient requests their medical records?
When a patient requests their medical records, I would first verify their identity through secure methods. Then, I would explain the process of accessing their records, including any associated fees, if applicable. I would also ensure they understand their rights regarding their health information, as outlined by HIPAA (or relevant legislation in other jurisdictions). I would then process their request efficiently, ensuring compliance with all relevant regulations and policies. If there are any parts of the record that are legally restricted from release, I would discuss those limitations with the patient, explaining the rationale clearly and respectfully.
For instance, if a patient requested their psychotherapy notes, I would clearly explain that there might be limitations based on privacy regulations and the nature of the content. I’d respect their requests while ensuring adherence to all legal and ethical guidelines.
Q 4. How would you respond to a colleague who accidentally disclosed patient information?
If a colleague accidentally disclosed patient information, my response would depend on the severity and nature of the disclosure. First, I would address the situation privately with my colleague, emphasizing the seriousness of the breach and the potential consequences. I would help them understand the implications of their actions and guide them towards reporting the incident according to the established protocol (usually involving the organization’s compliance department or designated authority). I would also offer support and guidance on preventing similar incidents in the future, focusing on education and reinforcing confidentiality protocols. Reporting the breach appropriately would be crucial, regardless of the colleague’s intent.
If the breach involved sensitive information and posed significant risk to the patient, I’d collaborate with the necessary authorities to ensure the patient is notified and appropriate actions are taken to mitigate the harm caused.
Q 5. What strategies do you employ to build rapport with patients?
Building rapport with patients is essential for effective healthcare. I employ several strategies: Active listening, demonstrating empathy, using clear and respectful communication, and creating a comfortable and safe environment. I make a conscious effort to understand the patient’s perspective, their concerns, and their individual needs. I also ensure clear and concise communication, avoiding medical jargon whenever possible. Nonverbal cues like maintaining eye contact and using a warm, friendly tone also contribute to building trust and a positive interaction.
For instance, beginning a consultation by asking the patient about their day or their hobbies, before delving into the medical reason for their visit, can make them feel more at ease and improve communication.
Q 6. Describe your experience handling patient inquiries and complaints.
I have extensive experience handling patient inquiries and complaints. My approach involves active listening, empathy, and a commitment to finding fair and effective resolutions. I strive to understand the patient’s concerns thoroughly, acknowledging their feelings and perspectives. If the complaint is justified, I work collaboratively with the patient to address the issue promptly and effectively. I document all interactions carefully and follow established protocols for managing complaints and feedback, ensuring that concerns are escalated appropriately when needed. I also strive to learn from every interaction, constantly refining my communication skills and approach to ensure all patients feel heard and valued.
For instance, if a patient complains about a long wait time, I would first apologize, explain the reason for the delay (if possible), and offer solutions to alleviate the situation in the future. This approach helps transform a negative experience into a more positive one.
Q 7. How would you communicate complex medical information to a patient in a clear and understandable manner?
Communicating complex medical information requires clear, concise language, avoiding jargon. I tailor my explanation to the patient’s educational level and understanding. I use visual aids, like diagrams or models, whenever appropriate. I encourage the patient to ask questions and ensure they understand the information before concluding the discussion. I use analogies and relatable examples to illustrate complex concepts. Finally, I provide written materials summarizing the key points discussed, ensuring the patient has access to the information later.
For example, explaining a complex heart condition might involve using a simplified diagram of the heart, pointing out the affected areas, and then comparing the condition to a familiar example, such as a blocked pipe affecting water flow.
Q 8. Explain the process of obtaining informed consent from a patient.
Obtaining informed consent is a crucial ethical and legal process ensuring patients understand and agree to medical interventions or research participation. It’s not merely a signature on a form; it’s an ongoing dialogue.
- Explanation of the Procedure: I begin by explaining the proposed treatment, procedure, or research in clear, non-medical terms, ensuring the patient understands the benefits, risks, alternatives, and potential consequences of refusing. I check for understanding at each step, using plain language and avoiding jargon. I answer all questions thoroughly and patiently.
- Addressing Capacity: I assess the patient’s decision-making capacity. This involves verifying their understanding of the information, their ability to reason, and their ability to express their wishes. If capacity is questionable, I consult with colleagues, family members (with patient consent), or legal guardians.
- Documenting Consent: Once the patient gives their voluntary consent, the process is meticulously documented. This includes the date, time, a summary of the discussion, confirmation of the patient’s understanding, and the patient’s signature (or a witness’s signature if the patient is unable to sign). I ensure the patient receives a copy of the consent form.
Example: Imagine a patient needing surgery. I wouldn’t just present them with a consent form. I would explain the procedure step-by-step, including the potential risks (bleeding, infection), benefits (pain relief, improved mobility), and alternatives (physical therapy). I’d encourage questions and address any concerns before obtaining their informed consent.
Q 9. How would you manage a situation where a patient is upset or agitated?
