Every successful interview starts with knowing what to expect. In this blog, we’ll take you through the top Pediatric Urologic Surgery interview questions, breaking them down with expert tips to help you deliver impactful answers. Step into your next interview fully prepared and ready to succeed.
Questions Asked in Pediatric Urologic Surgery Interview
Q 1. Describe your experience with hypospadias repair techniques.
Hypospadias repair is a complex procedure aiming to correct the abnormal opening of the urethra on the underside of the penis. The technique employed depends on several factors including the location of the urethral opening (distal, midshaft, proximal), the presence of chordee (downward curvature of the penis), and the patient’s age and overall health. My approach is individualized and often involves a staged approach, especially in more complex cases.
Distal Hypospadias: For distal hypospadias (opening near the glans), a simple one-stage repair is often sufficient. This typically involves creating a urethral plate from the existing tissue and using it to reconstruct the urethra, thereby creating a more normal urethral opening.
Midshaft and Proximal Hypospadias: These require more extensive procedures, often incorporating techniques like onlay island flaps or free grafts to lengthen the urethra. Chordee correction is frequently necessary, employing techniques such as the MAGPI (Modified Approach to Glansplasty and Plication Incision) or Nesbit procedure. Sometimes, a two-stage approach is utilized to minimize complications and ensure optimal cosmetic and functional outcomes.
Considerations: Careful surgical planning, meticulous tissue handling, and precise surgical technique are crucial to minimize complications such as fistula formation, stricture, and cosmetic deformity. Post-operative care involves careful monitoring for infection, maintaining adequate urinary drainage, and monitoring for complications. Regular follow-up is essential to ensure proper healing and address any issues that might arise.
Q 2. Explain your approach to managing vesicoureteral reflux (VUR) in infants.
Vesicoureteral reflux (VUR) is a condition where urine flows backward from the bladder to the ureters and kidneys. Management in infants depends on the severity of reflux, as determined by voiding cystourethrogram (VCUG).
Low-Grade Reflux (Grades I-II): These are usually managed conservatively with close monitoring through regular urinalysis and ultrasound scans to assess kidney growth and function. Prophylactic antibiotics may be considered in some cases to prevent urinary tract infections (UTIs).
High-Grade Reflux (Grades III-V): These often require more aggressive intervention. Options include prophylactic antibiotics to prevent UTIs and surgical correction, typically via endoscopic injection of a bulking agent (e.g., dextranomer/hyaluronic acid copolymer) to prevent reflux. In select cases, open surgery may be considered.
Important Considerations: Regular monitoring for UTIs is crucial. The goal of management is to prevent kidney damage from recurrent infections. The decision to intervene surgically is individualized, weighing the risks and benefits of surgery against the potential for spontaneous resolution and the risk of long-term kidney damage.
Q 3. What are the different types of bladder exstrophy, and how do you manage each?
Bladder exstrophy is a complex congenital anomaly where the bladder is exposed outside the abdomen. The severity varies, leading to different types:
Classic Bladder Exstrophy: The bladder is completely open and exposed. Management involves a staged surgical approach to close the bladder and reconstruct the abdominal wall. This often begins soon after birth, with further reconstruction later in childhood.
Cloacal Exstrophy: This is a more severe form involving malformations of the bladder, bowel, and genitalia. The management is extremely complex and involves multiple surgical specialties working collaboratively over an extended period.
Epispadias: While not technically a form of exstrophy, it is often associated and involves an abnormal positioning of the urethral opening on the dorsal (upper) surface of the penis. Surgical repair is needed to reposition the urethra.
Management Strategy: Regardless of the specific type, the primary goal is to create a functional urinary tract and reconstruct the abdominal wall. This requires specialized surgical techniques and long-term follow-up to address issues like incontinence and potential kidney damage.
Q 4. How do you diagnose and treat posterior urethral valves?
Posterior urethral valves (PUV) are thin membranes obstructing the urethra, leading to urinary obstruction and bladder distension.
Diagnosis: Diagnosis often begins with prenatal ultrasound, showing bilateral hydronephrosis (swelling of the kidneys). Postnatal confirmation is done via voiding cystourethrogram (VCUG), which visualizes the valves, and further evaluation of kidney function is essential.
Treatment: The mainstay of treatment is percutaneous valve ablation, a minimally invasive procedure performed using a cystoscope to puncture and destroy the valves. In some cases, open surgery might be required. Post-operative monitoring includes regular ultrasound assessments of kidney function, and further interventions might be needed to manage complications like vesicoureteral reflux or bladder dysfunction.
