Interviews are opportunities to demonstrate your expertise, and this guide is here to help you shine. Explore the essential Pre-Operative and Post-Operative Care interview questions that employers frequently ask, paired with strategies for crafting responses that set you apart from the competition.
Questions Asked in Pre-Operative and Post-Operative Care Interview
Q 1. Describe the pre-operative assessment process for a patient undergoing a major abdominal surgery.
The pre-operative assessment for a major abdominal surgery is crucial for ensuring patient safety and optimizing surgical outcomes. It’s a comprehensive process involving a detailed history, physical examination, and various investigations. We begin by gathering a thorough medical history, focusing on previous surgeries, allergies, medications (including over-the-counter drugs and herbal remedies), and any existing medical conditions like heart disease, diabetes, or respiratory problems. This helps us identify potential risks and tailor the anesthetic plan accordingly.
Next, a comprehensive physical examination is performed, paying particular attention to the cardiovascular and respiratory systems. We assess vital signs, listen to heart and lung sounds, and check for any signs of infection. For abdominal surgery, a detailed abdominal examination is essential, noting any masses, tenderness, or distension. Laboratory investigations are crucial and usually include a complete blood count (CBC) to assess hemoglobin levels and the risk of bleeding, coagulation studies to evaluate clotting function, electrolyte levels, liver and kidney function tests, and a urinalysis. Imaging studies like chest X-rays, ECGs, and sometimes CT scans may be needed to further assess organ function and identify any abnormalities. Finally, a detailed discussion with the patient and their family about the procedure, risks, benefits, and alternatives is paramount. This ensures informed consent and reduces anxiety.
- Example: A patient with a history of poorly controlled hypertension might require additional cardiovascular monitoring during and after surgery.
- Example: A patient with a history of deep vein thrombosis (DVT) might need prophylactic anticoagulation before surgery.
Q 2. Explain the importance of patient education in pre-operative care.
Patient education is absolutely vital in pre-operative care because it empowers patients, fosters collaboration, and improves outcomes. When patients understand the procedure, potential risks, recovery process, and their role in their care, they’re better prepared for the experience and more likely to adhere to post-operative instructions. This leads to reduced complications and faster recovery times.
We aim to provide clear, concise information, using simple language and avoiding medical jargon whenever possible. We address their concerns and anxieties honestly, providing realistic expectations. We explain the pre-operative preparation, including fasting guidelines, bowel preparation (if necessary), and skin preparation. We also cover post-operative pain management strategies, mobility expectations, and dietary restrictions. The use of visual aids, brochures, and videos can significantly improve patient understanding and retention.
Example: Clearly explaining the need for deep breathing exercises post-operatively can help prevent post-operative pneumonia. Providing detailed information on pain management options can alleviate patient anxiety and improve their experience.
Q 3. What are the common complications associated with general anesthesia?
General anesthesia, while generally safe, carries potential complications. These can range from minor to life-threatening. Common complications include nausea and vomiting (PONV), which is quite prevalent. Other common complications include:
- Hypotension: A drop in blood pressure that can lead to inadequate organ perfusion.
- Tachycardia/Bradycardia: Abnormal heart rate, either too fast or too slow.
- Respiratory depression: Slowed or inadequate breathing requiring ventilatory support.
- Malignant hyperthermia: A rare but potentially fatal condition characterized by rapid rise in body temperature, muscle rigidity, and acidosis. This is often triggered by certain anesthetic agents.
- Postoperative cognitive dysfunction (POCD): Temporary or sometimes persistent cognitive impairment after surgery.
- Allergic reactions: Though rare, allergic reactions to anesthetic drugs can occur.
Mitigation Strategies: Careful pre-operative assessment, appropriate anesthetic selection tailored to the patient’s condition, careful monitoring during surgery, and prompt intervention in case of complications are crucial in minimizing these risks.
Q 4. How do you manage a patient experiencing post-operative nausea and vomiting?