Managing an upset or agitated patient requires a calm, empathetic approach. My primary goal is to de-escalate the situation and ensure the patient feels heard and understood.
- Active Listening: I’d start by actively listening to the patient’s concerns without interrupting. I’d use verbal and non-verbal cues (nodding, maintaining eye contact) to show I’m engaged.
- Validation and Empathy: I’d validate their feelings, even if I don’t agree with their perspective. For instance, I might say, “I understand you’re feeling frustrated,” or “That sounds incredibly difficult.”
- Reframing and Clarification: I would try to understand the root cause of their agitation. Often, miscommunication or misunderstanding lies at the heart of the problem. I’d clarify any confusion and reframe the situation in a positive and reassuring manner.
- Collaboration and Solutions: I’d involve the patient in finding solutions to their concerns. This could involve adjusting treatment plans, offering additional resources, or connecting them with appropriate support services.
- Setting Boundaries: In cases of extreme agitation or aggression, I’d prioritize safety and set clear boundaries. This may involve seeking assistance from security or other medical personnel.
Example: If a patient is upset about a long wait time, I wouldn’t dismiss their feelings. I’d apologize for the inconvenience, explain the reason for the delay, and offer them options like rescheduling or providing them with updates.
Q 10. How do you ensure the accuracy and integrity of patient data?
Ensuring the accuracy and integrity of patient data is paramount. This involves a multi-faceted approach incorporating rigorous processes and technologies.
- Data Entry Protocols: We follow strict protocols for data entry, including double-checking information and using standardized terminologies. This minimizes errors and ensures consistency.
- Regular Audits and Validation: We conduct regular audits and data validation checks to identify and correct any inconsistencies or inaccuracies. This helps maintain data quality over time.
- Data Security Measures: We implement robust security measures, such as access controls, encryption, and regular security updates, to protect patient data from unauthorized access, use, or disclosure.
- Staff Training: All staff members receive comprehensive training on data handling procedures, including HIPAA compliance, data privacy, and best practices for data entry and management.
- Error Correction Procedures: We have clear procedures for correcting errors, documenting corrections, and tracking changes made to patient data. This allows for transparency and accountability.
Example: If a data entry error is discovered, we follow a specific procedure to correct the error, document the correction, and notify relevant parties. The correction and the reason for it are clearly recorded in the patient’s record, preserving audit trail integrity.
Q 11. Describe your experience working with electronic health records (EHRs).
I have extensive experience working with Electronic Health Records (EHRs), specifically using [mention specific EHR system, e.g., Epic, Cerner]. My experience encompasses data entry, retrieval, and analysis. I am proficient in using EHR systems to access patient medical history, including medications, allergies, lab results, imaging reports, and progress notes.
- Data Entry and Management: I am skilled in accurately and efficiently entering patient data into the EHR system, ensuring completeness, accuracy, and compliance with all relevant regulations.
- Information Retrieval: I am adept at quickly and efficiently retrieving relevant patient information from the EHR system to support clinical decision-making and patient care.
- Reporting and Analysis: I utilize the reporting and analytics capabilities of the EHR system to generate reports, analyze trends, and identify areas for improvement in patient care.
- Integration with Other Systems: I am familiar with integrating EHR systems with other healthcare information systems, such as pharmacy systems and laboratory information systems, to ensure seamless data flow and reduce redundancies.
Example: During a patient’s appointment, I use the EHR to quickly review their medical history, identify any potential medication interactions, and ensure that all necessary information is readily available for the physician.
Q 12. How would you handle a situation where you suspect a breach of patient confidentiality?
Suspecting a breach of patient confidentiality is a serious matter requiring immediate action.
- Report Immediately: I would immediately report my suspicions to my supervisor and the appropriate authorities within the healthcare organization, according to established protocols.
- Document Everything: I would meticulously document all relevant details, including the nature of the suspected breach, the date, time, individuals involved (if known), and any evidence supporting the suspicion.
- Follow Established Procedures: I would strictly adhere to all established procedures for handling suspected breaches of confidentiality, including cooperating fully with internal and external investigations.
- Maintain Confidentiality: Until the investigation is complete, I would maintain strict confidentiality about the suspected breach, discussing it only with authorized individuals involved in the investigation.
Example: If I discovered a colleague accessing patient records without a legitimate medical reason, I would report this immediately to my supervisor, providing all the relevant details.
Q 13. What is your understanding of protected health information (PHI)?
Protected Health Information (PHI) encompasses any individually identifiable health information held or transmitted by a covered entity or its business associate, in any form or media, whether electronic, paper, or oral. This includes a broad range of data that can be used to identify an individual and relate to their past, present, or future physical or mental health, or provision of healthcare.
- Examples of PHI: Names, addresses, social security numbers, medical record numbers, dates of birth, medical history, diagnoses, test results, insurance information, and any other information that could reasonably be used to identify an individual.