Consequences of untreated PUV: Untreated PUV can cause severe kidney damage and ultimately renal failure. Early diagnosis and treatment are critical to preserving kidney function.
Q 5. Discuss the surgical management of cryptorchidism.
Cryptorchidism, or undescended testicles, requires surgical intervention if the testicles haven’t descended by the age of six months to one year. The goal of surgery (orchiopexy) is to bring the testicle into the scrotum, improving fertility potential and reducing the risk of malignancy.
Surgical Technique: The approach depends on the location of the testicle. Sometimes, simple mobilization and placement are possible. More often, the procedure involves bringing the blood vessels to the appropriate location to allow for testicular viability and fixation in the scrotum.
Laparoscopic Orchiopexy: This minimally invasive approach can be used for intra-abdominal testes and offers advantages like smaller incisions and less post-operative pain.
Importance of Timing: Early intervention is crucial to avoid potential long-term complications like infertility and increased risk of testicular cancer.
Q 6. What is your experience with laparoscopic pediatric urological procedures?
Laparoscopic pediatric urological procedures have become increasingly common in my practice. The benefits include smaller incisions, reduced post-operative pain, shorter hospital stays, and improved cosmesis. I use laparoscopy for several procedures, including pyeloplasty (repair of a narrowed ureter), nephrectomy (kidney removal), and orchiopexy (testicular fixation).
Advantages: Minimally invasive nature reduces trauma, leading to faster recovery. The magnification provided during laparoscopy allows for precise dissection and tissue handling.
Limitations: The learning curve is steeper than for open surgery, requiring specialized training and equipment. Not all procedures are suitable for a laparoscopic approach.
Future Trends: Robotic-assisted laparoscopy is emerging, offering even greater precision and dexterity. I anticipate increasing adoption of these advanced techniques in the future.
Q 7. Explain your approach to the management of primary megaureter.
Primary megaureter is a condition where the ureter is abnormally dilated, often leading to hydronephrosis. The management strategy hinges on determining the cause of the dilatation (obstructive versus non-obstructive).
Diagnosis: This is often diagnosed prenatally via ultrasound. Postnatal evaluation includes VCUG and renal scans to assess kidney function and evaluate for any obstruction.
Non-obstructive Megaureter: In many cases, megaureter is non-obstructive and often resolves spontaneously. Close monitoring of kidney function is essential. Surgical intervention is generally not necessary unless there are signs of deteriorating renal function or recurrent UTIs.
Obstructive Megaureter: If obstruction is present, surgical intervention is often required to restore normal urine flow. This might involve a ureteroplasty (reconstructing the ureter) or occasionally ureteropyelostomy (surgical connection of the ureter to the renal pelvis). The specific technique depends on the cause and location of the obstruction.
Individualized Approach: The approach to primary megaureter is highly individualized, guided by the clinical findings and the severity of renal impairment.
Q 8. How do you counsel parents about the risks and benefits of surgery for their child?
Counseling parents about pediatric surgery requires a delicate balance of providing thorough information and offering compassionate support. I begin by explaining the child’s condition in simple, age-appropriate terms, ensuring the parents understand the diagnosis and its potential impact on their child’s health and development. Then, I clearly outline the proposed surgical procedure, explaining its purpose, the steps involved, and the expected outcomes in a way that’s easily understood.
Crucially, I discuss the potential risks associated with the surgery, including complications such as bleeding, infection, and anesthetic reactions. I present these risks honestly but within the context of their likelihood, emphasizing that serious complications are rare. For instance, when discussing a hypospadias repair (a condition where the urethra opening is not at the tip of the penis), I’ll explain the possibility of infection or a need for revision surgery, while also highlighting the high success rate in achieving a cosmetically pleasing and functionally normal penis. I always make sure to answer any questions the parents may have, no matter how basic or complex. Finally, I discuss the benefits of surgery, focusing on how it can improve the child’s quality of life, reduce symptoms, and prevent long-term health problems. This collaborative approach fosters trust and ensures informed consent.
I often use visual aids like diagrams or videos to illustrate the procedure and its potential benefits, making the information more accessible and less intimidating. I find that allowing ample time for questions and providing written summaries of the discussion help parents feel empowered to make informed decisions.
Q 9. Describe your experience with the management of urinary tract infections (UTIs) in children.
Managing UTIs in children requires a prompt and thorough approach, starting with a detailed history and physical examination. The age of the child is crucial; infants may present with non-specific symptoms like fever, poor feeding, and vomiting, while older children may complain of dysuria (painful urination), frequency, urgency, and abdominal pain.