Post-operative nausea and vomiting (PONV) is a common and distressing complication. Management focuses on preventing it whenever possible and treating it effectively if it occurs. Prophylactic antiemetic medication is often given before, during, and after surgery. This might include 5-HT3 receptor antagonists (like ondansetron), antihistamines, or neurokinin-1 receptor antagonists. If PONV occurs despite prophylaxis, we initiate treatment with antiemetic medications as needed. We may adjust the route of administration, depending on the patient’s ability to tolerate oral medications. Intravenous antiemetics are used if the patient is unable to take oral medications.
In addition to medication, supportive measures are vital. These might include clear liquid diet and avoiding strong odours. In severe cases, intravenous fluids might be required to prevent dehydration. We closely monitor the patient’s fluid balance, electrolyte levels, and vital signs. Pain control is also important as pain can exacerbate nausea and vomiting.
Q 5. Describe your experience with pain management in post-operative patients.
Pain management in post-operative patients is a crucial aspect of care that significantly impacts their recovery and overall well-being. We employ a multimodal approach, combining different methods to achieve optimal pain control while minimizing side effects. This might include:
- Analgesics: Opioids, NSAIDs, and acetaminophen are used, tailoring the choice and dosage to the patient’s specific needs and pain level. We always consider the potential risks and side effects of each medication.
- Regional anesthesia techniques: Epidural or nerve blocks can provide excellent pain relief with fewer systemic side effects than systemic opioids. These methods are especially beneficial for patients undergoing major abdominal or orthopedic surgery.
- Non-pharmacological approaches: These might include heat/cold therapy, relaxation techniques, patient education on pain management strategies, and physical therapy to improve mobility and reduce pain.
Example: A patient with severe post-operative pain might initially require intravenous opioids, gradually transitioning to oral analgesics as the pain subsides. Regular assessment of the patient’s pain level using validated pain scales (like the numerical rating scale or visual analog scale) is crucial for guiding our pain management strategy.
Q 6. What are the signs and symptoms of post-operative hypovolemic shock?
Post-operative hypovolemic shock is a life-threatening condition caused by significant blood or fluid loss. It occurs when the circulatory system doesn’t have enough fluid volume to deliver adequate oxygen and nutrients to the tissues. The signs and symptoms can vary depending on the severity of the fluid loss. However, common indicators include:
- Hypotension: Low blood pressure is a hallmark sign.
- Tachycardia: Rapid heart rate as the heart tries to compensate for the decreased blood volume.
- Tachypnea: Increased respiratory rate as the body attempts to increase oxygen intake.
- Cool, clammy skin: Peripheral vasoconstriction leads to reduced blood flow to the extremities, resulting in pale and cool skin.
- Decreased urine output: The kidneys respond to hypovolemia by reducing urine production.
- Altered mental status: Confusion, lethargy, or even unconsciousness can occur due to reduced cerebral blood flow.
- Weakness and fatigue: Muscle weakness and generalized fatigue are common.
Immediate Action: This is a medical emergency requiring immediate intervention. It involves fluid resuscitation with intravenous fluids, blood transfusions (if indicated), and treatment of the underlying cause of blood/fluid loss. Monitoring vital signs, fluid balance, and urine output are crucial.
Q 7. How do you assess a patient’s respiratory status post-operatively?
Post-operative respiratory assessment is critical as respiratory complications are among the most common problems after surgery. The assessment includes:
- Respiratory rate and rhythm: Observing the rate, depth, and regularity of breathing. Tachypnea (rapid breathing) or bradypnea (slow breathing) might indicate underlying problems.
- Breath sounds: Auscultating the lungs to identify any abnormal sounds such as crackles, wheezes, or diminished breath sounds. These can be indicative of atelectasis (lung collapse), pneumonia, or other respiratory complications.
- Oxygen saturation: Measuring SpO2 using pulse oximetry to assess the oxygenation level in the blood. Hypoxemia (low blood oxygen) needs prompt attention.
- Work of breathing: Assessing the effort required for breathing, noting any use of accessory muscles, retractions, or nasal flaring. Increased work of breathing suggests respiratory distress.
- Arterial blood gas (ABG) analysis: In certain cases, ABG analysis is used to precisely measure the blood’s oxygen and carbon dioxide levels and acid-base balance. This provides valuable information for guiding respiratory support.