- HIPAA Compliance: My understanding of PHI is deeply rooted in HIPAA (Health Insurance Portability and Accountability Act) regulations, which strictly govern the use, disclosure, and protection of PHI. Strict adherence to HIPAA rules is essential in safeguarding patient privacy.
Example: A patient’s name, date of birth, and diagnosis of diabetes would all constitute PHI. The information is individually identifiable and relates to their health status.
Q 14. How would you address a patient’s concerns regarding their privacy?
Addressing a patient’s concerns about their privacy involves a combination of empathy, transparency, and education.
- Listen and Empathize: I would begin by actively listening to their concerns without interrupting and validating their feelings. I would make them feel heard and understood.
- Explain Privacy Policies and Procedures: I would clearly explain our organization’s privacy policies and procedures, focusing on how their information is protected and used. I would use plain language, avoiding jargon.
- Answer Questions Thoroughly: I would answer all their questions thoroughly and honestly, ensuring they understand how their data is handled and used. I would correct any misunderstandings.
- Provide Resources: If necessary, I would provide them with additional resources, such as written materials or contact information for the privacy officer.
- Follow Up: I would follow up with the patient to ensure their concerns have been addressed and they feel comfortable with the way their information is handled.
Example: If a patient expresses concern about their data being shared with insurance companies, I would explain the limits of data sharing mandated by HIPAA, and what specific information is shared with insurance providers for billing purposes.
Q 15. Explain your understanding of the different levels of patient information access.
Patient information access is tiered to ensure appropriate levels of confidentiality and security. Access is typically determined by an individual’s role and their need to know. This is often dictated by legal frameworks like HIPAA (in the US) or similar regulations in other countries.
- Restricted Access: This level is reserved for the patient themselves and authorized healthcare professionals directly involved in their care (e.g., treating physician, nurses directly involved in care). This might include viewing medical records, test results, and treatment plans.
- Limited Access: This level grants access to individuals who need specific pieces of information for administrative or billing purposes. For example, billing personnel might need access to insurance information but not detailed medical history. This access is strictly controlled and audited.
- Administrative Access: This level might be granted to IT staff or system administrators responsible for maintaining the electronic health records system. This access is typically controlled and requires strong security protocols, including audit trails to track all actions. They have access to the structure of the system but not to the individual patient information unless for essential IT maintenance tasks, such as system troubleshooting.
Think of it like a multi-level security building. Only those with appropriate clearance can access specific floors, and their movement is carefully monitored.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How would you maintain confidentiality in a busy healthcare environment?
Maintaining confidentiality in a busy healthcare setting requires a multi-pronged approach, encompassing both physical and procedural safeguards. It’s about building a culture of privacy.
- Physical Security: Secure areas for storing and accessing patient records, limiting access to authorized personnel only, using locked filing cabinets, and ensuring computers are password-protected and logged out when unattended.
- Procedural Security: Implementing strict protocols for handling patient information, such as shredding confidential documents before disposal, using secure messaging for electronic communication, and regularly reviewing and updating security protocols. This also includes conducting regular training for all staff on confidentiality policies and best practices.
- Communication Protocols: Never discussing patients in public areas, using appropriate terminology when referring to patients (avoiding using patient identifiers in public spaces), and adhering strictly to ‘need-to-know’ principles when sharing patient information.
- Technological Safeguards: Using secure electronic health record systems with robust access control, data encryption, and audit trails. Implementing strong password policies and regular security updates.
For instance, in a previous role, we implemented a ‘whisper room’ for discussing sensitive patient information, ensuring conversations weren’t overheard. We also regularly audited access logs to our electronic system to identify and address potential breaches.
Q 17. How do you ensure patient privacy when using technology (e.g., email, phone)?
Protecting patient privacy when using technology necessitates a proactive and cautious approach. The key is to treat all electronic communications as if they are paper records.
- Email: Never send protected health information (PHI) via unencrypted email. Instead, use secure messaging systems provided by your healthcare organization, or HIPAA-compliant email services if necessary. Only include necessary information in the email, and always verify the recipient’s email address before sending.
- Phone: Avoid discussing sensitive patient details in public places or on speakerphone. When leaving a voicemail message, avoid mentioning the patient’s name or other identifying information. Use secure methods of communication for discussing PHI, such as encrypted phone calls.
- Technology Security: Use strong, unique passwords, and enable two-factor authentication where available. Ensure all devices are updated with the latest security patches and that appropriate anti-virus and anti-malware software is installed. Report any suspected security breaches immediately.
- HIPAA Compliance: Ensure you adhere to all applicable HIPAA rules and regulations, including those concerning electronic protected health information (ePHI).
Imagine you’re sending a highly sensitive document via postal mail—you’d ensure it’s sealed properly and sent securely. The same principle applies to electronic communication.
Q 18. Describe a time you had to deal with a difficult or challenging patient interaction.
I once encountered a patient who was extremely agitated and distrustful of the healthcare system due to a past negative experience. He refused treatment and became verbally abusive.