Laboratory investigations, including urinalysis and urine culture, are essential to confirm the diagnosis and identify the causative organism. Treatment typically involves antibiotics, tailored to the specific bacteria identified. For uncomplicated UTIs, a short course of antibiotics is often sufficient. However, recurrent or complicated UTIs (those associated with abnormalities of the urinary tract) require more extensive evaluation and management. This may involve imaging studies such as renal ultrasound or voiding cystourethrogram (VCUG) to assess for underlying structural abnormalities, such as vesicoureteral reflux (VUR), where urine flows backward from the bladder to the kidneys.
Management of recurrent UTIs can involve long-term antibiotic prophylaxis (preventative antibiotics), regular urine cultures, and, in cases of significant reflux, surgical intervention may be necessary.
A key aspect of managing UTIs in children is educating parents on preventative measures, such as encouraging adequate fluid intake, proper hygiene practices, and prompt treatment of any urinary symptoms.
Q 10. What are the common complications associated with pediatric urological surgery?
Pediatric urological surgery, while generally safe and effective, carries certain potential complications. These can be broadly categorized into early and late complications.
- Early complications (occurring within the first few weeks post-surgery) may include bleeding, infection at the surgical site (wound infection), urinary tract infection (UTI), and anesthetic complications. In minimally invasive surgery, specific complications like port-site bleeding or bowel injury can occur.
- Late complications (developing weeks, months, or even years later) may include strictures (narrowing) of the urethra or ureter, incontinence (inability to control urine), recurrent UTIs, and problems with sexual function. The chance of these complications varies depending on the specific surgery performed.
The risk of these complications is mitigated through meticulous surgical technique, appropriate patient selection, and careful postoperative management. Regular follow-up appointments are essential to monitor for any signs of complications and provide prompt intervention if needed. For example, post-hypospadias repair, careful monitoring for urethral stricture is crucial, with potential for dilation or surgical revision if necessary.
Q 11. How do you manage postoperative pain and complications in pediatric patients?
Postoperative pain management in pediatric patients is crucial for ensuring their comfort, promoting healing, and minimizing the psychological impact of surgery. We utilize a multimodal approach, combining several pain management strategies.
Pharmacological methods include age-appropriate analgesics, such as acetaminophen or ibuprofen, and in some cases, opioids may be necessary for severe pain. However, opioid use in children is minimized due to the potential for side effects. Regional anesthesia techniques, such as caudal or epidural blocks, may be employed to provide effective pain relief for specific procedures.
Non-pharmacological methods play a significant role. These include providing emotional support, distraction techniques (play therapy, entertainment), positioning to maximize comfort, and regular monitoring of vital signs to detect early signs of complications or pain. We involve the family in the pain management plan, educating them on recognizing signs of pain and appropriate methods of comforting their child. The goal is to keep pain manageable, allowing children to recover optimally and participate in age-appropriate activities as soon as possible.
Q 12. Discuss your understanding of the latest advancements in pediatric urology.
Pediatric urology has seen remarkable advancements in recent years. Minimally invasive techniques, such as laparoscopy and robotic surgery, are becoming increasingly prevalent, offering significant advantages like smaller incisions, reduced pain, shorter hospital stays, and faster recovery times.
Advancements in imaging technology, particularly in ultrasound, MRI, and CT scans, have greatly improved our ability to diagnose and manage complex urological conditions. Functional imaging techniques provide valuable insights into the dynamics of the urinary system. The development of novel surgical techniques, such as less invasive approaches to hypospadias repair and newer materials for reconstructive procedures, continues to improve surgical outcomes.
Furthermore, significant strides have been made in the understanding of genetic and epigenetic factors contributing to congenital urological anomalies. This has potential implications for future diagnostic and therapeutic strategies, including gene therapy. The field is constantly evolving and I stay updated through continuous medical education, participation in professional conferences and research activities.
Q 13. How do you utilize imaging modalities (ultrasound, CT, MRI) in pediatric urological cases?
Imaging modalities are invaluable in pediatric urology. Ultrasound is often the first-line imaging technique, particularly in evaluating the kidneys and bladder. Its non-invasive nature and lack of ionizing radiation make it ideal for children. Renal ultrasounds assess kidney size, shape, and function, while bladder ultrasounds can detect bladder distention or masses. Voiding cystourethrography (VCUG), a type of fluoroscopic study, is used to assess for vesicoureteral reflux.