Interventions: Based on the assessment findings, interventions might include supplemental oxygen, incentive spirometry to prevent atelectasis, coughing and deep breathing exercises, airway suctioning, and in severe cases, mechanical ventilation.
Q 8. What are the key components of a post-operative care plan?
A comprehensive post-operative care plan focuses on a smooth transition from the operating room to recovery and eventual discharge. It’s a dynamic document, adjusted based on the patient’s specific needs and response to treatment. Key components include:
- Pain Management: This is paramount. We assess pain levels regularly using validated scales (like the Numeric Rating Scale or the Faces Pain Scale) and tailor analgesia – including medication, nerve blocks, or other modalities – to individual patient requirements. For example, a patient recovering from abdominal surgery might require a multimodal approach involving opioids, NSAIDs, and regional anesthesia.
- Wound Care: Careful assessment and management of the surgical site are crucial to prevent infection. This involves regular inspection for signs of infection (redness, swelling, drainage, warmth), appropriate dressing changes, and sometimes the use of negative pressure wound therapy.
- Fluid and Electrolyte Balance: Surgery can disrupt fluid balance. We monitor intake and output, electrolyte levels (sodium, potassium, etc.), and adjust intravenous fluids as necessary to prevent dehydration or electrolyte imbalances.
- Respiratory Care: Patients are encouraged to deep breathe and cough regularly to prevent atelectasis (lung collapse) and pneumonia. Incentive spirometry and early ambulation are also important components.
- Gastrointestinal Function: We monitor bowel sounds, assess for nausea and vomiting, and encourage early mobilization and oral intake as tolerated. Management of post-operative ileus (discussed in a later question) is a key part of this.
- Mobility and Physical Therapy: Early mobilization is vital to prevent complications such as DVT (deep vein thrombosis), pneumonia, and muscle atrophy. Physical therapists play a crucial role in guiding patients through exercises and assisting with ambulation.
- Medication Reconciliation: A thorough review of all medications the patient is taking, including those started post-operatively, is necessary to prevent drug interactions and adverse effects.
- Discharge Planning: This process begins early in the post-operative period and includes arranging for home care, follow-up appointments, and providing clear instructions to the patient and caregivers.
Q 9. Explain the role of deep vein thrombosis (DVT) prophylaxis in post-operative care.
Deep vein thrombosis (DVT) prophylaxis is crucial in post-operative care because surgery increases the risk of blood clot formation in the deep veins of the legs. These clots can travel to the lungs, causing a life-threatening pulmonary embolism (PE). Prophylaxis aims to prevent these devastating complications.
Strategies for DVT prophylaxis include:
- Mechanical methods: Graduated compression stockings (GCSS) improve venous return, reducing blood stasis. Intermittent pneumatic compression (IPC) devices provide rhythmic compression to the legs, further promoting venous return.
- Pharmacological methods: Low molecular weight heparin (LMWH) like enoxaparin or fondaparinux are commonly used. These medications prevent clot formation without significant bleeding risk in most patients. The choice of prophylaxis depends on the patient’s risk factors, type of surgery, and other medical conditions.
For example, a patient undergoing major orthopedic surgery would likely receive both GCSS and LMWH prophylaxis. The timing and duration of prophylaxis are tailored to the individual patient’s risk profile.
Q 10. How do you identify and manage a post-operative wound infection?
Post-operative wound infection is a serious complication that needs prompt identification and management. Early detection is key.
Identification: We assess the surgical site regularly for signs of infection, including:
- Increased pain: More than would be expected for normal post-operative recovery.
- Redness and swelling: Beyond the initial post-operative inflammation.
- Warmth to the touch: Indicating increased blood flow to the area.
- Purulent drainage: Pus is a clear sign of infection.
- Fever and chills: Systemic signs of infection.
- Elevated white blood cell count: A laboratory finding indicating infection.
Management: Management involves:
- Wound culture: To identify the causative organism and guide antibiotic selection.
- Antibiotics: Broad-spectrum antibiotics are often initiated empirically, then narrowed once culture results are available.