My approach involved remaining calm and empathetic, actively listening to his concerns without interrupting. I validated his feelings, acknowledged his past experience, and explained the benefits of the treatment in simple, non-judgmental terms. I also sought support from a colleague and, with their assistance, we were able to slowly build a rapport with him, eventually persuading him to accept the necessary care.
This experience taught me the importance of patience, empathy, and teamwork in managing challenging patient interactions. It highlighted the need to approach each patient with an understanding of their unique background and perspective.
Q 19. How do you prioritize patient needs while balancing multiple tasks?
Prioritizing patient needs while managing multiple tasks requires a structured approach that combines efficient task management with a patient-centric focus.
- Prioritization Matrix: I use a prioritization matrix (e.g., Urgent/Important matrix) to categorize tasks based on their urgency and impact on patient care. Tasks directly related to patient safety or immediate needs always take precedence.
- Time Management Techniques: Employing time management techniques like time blocking, the Pomodoro Technique, and delegation (where appropriate) to ensure that tasks are completed efficiently and effectively.
- Communication & Collaboration: Open communication with colleagues is vital. If I am overwhelmed, I proactively communicate my workload and seek support to ensure all patients receive timely and appropriate care. This includes clarifying patient needs and roles with team members.
- Flexibility and Adaptability: Being flexible and adaptable is key. Unexpected situations frequently arise, and the ability to adjust priorities based on changing circumstances is crucial.
For instance, if I had a patient requiring immediate attention and another patient with a less urgent need, I would address the immediate need first, then transition to the other once the critical need is addressed. This ensures patient safety and provides equitable care.
Q 20. How do you handle sensitive or emotionally charged patient situations?
Handling sensitive or emotionally charged situations requires a blend of professional skills and empathy. The goal is to create a safe space for patients to express themselves.
- Active Listening: Giving patients undivided attention, listening without judgment, and using verbal and nonverbal cues to show empathy and understanding.
- Validation: Acknowledging the patient’s feelings and validating their experience, even if you don’t necessarily agree with their perspective. This helps create a connection and trust.
- Emotional Regulation: Maintaining emotional composure and professional demeanor, even in highly stressful situations. This helps de-escalate the situation and prevents it from further escalating.
- Referral: Referring patients to appropriate resources, such as social workers, counselors, or support groups, when needed. Recognizing the limits of your role and ensuring the patient receives comprehensive care.
In one instance, I had a patient who was deeply distressed after receiving a difficult diagnosis. I allowed them to express their feelings without interruption, validated their grief, and offered them emotional support, connecting them with the hospital’s social work team for further assistance.
Q 21. Describe your experience with patient education and support.
Patient education and support are integral to providing high-quality care. It empowers patients to take an active role in managing their health.
- Needs Assessment: I begin by assessing the patient’s understanding of their condition, treatment plan, and potential risks and benefits. I tailor my approach to their educational level and learning style.
- Clear and Concise Communication: Using simple, non-medical language, avoiding jargon, and providing written materials to reinforce key points. This ensures that information is readily understood and retained.
- Interactive Methods: Incorporating interactive methods like diagrams, videos, or demonstrations to enhance understanding and engagement.
- Follow-up and Support: Providing opportunities for questions and follow-up, ensuring that patients feel comfortable contacting me or other members of the care team with any concerns.
- Resource Provision: Connecting patients with relevant resources, such as support groups, online information, or community services.
For example, I created a series of easy-to-understand brochures for patients newly diagnosed with diabetes, covering topics such as medication management, diet, and exercise. I also organized a support group for them to connect with each other and share their experiences. This provided a holistic approach to patient education and support, enabling better health management.
Q 22. How would you explain a complex medical procedure to a patient with limited medical knowledge?
Explaining complex medical procedures to patients with limited medical knowledge requires clear, concise communication and a patient-centered approach. I avoid using medical jargon and instead use analogies and simple language. I break down the procedure into smaller, manageable steps, using visual aids like diagrams or models whenever possible. I encourage questions and ensure the patient understands the procedure’s purpose, benefits, risks, and potential alternatives.
For example, if explaining a coronary angioplasty, I would say something like, “Imagine your heart’s arteries are like garden hoses. If they become clogged, blood flow is restricted. This procedure is like using a tiny balloon to clear the blockage, allowing blood to flow freely again.” I would then explain the steps involved – the catheter insertion, balloon inflation, and stent placement – in simple terms, using the garden hose analogy to illustrate each step.
I always confirm understanding by asking the patient to explain the procedure in their own words. This ensures comprehension and allows me to address any remaining concerns or misunderstandings.
Q 23. What measures do you take to prevent errors related to patient identification?
Preventing errors related to patient identification is paramount. My approach involves a multi-layered strategy. First, I always use at least two patient identifiers before providing any care or treatment. This typically includes checking the patient’s name and date of birth against their identification bracelet. Second, I visually confirm the patient’s identity, comparing it to the information on the bracelet and medical record. Third, I utilize electronic health record (EHR) systems that incorporate barcode scanning or other technologies for positive patient identification.