CT scans and MRIs are used selectively in more complex cases where detailed anatomical information is required. CT is useful for visualizing bony structures and complex abnormalities, whereas MRI provides superior soft-tissue detail. These techniques, however, involve ionizing radiation (CT) or strong magnetic fields (MRI), and their use is carefully considered, balancing the benefit of obtaining detailed images against the potential risks, especially in younger children. We always choose the safest and most appropriate imaging modality based on the child’s age and clinical circumstances.
Q 14. What is your experience with the use of minimally invasive surgical techniques in pediatric urology?
Minimally invasive surgical techniques have revolutionized pediatric urology. I have extensive experience using laparoscopy and robotic surgery for a range of procedures, including pyeloplasty (repair of a narrowed ureter), nephrectomy (kidney removal), and adrenalectomy (adrenal gland removal).
Compared to open surgery, minimally invasive approaches offer several key advantages. Patients experience less pain, have smaller incisions, resulting in improved cosmesis, shorter hospital stays, and quicker recovery times. These benefits are particularly significant for children, minimizing their physical and psychological trauma. The use of advanced visualization techniques, such as high-definition cameras and robotic manipulators, allows for enhanced precision and dexterity during the procedure. While minimally invasive surgery isn’t always suitable for every pediatric urological condition, its utilization is continuously expanding and significantly contributing to improved patient outcomes.
Q 15. Describe your experience with the management of neurogenic bladder.
Neurogenic bladder refers to bladder dysfunction caused by a neurological condition affecting the nerves controlling bladder function. Management is highly individualized and depends on the underlying neurological condition, the child’s age, and the severity of the bladder dysfunction. My approach involves a multidisciplinary team including urologists, neurologists, physical therapists, and often, nurses specialized in continence care.
Initial assessment includes a thorough history and physical exam, focusing on the neurological condition, voiding symptoms (frequency, urgency, incontinence, hesitancy), and potential complications like urinary tract infections (UTIs). Urodynamic studies, including cystometry and pressure-flow studies, are crucial to objectively assess bladder function and identify the specific type of neurogenic bladder (e.g., spastic, flaccid).
Management strategies range from conservative measures to surgical intervention. Conservative approaches include bladder training, intermittent catheterization (clean intermittent self-catheterization, or CISC, is taught as soon as appropriate), and medications to manage bladder spasms or improve bladder emptying. For example, a child with a spastic neurogenic bladder might benefit from anticholinergics to relax the bladder. In cases of recurrent UTIs or significant bladder dysfunction unresponsive to conservative measures, surgical options may be considered, such as augmentation cystoplasty (increasing bladder capacity) or urinary diversion (creating an alternative pathway for urine).
A key element is educating the family about the child’s condition, the management plan, and the importance of consistent adherence to the treatment regimen. Regular follow-up visits are crucial to monitor bladder function, prevent complications, and adjust the management plan as needed.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Explain your approach to the management of obstructive uropathy.
Obstructive uropathy refers to the blockage of urine flow from the kidneys to the bladder. Early detection and prompt management are critical to prevent irreversible kidney damage. My approach emphasizes a systematic investigation to identify the cause and location of the obstruction, followed by appropriate intervention.
The initial assessment includes a thorough history (including prenatal history and symptoms like abdominal pain, vomiting, or recurrent UTIs) and physical examination, along with imaging studies such as ultrasound, voiding cystourethrogram (VCUG), and potentially, renal scans (e.g., DMSA or MAG3) to assess renal function and the location and severity of the obstruction. Sometimes, a CT scan with contrast is needed for better visualization. The specific cause, for instance posterior urethral valves or ureteropelvic junction obstruction, will guide the management.
Management depends on the cause and severity of the obstruction. In some cases, minimally invasive procedures like endoscopic incision or stenting may suffice to relieve the obstruction. More complex obstructions might require open surgery. For example, a child with posterior urethral valves might need a valve ablation procedure. Post-operative management includes close monitoring of renal function and hydration to ensure proper urine flow.
Regular follow-up is essential to monitor renal function and ensure the effectiveness of the intervention. Long-term management may include prophylactic antibiotics to prevent UTIs or ongoing monitoring for residual renal impairment.
Q 17. How do you assess renal function in pediatric patients?
Assessing renal function in pediatric patients involves a multi-faceted approach, combining clinical evaluation with laboratory tests and imaging. It’s crucial to tailor the assessment to the child’s age and the clinical suspicion.
Clinically, we look for signs of renal impairment such as poor growth, hypertension, edema, or anemia. Laboratory tests play a significant role. Serum creatinine and blood urea nitrogen (BUN) are commonly used markers, but their interpretation needs to be age-adjusted because creatinine production varies with age and muscle mass. A better indicator in children is the estimated glomerular filtration rate (eGFR), calculated using equations that incorporate age, sex, and serum creatinine. Urine analysis is also crucial, checking for proteinuria, hematuria, or other abnormalities that might indicate renal disease.