- Wound debridement: Surgical removal of infected tissue may be necessary in severe cases.
- Wound dressing changes: Frequent dressing changes with appropriate wound care products.
- Pain management: Pain control is crucial for patient comfort and healing.
- Close monitoring: Frequent monitoring for clinical improvement and detection of complications.
For example, if a patient develops localized redness, swelling, and purulent drainage around their incision, we would take a wound culture, start them on broad-spectrum antibiotics, and reassess within 24-48 hours. If there’s no improvement, or if systemic signs of infection appear, surgical debridement might be necessary.
Q 11. Describe your experience with managing a patient with a post-operative ileus.
Post-operative ileus is a temporary paralysis of the bowel that commonly occurs after abdominal surgery. It’s characterized by abdominal distension, nausea, vomiting, and inability to pass gas or stool. Management requires a multi-pronged approach.
In my experience, managing a patient with post-operative ileus starts with conservative measures:
- NPO (nothing by mouth): Resting the bowel is crucial. Intravenous fluids provide hydration and electrolytes.
- Nasogastric suction: To decompress the bowel and remove accumulated gas and fluid.
- Pain management: Pain can exacerbate ileus, so effective analgesia is important.
- Early mobilization: Gentle ambulation can help stimulate bowel motility.
If conservative measures fail, more aggressive interventions might be considered, such as:
- Prokinetic medications: Drugs like metoclopramide stimulate bowel motility.
- Rectal stimulation: A procedure that helps restart bowel movement.
One case I remember involved a patient who developed persistent post-operative ileus after a bowel resection. Conservative measures were initially successful, but when her symptoms persisted, metoclopramide was introduced. Careful monitoring of her fluid balance and electrolyte levels was crucial during this time. Eventually, her bowel function returned, and she was discharged without further complications.
Q 12. Explain the importance of early mobilization in post-operative care.
Early mobilization, meaning getting the patient out of bed and moving around as soon as it’s safe to do so, is a cornerstone of post-operative care. It’s not just about getting patients up and walking; it’s about preventing a cascade of negative consequences.
The benefits are numerous:
- Reduced risk of DVT and PE: Movement improves circulation, preventing blood stasis that leads to clot formation.
- Improved respiratory function: Ambulation helps clear secretions, reducing the risk of pneumonia and atelectasis.
- Faster bowel function recovery: Activity stimulates gut motility, reducing post-operative ileus.
- Reduced risk of urinary tract infections (UTIs): Movement improves bladder emptying.
- Improved overall strength and functional recovery: Early mobilization helps prevent muscle atrophy and promotes faster return to normal activities.
- Reduced hospital length of stay: Patients who mobilize early often have shorter hospital stays.
Of course, early mobilization must be tailored to the patient’s condition and surgical procedure. Patients with certain surgeries or underlying conditions might require a more gradual approach. For example, a patient recovering from a major abdominal surgery would have a different mobilization protocol than a patient after a minor outpatient procedure. Close collaboration with physical therapy is essential.
Q 13. How do you communicate effectively with surgical teams and other healthcare professionals?
Effective communication is essential in the perioperative setting. I utilize a multi-faceted approach to ensure clear and timely communication with surgical teams and other healthcare professionals.
This includes:
- SBAR (Situation-Background-Assessment-Recommendation): This structured communication framework helps convey critical information concisely and efficiently during handoffs or urgent situations. For example, if a patient experiences a sudden drop in blood pressure, the SBAR format helps me convey the necessary information to the surgical team quickly and effectively.
- Regular rounds and team meetings: Participating in regular rounds allows for shared decision-making and collaborative problem-solving. Team meetings facilitate efficient communication regarding patient progress and potential complications.
- Clear and concise documentation: Detailed documentation in the electronic health record (EHR) is crucial for transparency and continuity of care. I ensure that all assessments, interventions, and responses are carefully documented, using standardized terminology and avoiding ambiguity.
- Active listening and respectful dialogue: I actively listen to concerns raised by colleagues and seek to address them appropriately. I also foster an environment of mutual respect and collaboration.