For example, before administering medication, I would check the patient’s name and date of birth on their bracelet and compare it to the information on the medication label and the EHR, and visually confirm that I am giving medication to the correct patient. In situations involving high-risk procedures, such as surgery, I would involve a second healthcare professional in the verification process to ensure there are no discrepancies.
Q 24. How would you respond to a request for information that falls outside your scope of practice?
When a patient requests information that falls outside my scope of practice, I acknowledge their request and explain, in a respectful and understanding manner, why I cannot directly provide the answer. I emphasize that I value their inquiry and am committed to helping them find the right resources. I then connect them with the appropriate healthcare professional who can address their concern. This might involve directing them to a specialist, referring them to a reliable source of medical information, or suggesting that they discuss the matter with their physician.
For example, if a patient asks about a complex genetic disorder that is beyond my area of expertise, I would explain that I am not qualified to answer their questions but would be happy to help them schedule an appointment with a geneticist who can provide accurate and detailed information.
Q 25. Describe your experience with documenting patient interactions and care.
Throughout my career, I have consistently maintained meticulous documentation of patient interactions and care. I use the SOAP (Subjective, Objective, Assessment, Plan) method or similar structured documentation format. This ensures clear and concise recording of all relevant information. The subjective section includes the patient’s statements and concerns; the objective section documents measurable findings such as vital signs and test results; the assessment section outlines my clinical judgment based on these findings, and the plan details the treatment plan and subsequent steps.
My documentation always adheres to HIPAA guidelines, ensuring patient confidentiality and data security. I ensure my notes are factual, accurate, legible, complete, timely and concise. I avoid using subjective interpretations or assumptions, focusing instead on observable facts and the patient’s own words. In addition, I always utilize the approved EHR system, regularly review, and amend my notes as needed. I also utilize secure messaging for communicating with colleagues and specialists, thereby maintaining patient confidentiality within the scope of practice.
Q 26. How do you ensure patient satisfaction in your interactions?
Ensuring patient satisfaction involves building rapport, actively listening, and demonstrating empathy and respect. I start by addressing the patient by their preferred name and introducing myself clearly. I make a conscious effort to make eye contact, maintain a calm demeanor, and actively listen to their concerns. I explain procedures and treatments clearly, using simple language and avoiding medical jargon. I offer them choices whenever possible, empowering them to participate in their care. And I always check in to see if they have any questions or concerns throughout our interactions.
For instance, if a patient is anxious about a procedure, I take the time to address their concerns, answer their questions patiently, and provide reassurance. If there’s a long wait time, I proactively communicate the situation, apologizing for any inconvenience. I regularly ask them how I can improve, and try to implement those changes in my future interactions.
Q 27. How do you adapt your communication style to meet the needs of different patients?
Adapting my communication style to meet the needs of diverse patients is essential. I consider factors such as age, cultural background, language proficiency, and cognitive abilities. For older adults, I may need to speak more slowly and clearly and use larger font sizes on any written material. With patients who have limited English proficiency, I may need to use a translator or utilize simple, universal gestures. For children, I would use age-appropriate language, playful communication strategies, and engage them actively throughout the conversation. I always consider visual impairments, hearing impairments, cognitive limitations and adjust accordingly.
For instance, with a patient who is hard of hearing, I would make sure to face them directly, speak clearly and slowly, and reduce background noise. With a visually impaired patient, I would provide detailed verbal descriptions.
Q 28. Describe a time you had to advocate for a patient’s rights or needs.
In a previous role, I advocated for a patient who was repeatedly denied necessary pain medication despite significant reports of post-surgical pain. The physician attributed the pain to psychological factors without thoroughly investigating the patient’s physical condition. I noticed inconsistencies in the documentation and the patient’s obvious distress. I documented the patient’s symptoms meticulously, gathered supporting evidence from nursing staff, and respectfully but firmly expressed my concerns to the physician and the medical director. I emphasized the patient’s right to appropriate pain management and highlighted the ethical implications of inadequate pain control.
Through persistent advocacy and detailed documentation of my observations, I successfully ensured the patient received a thorough assessment and appropriate pain medication, alleviating their suffering and improving their overall well-being. This experience reinforced the importance of patient advocacy, meticulous documentation, and interprofessional collaboration in ensuring optimal patient care.
Key Topics to Learn for Patient Interaction and Confidentiality Interview
- Effective Communication Techniques: Mastering active listening, clear and concise verbal and non-verbal communication, adapting your approach to diverse patient populations, and handling difficult conversations with empathy and professionalism.
- HIPAA Compliance and Legal Frameworks: Understanding the core principles of HIPAA, patient rights related to privacy, and the legal implications of confidentiality breaches. This includes practical application of these regulations in everyday scenarios.
- Building Rapport and Trust: Developing strategies to create a safe and comfortable environment for patients, fostering open communication, and understanding the importance of building trust through respectful interactions.