Renal imaging is often necessary to visualize the kidneys and assess their size, structure, and function. Ultrasound is usually the initial imaging modality; it’s non-invasive and provides a good assessment of kidney size and morphology. More sophisticated imaging techniques like DMSA (dimercaptosuccinic acid) scans and MAG3 (mercaptoacetyltriglycine) scans provide functional information about each kidney, demonstrating their individual contribution to overall renal function.
It’s important to consider that different tests have limitations. For instance, serum creatinine may not reflect a decline in renal function until significant damage has already occurred. Therefore, a comprehensive assessment incorporating clinical findings, laboratory data, and imaging studies is essential for accurate evaluation of renal function in children.
Q 18. What are the different types of kidney stones in children, and how do you manage them?
Kidney stones in children, while less common than in adults, can cause significant pain and complications. The most common types are calcium oxalate stones, followed by uric acid stones and struvite stones. Calcium oxalate stones are frequently idiopathic but can be associated with dehydration or certain metabolic disorders. Uric acid stones are seen in children with gout or other metabolic disorders, while struvite stones are usually associated with chronic UTIs caused by urease-producing bacteria.
Diagnosis typically begins with a detailed history and physical examination, focusing on symptoms such as flank pain, hematuria, and changes in urinary habits. Imaging studies such as ultrasound and non-contrast CT scans are invaluable for detecting stones and assessing their size and location. Additional tests might include urinalysis to identify stone composition and metabolic workup to investigate underlying causes.
Management depends on the stone size, location, and symptoms. Small stones (less than 5 mm) often pass spontaneously with increased fluid intake and pain management. Larger stones or those causing obstruction might require intervention. Options include extracorporeal shock wave lithotripsy (ESWL), which uses shock waves to break up the stones, or ureteroscopy, a minimally invasive procedure that allows for direct visualization and removal of the stones. In some cases, open surgery might be necessary. Post-treatment, we focus on preventing recurrence through dietary modifications, increased fluid intake, and addressing any underlying metabolic disorders.
Q 19. Discuss the management of enuresis.
Enuresis, or bedwetting, is a common problem in children. The management approach is tailored to the child’s age, developmental stage, and the presence of any underlying medical or psychological issues. It’s crucial to distinguish between primary enuresis (never achieved nighttime bladder control) and secondary enuresis (bedwetting after a period of dryness).
A detailed history is essential, including a review of the child’s fluid intake, toilet habits, and sleep patterns. A physical exam is conducted to rule out any underlying medical conditions, such as UTIs or diabetes. In some cases, further investigations may include urinalysis and urodynamic studies. Psychological factors are also considered.
Management starts with education and reassurance, emphasizing that it’s a common problem and that treatment is effective. Behavioral therapies, such as bladder training, nighttime fluid restriction, and positive reinforcement, are often the first line of treatment. In some children, alarms that wake them up at the onset of urination are helpful. Pharmacological interventions, such as desmopressin (a medication that reduces urine production), might be considered if behavioral therapies are insufficient. Success rates often improve with a combination of approaches tailored to the individual child.
Regular follow-up is vital to monitor progress and adjust the treatment as needed. It’s important to involve the child and family in the management plan, creating a supportive and collaborative environment.
Q 20. How do you approach the diagnosis and treatment of ambiguous genitalia?
Ambiguous genitalia refers to a situation where the external sex organs are not clearly male or female at birth. This necessitates a careful and coordinated multidisciplinary approach involving pediatric urologists, endocrinologists, geneticists, and psychologists. The management aims to determine the child’s chromosomal sex, gonadal sex, and the potential for future fertility.
The diagnostic process begins with a thorough physical examination to assess the external genitalia and evaluate the internal anatomy using imaging techniques such as ultrasound and MRI. Chromosomal analysis (karyotyping) and hormonal studies are crucial for determining the genetic sex and hormonal profile. Genetic testing might be needed to identify specific genetic conditions underlying the ambiguity.
Treatment decisions are made based on the diagnosis and the potential for future fertility. Surgery may be indicated to correct the external genitalia, but the timing of surgery is often debated. Many experts advocate for delaying surgery until the child is old enough to participate in the decision-making process. Hormone replacement therapy might be necessary in some cases to promote appropriate sexual development. Long-term follow-up is essential to monitor growth, development, and psychological well-being.