- Escalation of concerns: When necessary, I promptly escalate any urgent issues or concerns to the appropriate healthcare professional or team, ensuring timely intervention.
Q 14. Describe your experience with electronic health records (EHRs) in the perioperative setting.
Electronic health records (EHRs) are integral to efficient and safe perioperative care. My experience with EHRs in this setting is extensive. I’m proficient in using various EHR systems for:
- Pre-operative assessment and planning: EHRs allow for efficient access to patient medical history, including allergies, medications, and past surgical procedures. This information is essential for preoperative planning and risk stratification.
- Intra-operative documentation: EHRs facilitate real-time documentation of the surgical procedure, including fluid balance, blood loss, and medication administration. This ensures accurate and complete documentation of the surgical event.
- Post-operative monitoring and charting: EHRs allow for ongoing monitoring of vital signs, pain scores, and laboratory results. This facilitates timely detection of any complications and enables informed decision-making regarding post-operative management.
- Communication and collaboration: EHRs serve as a central repository for communication between different healthcare providers involved in the patient’s care, improving coordination and reducing the potential for errors.
- Medication management: EHRs provide alerts for potential drug interactions, improving medication safety and minimizing adverse drug events.
While EHRs offer significant benefits, challenges include managing data entry time, ensuring data accuracy, and navigating system complexities. Despite these challenges, proficient use of EHRs is crucial for effective and safe perioperative care.
Q 15. What is your approach to managing a patient’s anxiety before surgery?
Managing pre-operative anxiety is crucial for a successful surgical experience. My approach is multi-faceted and personalized to each patient’s needs. It begins with a thorough assessment of their anxiety levels through conversation and standardized anxiety scales. I then tailor my approach, which may involve:
- Education: Providing clear, concise information about the procedure, what to expect before, during, and after surgery, and answering all their questions honestly and patiently. This reduces uncertainty, a major anxiety trigger.
- Relaxation Techniques: Teaching deep breathing exercises, guided imagery, or progressive muscle relaxation. I might even recommend pre-operative yoga or meditation resources.
- Pharmacological Interventions: In cases of severe anxiety, I would consult with an anesthesiologist to prescribe anxiolytic medications like benzodiazepines, carefully considering potential drug interactions and side effects. This is always a last resort after exploring non-pharmacological options.
- Psychological Support: If anxiety is persistent or significantly impacting the patient’s well-being, I refer them to a psychologist or psychiatrist for further assessment and therapy.
For example, I once had a patient terrified of needles. By carefully explaining the intravenous process, allowing her to control the pace of the insertion, and employing distraction techniques, I was able to alleviate her fear and ensure a smooth pre-operative experience.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you ensure patient safety in the pre-operative and post-operative periods?
Patient safety is paramount in both pre-operative and post-operative care. My approach is built around a system of checks and balances, encompassing:
- Pre-operative Checklist: Thorough review of the patient’s medical history, current medications, allergies, and potential risks. This includes verifying consent forms, completing pre-operative assessments (e.g., ECG, blood work), and ensuring appropriate fasting guidelines are followed.
- Surgical Site Marking: Confirming the correct surgical site with the surgical team and the patient to prevent wrong-site surgery—a critical safety measure. We use indelible markers and involve the patient in the verification process.
- Post-operative Monitoring: Close monitoring of vital signs (heart rate, blood pressure, respiratory rate, temperature, oxygen saturation), pain levels, and potential complications like bleeding, infection, or thromboembolism. This involves frequent assessments, reviewing laboratory results, and close collaboration with the surgical team.
- Medication Reconciliation: Carefully reviewing all medications the patient is taking, including over-the-counter drugs and herbal supplements, to identify potential drug interactions and prevent adverse effects. This is especially important when initiating new post-operative medications.
- Fall Prevention: Assessing fall risk factors and implementing strategies to prevent falls, such as bedside rails, call bells, and appropriate assistance with ambulation, especially in the immediate post-operative period when patients might be drowsy or weak.
For instance, in a recent case, we identified a potential drug interaction during the pre-operative review, preventing a potentially dangerous situation.
Q 17. Describe your experience with different types of surgical drains.