- Conflict Resolution and De-escalation: Techniques for managing challenging patient interactions, addressing complaints effectively, and de-escalating potentially volatile situations while maintaining patient confidentiality.
- Documentation and Record Keeping: Understanding best practices for accurate, concise, and confidential documentation of patient interactions, including electronic health record (EHR) systems and data security protocols.
- Ethical Considerations: Exploring ethical dilemmas related to patient confidentiality, such as disclosing information to mandated reporters or handling requests for information from unauthorized individuals. Understanding the balance between patient privacy and legal obligations.
- Cultural Sensitivity and Awareness: Recognizing and respecting diverse cultural backgrounds and beliefs that may impact patient communication and healthcare preferences. Applying culturally sensitive communication strategies in diverse patient interactions.
Next Steps
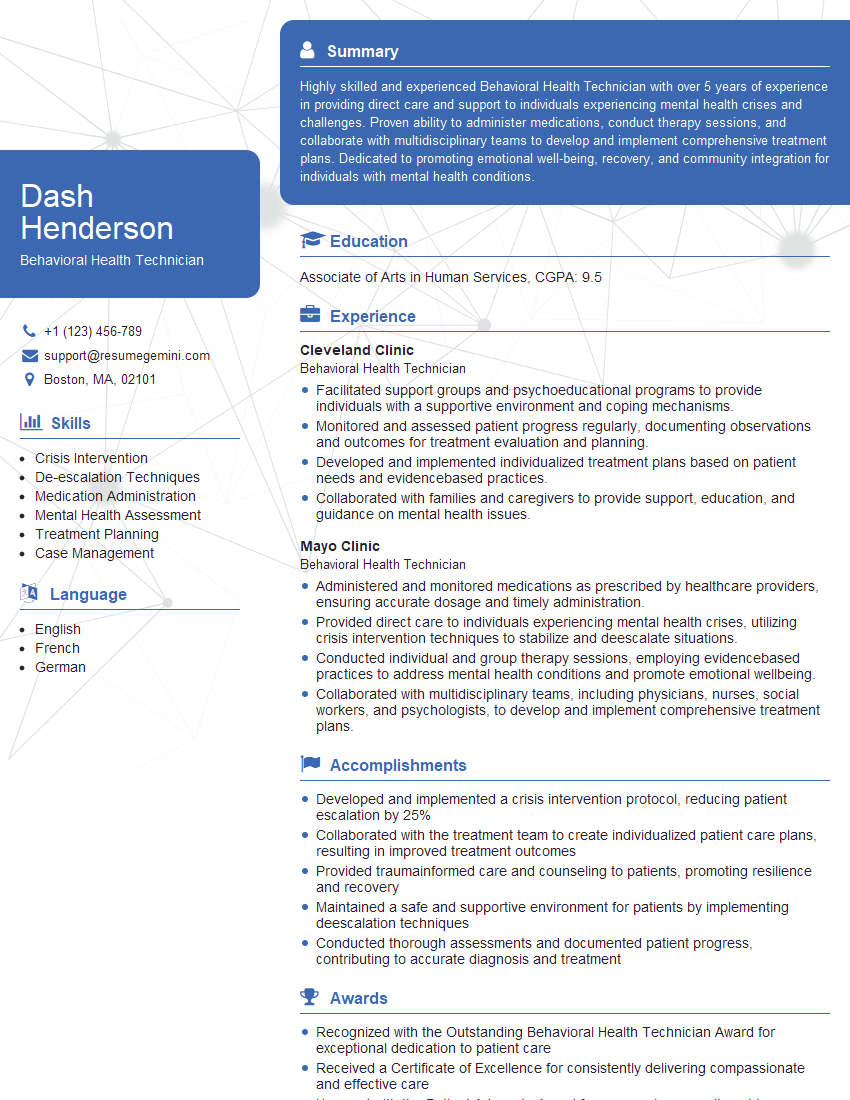
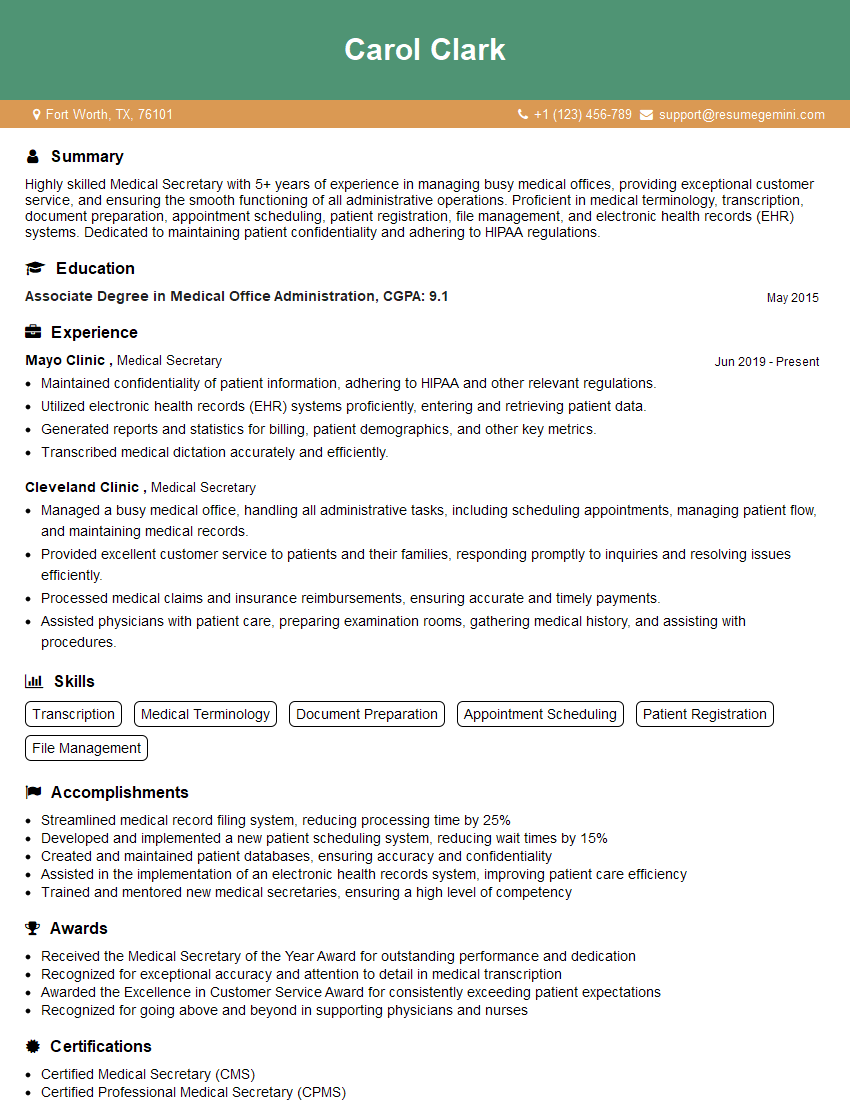
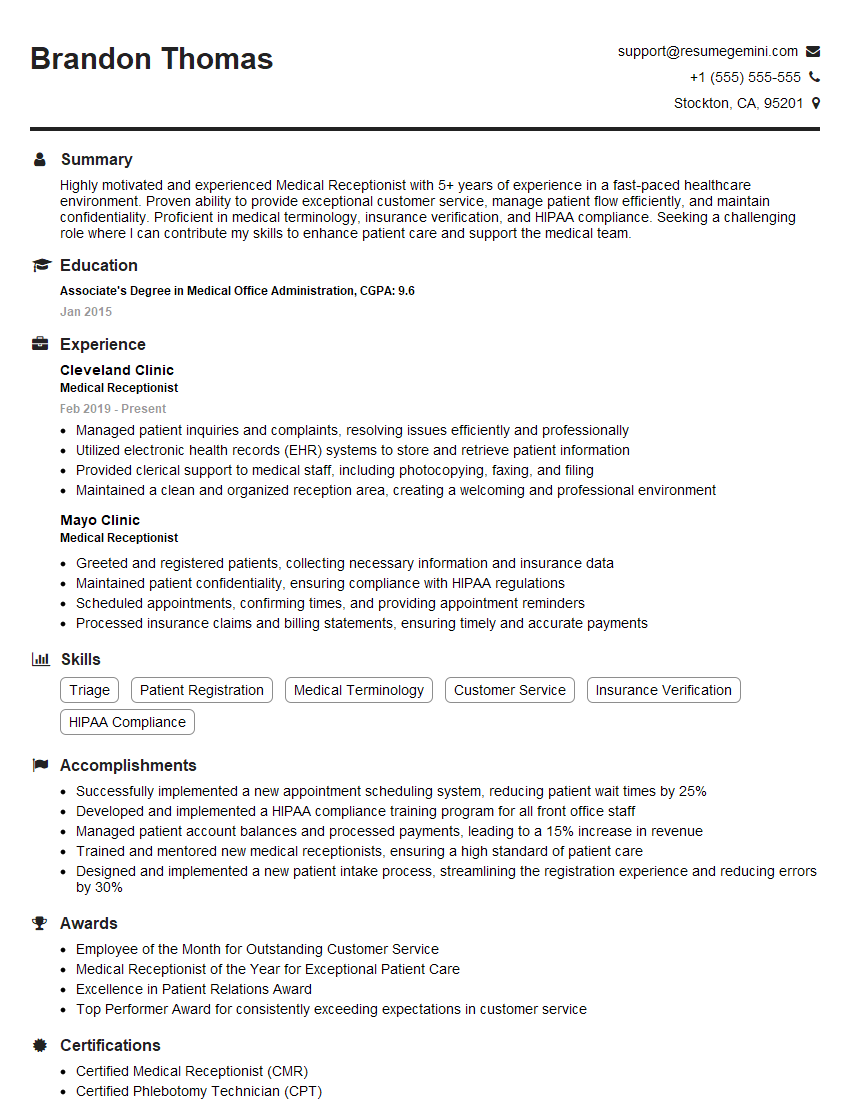
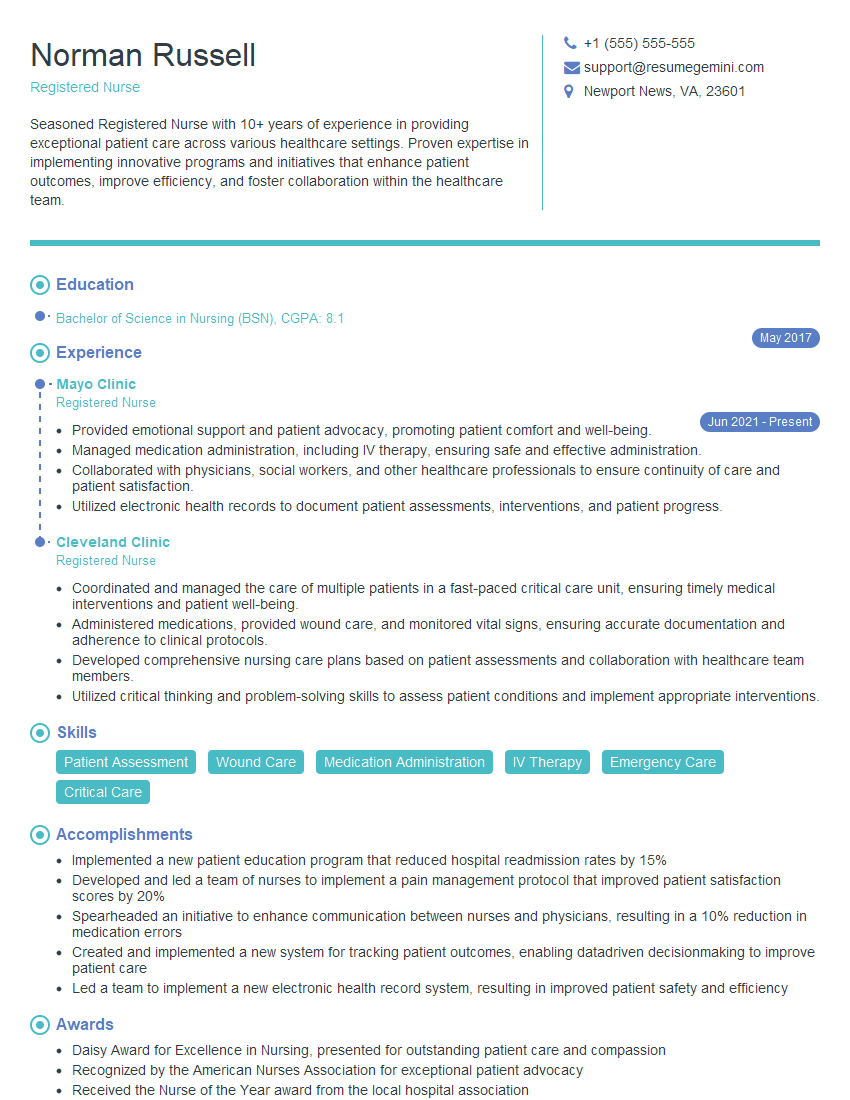
Mastering Patient Interaction and Confidentiality is crucial for career advancement in healthcare. Demonstrating proficiency in these areas showcases your commitment to ethical practice and patient well-being, making you a highly desirable candidate. To significantly boost your job prospects, create an ATS-friendly resume that highlights your relevant skills and experience. ResumeGemini is a trusted resource to help you build a professional and impactful resume. We provide examples of resumes tailored to Patient Interaction and Confidentiality roles to guide you in crafting your own compelling application.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
hello,
Our consultant firm based in the USA and our client are interested in your products.
Could you provide your company brochure and respond from your official email id (if different from the current in use), so i can send you the client’s requirement.
Payment before production.
I await your answer.
Regards,
MrSmith
hello,
Our consultant firm based in the USA and our client are interested in your products.
Could you provide your company brochure and respond from your official email id (if different from the current in use), so i can send you the client’s requirement.
Payment before production.
I await your answer.
Regards,
MrSmith
These apartments are so amazing, posting them online would break the algorithm.
https://bit.ly/Lovely2BedsApartmentHudsonYards
Reach out at [email protected] and let’s get started!
Take a look at this stunning 2-bedroom apartment perfectly situated NYC’s coveted Hudson Yards!
https://bit.ly/Lovely2BedsApartmentHudsonYards
Live Rent Free!
https://bit.ly/LiveRentFREE
Interesting Article, I liked the depth of knowledge you’ve shared.
Helpful, thanks for sharing.
Hi, I represent a social media marketing agency and liked your blog
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?