This process is emotionally challenging for families. Providing sensitive counseling and support is paramount throughout the diagnostic and treatment process, fostering open communication and collaboration between the medical team and the family. The focus is on creating a plan that respects the child’s future autonomy.
Q 21. Describe your understanding of the psychological impact of urological conditions on children and their families.
Urological conditions in children can significantly impact their psychological well-being and that of their families. The nature and severity of the impact vary depending on the specific condition, its treatment, and the child’s age and personality. Conditions like enuresis, for instance, can lead to feelings of shame, embarrassment, and low self-esteem. Children with ambiguous genitalia or other conditions requiring surgery may face body image issues and anxiety about their appearance.
The psychological impact extends to the families as well. Parents may experience guilt, anxiety, and stress related to their child’s condition and the challenges of managing it. Siblings may also be affected, feeling neglected or worried about their brother or sister. The financial burden of treatment can add to the family’s stress.
To mitigate the psychological impact, it’s crucial to provide comprehensive psychosocial support. This includes open communication between the medical team and the family, allowing for honest discussions about the child’s condition, treatment options, and prognosis. Referral to psychologists or social workers may be beneficial for both the child and the family, providing coping strategies, emotional support, and guidance through the challenges. Support groups can also provide a valuable sense of community and shared experience.
The goal is to create a supportive and understanding environment where the child and family feel empowered to cope with the challenges of the condition and lead fulfilling lives.
Q 22. What is your experience with the long-term follow-up of pediatric urological patients?
Long-term follow-up in pediatric urology is crucial because children’s anatomy and physiology change significantly as they grow. It’s not just about addressing the immediate surgical outcome; we need to monitor for potential complications, recurrence, or delayed effects that might only become apparent years later.
My approach involves a structured schedule of follow-up visits tailored to the specific condition and surgical intervention. For example, children post-hypospadias repair might require regular assessments of urethral caliber and cosmetic appearance for several years. Those with vesicoureteral reflux (VUR) need regular ultrasound scans and urinalysis to monitor for infection and kidney damage. We also carefully track growth parameters, particularly in cases involving renal surgeries.
Furthermore, we actively engage the families in the long-term care plan, educating them about potential issues and empowering them to report any concerns promptly. This collaborative approach is essential for early detection and management of any potential problems. Regular communication, including email and phone access, facilitates this process. We also employ electronic health records to track all clinical data effectively for seamless transition of care as the patient ages.
Q 23. Explain your approach to managing a surgical emergency in pediatric urology.
Managing a surgical emergency in pediatric urology requires immediate action, prioritizing the child’s well-being and stability. Our initial steps focus on stabilizing the patient’s vital signs—ABCs (Airway, Breathing, Circulation)—before moving on to a detailed urologic assessment.
The emergency could range from a traumatic injury like bladder rupture to severe complications from a previously treated condition such as a urinary stone causing complete obstruction. Our approach involves:
- Rapid assessment: Identifying the severity of the condition, using imaging (ultrasound, CT scan) if needed.
- Stabilization: Addressing any immediate threats to life or limb.
- Surgical intervention: If necessary, this might include procedures like percutaneous nephrostomy for relief of an obstructed kidney or immediate repair of a urethral trauma.
- Post-operative care: Intensive care, pain management, and close monitoring of vital signs and organ function.
Effective communication with the family is essential throughout the process, offering support and providing regular updates on the child’s condition. We adhere strictly to established pediatric emergency protocols and ensure close collaboration with other specialists like trauma surgeons or anesthesiologists, as needed. For instance, managing a severe penile fracture requires immediate reduction and fixation, followed by meticulous post-operative care to prevent complications like chordee or erectile dysfunction.
Q 24. What is your experience with robotic-assisted surgery in pediatric urology?
Robotic-assisted surgery has revolutionized many aspects of pediatric urology. The benefits include enhanced precision, minimized invasiveness, reduced blood loss, shorter hospital stays, and improved cosmetic outcomes. My experience with robotic surgery in pediatric urology is extensive, covering a wide range of procedures.
We utilize robotic-assisted techniques for complex reconstructive surgeries such as pyeloplasty (repair of a narrowed ureter), ureteral reimplantation (correcting vesicoureteral reflux), and complex hypospadias repair. The magnified three-dimensional visualization and enhanced dexterity offered by the robotic system allow for intricate surgical maneuvers that are often difficult to achieve with conventional laparoscopy or open surgery. This translates to better anatomical restoration and reduced risk of complications.