I have extensive experience with various surgical drains, each designed for specific purposes. Some common types include:
- Jackson-Pratt (JP) Drains: These are closed-suction drains often used for collecting fluid from surgical sites. They’re easy to manage and effective in preventing fluid accumulation.
- Hemovac Drains: Similar to JP drains, these also utilize a closed suction system. They are often larger capacity than JP drains.
- Penrose Drains: These are open drains, typically used for passive drainage of fluid. They’re simpler but require more frequent dressing changes and are associated with a higher risk of infection compared to closed-suction systems.
My experience includes managing drains post-operatively, monitoring drainage output, and assessing for signs of infection or complications. For example, I once managed a patient with a significant amount of serosanguineous drainage from a JP drain post-abdominal surgery. Through careful monitoring and prompt attention, we were able to prevent complications. The choice of drain depends heavily on the type of surgery and anticipated drainage volume.
Q 18. How do you recognize and respond to malignant hyperthermia?
Malignant hyperthermia (MH) is a rare but life-threatening genetic disorder triggered by certain anesthetic agents. Recognizing and responding quickly is critical. Symptoms typically present during or shortly after the induction of anesthesia and include:
- Rapid rise in body temperature: This is a late sign and a dangerous indicator; earlier signs are crucial to identify.
- Muscle rigidity: Initially, it might manifest as masseter muscle rigidity (jaw stiffness).
- Tachycardia and arrhythmias: A rapid heart rate and irregular heartbeat.
- Acidosis: An increase in the acidity of the blood.
- Hyperkalemia: Elevated levels of potassium in the blood.
My response protocol involves immediately:
- Stopping the triggering agent: Discontinuing any suspect anesthetic or muscle relaxant immediately.
- Administering dantrolene: This is the specific antidote for MH. Rapid administration is crucial.
- Cooling the patient: Using methods like ice packs, cooling blankets, and possibly even administering iced intravenous fluids to reduce body temperature.
- Supportive care: Managing acidosis, hyperkalemia, and other complications as needed with appropriate medications and respiratory support.
Effective management requires a multidisciplinary team approach, including anesthesiologists, surgeons, and critical care specialists. Early recognition is vital for improved patient outcomes. I have participated in the management of MH cases, emphasizing the importance of rapid and coordinated action. A strong understanding of the pathophysiology and treatment is essential.
Q 19. Explain your understanding of different types of surgical incisions and their implications.
Surgical incisions vary widely depending on the surgical procedure and the surgeon’s preference. Understanding the types and implications is crucial for assessing post-operative risks and planning care. Some common incision types include:
- Midline Incision: A vertical incision along the midline of the abdomen. It provides excellent access to many abdominal organs but can result in significant scar tissue and higher risk of incisional hernias.
- Paramedian Incision: A vertical incision parallel to the midline. Similar access to midline incision but can be associated with less scar tissue.
- Transverse Incision (Pfannenstiel): A horizontal incision across the lower abdomen, often used in gynecological surgery. It tends to have better cosmetic results but may limit access.
- Kocher Incision: A curved incision along the right upper quadrant, typically used for gallbladder surgery. It’s less visible than a midline incision.
The implications of the incision type extend beyond the cosmetic outcome. For instance, midline incisions have a higher risk of infection compared to transverse incisions, and the location of the incision can affect the potential for complications like nerve damage or organ injury. Understanding these implications helps in the development of a tailored post-operative care plan to minimize risks and optimize patient recovery.
Q 20. Describe your experience with administering medications in the pre-operative and post-operative settings.
Administering medications in pre-operative and post-operative settings requires meticulous attention to detail and safety. In the pre-operative phase, medications are often administered to alleviate anxiety, reduce secretions, or provide prophylactic antibiotics. Post-operatively, medications address pain, nausea, prevent complications, and promote healing.
My experience includes administering a wide range of medications, including:
- Analgesics: Opioids (e.g., morphine, fentanyl), non-steroidal anti-inflammatory drugs (NSAIDs), and other pain-relieving medications, always considering the patient’s pain level and risk factors.
- Antiemetics: Medications to prevent or treat nausea and vomiting, crucial for post-operative comfort.