However, it’s essential to remember that robotic surgery is not a replacement for open surgery in all cases. Careful patient selection is crucial. We need to consider the child’s age, anatomy, and the specific nature of the pathology. We prioritize the safety and well-being of the child, and open surgery remains our preferred technique in certain scenarios, where the complexity warrants it.
Q 25. How do you incorporate evidence-based practices into your clinical decision-making?
Evidence-based practice is the cornerstone of my clinical decision-making. It involves integrating the best available research evidence with clinical expertise and patient values to deliver optimal care. I stay updated on the latest research through various means:
- Regular review of peer-reviewed journals: Publications like the Journal of Urology, Journal of Pediatric Urology, and others provide current information on surgical techniques, diagnostic approaches, and treatment outcomes.
- Attendance at national and international conferences: These events provide opportunities to learn from leading experts and network with colleagues.
- Membership in professional organizations: Participation in organizations like the American Urological Association (AUA) provides access to guidelines, educational resources, and networking opportunities.
- Critical appraisal of research findings: I carefully evaluate the quality, validity, and applicability of research studies before incorporating them into my practice.
For example, when deciding on the optimal surgical approach for a specific case of VUR, I would consult the latest AUA guidelines, review the relevant literature on different surgical techniques, and consider the child’s individual circumstances before making a personalized recommendation. The ultimate goal is to provide the most effective and safest treatment tailored to each patient.
Q 26. How do you manage the ethical dilemmas encountered in pediatric urology?
Ethical dilemmas in pediatric urology are complex and often arise from the unique vulnerabilities of children. These could involve decisions about aggressive versus conservative management, balancing the risks and benefits of surgery, respecting parental autonomy while prioritizing the child’s best interests, and navigating issues of informed consent.
My approach involves a multidisciplinary approach. We involve ethicists, social workers, and psychologists when navigating difficult cases. We prioritize open communication with families, ensuring they understand the various treatment options, potential risks and benefits, and the long-term implications of each decision. Transparency and shared decision-making are paramount. We ensure the child’s voice is heard to the extent their developmental stage allows.
For instance, managing a child with ambiguous genitalia requires careful consideration of the child’s and family’s values and beliefs alongside best medical practice. We strive to create a supportive environment that empowers the family to make informed decisions in the child’s best interest, while considering their cultural and religious background. This might involve referring the family to specialized support groups or genetic counselors for further guidance.
Q 27. Describe a challenging case in pediatric urology and how you successfully managed it.
One challenging case involved a 6-month-old infant presenting with bilateral massive hydronephrosis (swelling of the kidneys due to urine blockage) secondary to posterior urethral valves (PUVs). PUVs are a congenital condition that obstructs urine outflow from the bladder. The infant was critically ill, showing signs of renal failure.
The initial challenge was the severity of the condition; immediate intervention was necessary to prevent irreversible renal damage. We performed a vesicostomy (creating a temporary opening in the bladder) to divert urine flow, relieving the pressure on the kidneys. This stabilized the infant’s condition. Following stabilization, we performed an endoscopic resection of the PUVs using a specialized pediatric endoscope to minimize trauma.
Post-operatively, close monitoring of renal function was crucial. We employed regular ultrasound scans and blood tests to track the kidneys’ recovery. The infant responded well to treatment and gradually showed improvement in renal function. After several months, the vesicostomy was closed successfully. Long-term follow-up confirmed the child’s continued normal kidney function and healthy growth, showcasing the importance of a timely and effective multi-pronged approach in such critical cases.
Key Topics to Learn for Pediatric Urologic Surgery Interview
- Embryology and Congenital Anomalies: Understanding the developmental processes and common congenital anomalies of the urinary tract in children (e.g., hypospadias, vesicoureteral reflux, posterior urethral valves). Consider the spectrum of severity and associated conditions.
- Diagnosis and Imaging: Mastering the interpretation of various imaging modalities (ultrasound, voiding cystourethrogram, renal scan) and their role in diagnosing pediatric urologic conditions. Practice correlating imaging findings with clinical presentations.
- Surgical Techniques: Familiarity with common surgical procedures used in pediatric urology, including those for hypospadias repair, ureteral reimplantation, and pyeloplasty. Focus on indications, contraindications, and potential complications.
- Minimally Invasive Surgery: Understanding the principles and applications of laparoscopy and robotic surgery in pediatric urology. Discuss advantages and limitations compared to open surgery.
- Urinary Tract Infections (UTIs): Know the epidemiology, diagnosis, management, and potential long-term consequences of UTIs in children. Be prepared to discuss recurrent UTIs and vesicoureteral reflux.
- Neurogenic Bladder: Understanding the pathophysiology, diagnosis, and management of neurogenic bladder dysfunction in children with spinal cord injuries or other neurological conditions. Be familiar with various treatment options.
- Enuresis and Voiding Dysfunction: Familiarize yourself with the evaluation and management of enuresis and other voiding dysfunctions in children, including behavioral therapy and medication options.
- Bladder Exstrophy: Understand the complex multidisciplinary management approach for this significant congenital anomaly.
- Oncological Aspects: Basic understanding of pediatric urological cancers (Wilms tumor, rhabdomyosarcoma) including staging, treatment modalities and long-term follow-up.
- Ethical Considerations: Be prepared to discuss ethical dilemmas that may arise in pediatric urology, such as parental consent and decision-making for complex cases.
Next Steps
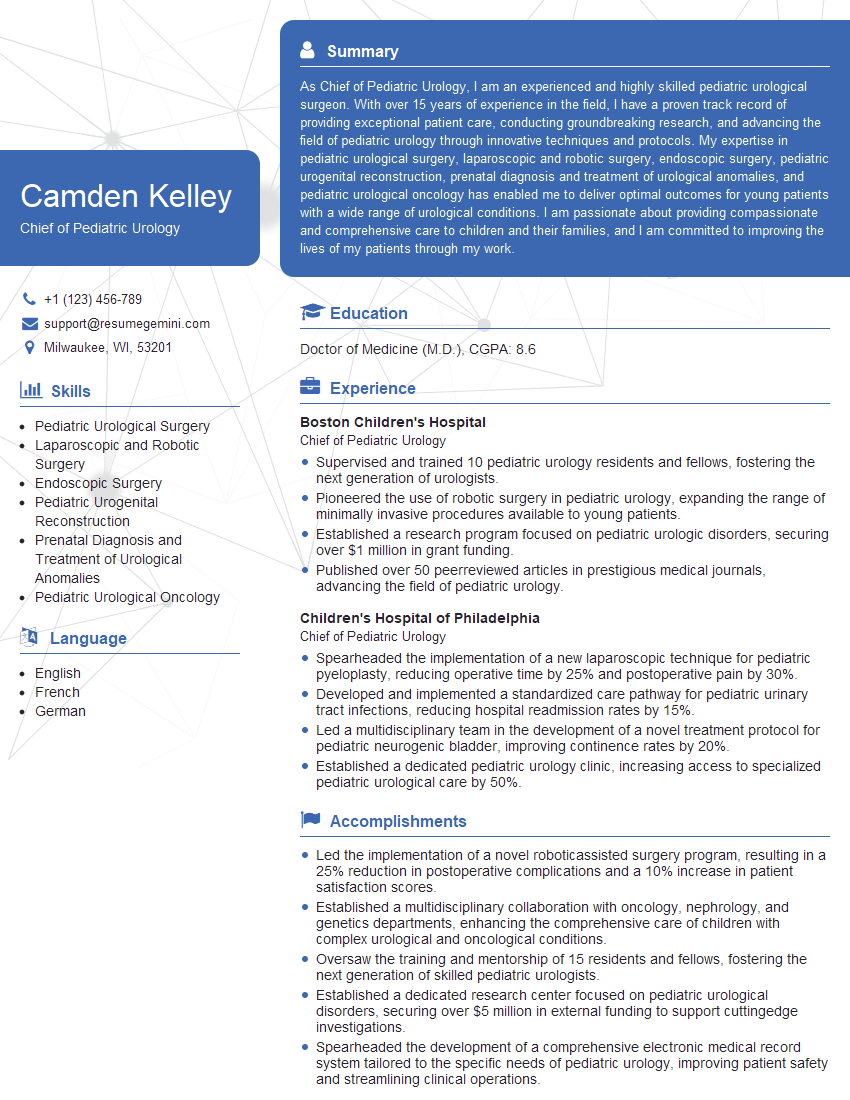
Mastering Pediatric Urologic Surgery opens doors to a rewarding career with significant impact on young patients’ lives. This specialization demands a deep understanding of both surgical techniques and the unique developmental considerations of children. To stand out to potential employers, crafting a compelling and ATS-friendly resume is crucial. ResumeGemini is a trusted resource that can help you build a professional resume tailored to highlight your skills and experience in this competitive field. Examples of resumes specifically tailored to Pediatric Urologic Surgery are available to further enhance your application materials.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Live Rent Free!
https://bit.ly/LiveRentFREE
Interesting Article, I liked the depth of knowledge you’ve shared.
Helpful, thanks for sharing.
Hi, I represent a social media marketing agency and liked your blog
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?