- Anticoagulants: To prevent blood clots, particularly important in post-operative patients at high risk of thromboembolism.
- Antibiotics: Prophylactic antibiotics are given pre-operatively in certain surgical procedures to reduce the risk of infection, while post-operative antibiotics are used to treat infections if they develop.
I strictly adhere to the five rights of medication administration (right patient, right drug, right dose, right route, right time) and document every medication administered meticulously. I always check for allergies and monitor for any adverse reactions, promptly reporting and managing any complications. For instance, I once identified a potential allergy to an antibiotic during the pre-operative assessment, preventing a serious allergic reaction during the surgery. My focus is always on safe and effective medication administration.
Q 21. How do you monitor fluid balance in post-operative patients?
Monitoring fluid balance in post-operative patients is crucial for preventing complications like dehydration, fluid overload, and electrolyte imbalances. My approach involves:
- Accurate Intake and Output (I&O) Measurement: Carefully recording all fluid intake (IV fluids, oral fluids) and output (urine, drainage from drains, vomitus). This provides a clear picture of the patient’s fluid balance.
- Daily Weight Monitoring: Significant weight changes can indicate fluid retention or dehydration. I check daily weights to detect subtle changes.
- Laboratory Assessments: Regularly monitoring serum electrolytes (sodium, potassium, chloride), blood urea nitrogen (BUN), and creatinine levels to assess kidney function and electrolyte balance.
- Clinical Assessment: Assessing for signs of dehydration (e.g., dry mucous membranes, decreased urine output, hypotension) or fluid overload (e.g., edema, shortness of breath, increased blood pressure).
- Adjusting Fluid Therapy: Based on the above assessments, I collaborate with the medical team to adjust intravenous fluid therapy to maintain optimal fluid balance and electrolyte levels.
For example, I recently managed a patient who developed significant fluid loss due to postoperative vomiting. By carefully monitoring I&O and adjusting IV fluids, we were able to prevent dehydration and ensure a smooth recovery. Effective fluid management requires vigilance and a comprehensive approach, involving careful observation and timely interventions.
Q 22. What is your experience with using different monitoring devices in the perioperative setting?
My experience with perioperative monitoring devices is extensive. I’m proficient in using a wide array of equipment, including:
- ECG monitors: Essential for detecting arrhythmias and other cardiac issues, especially crucial during anesthesia and in post-operative recovery. I regularly assess the rhythm strips for abnormalities and adjust treatment accordingly.
- Pulse oximeters: These continuously monitor blood oxygen saturation (SpO2) and pulse rate. A critical tool in identifying hypoxia, a potentially life-threatening condition. I’ve used them extensively to titrate oxygen therapy and address desaturation events.
- Blood pressure monitors (invasive and non-invasive): Essential for assessing hemodynamic stability. Invasive monitoring provides continuous, highly accurate readings, particularly useful in critical cases. Non-invasive methods are used routinely, but I understand their limitations, such as potential for inaccurate readings due to movement or vasoconstriction.
- Capnography: This measures end-tidal carbon dioxide (EtCO2), providing real-time information about ventilation and perfusion. It’s invaluable during anesthesia and in detecting potential airway complications. I rely heavily on capnography to confirm proper endotracheal tube placement and monitor the adequacy of ventilation.
- Temperature monitoring: Continuous temperature monitoring helps detect hypothermia or hyperthermia, both serious post-operative risks. I understand the importance of maintaining normothermia for optimal patient outcomes.
I’m also familiar with advanced monitoring techniques like arterial line insertion and central venous pressure monitoring, employing these when clinically indicated. My experience includes troubleshooting equipment malfunctions and interpreting data to make informed clinical decisions. For example, I recently identified a developing cardiac arrhythmia in a post-operative patient through careful ECG monitoring, leading to prompt intervention and preventing a potentially serious event.
Q 23. How do you assess a patient’s level of consciousness post-operatively?
Assessing a patient’s level of consciousness post-operatively is crucial for safe recovery. I use the Glasgow Coma Scale (GCS) – a standardized neurological assessment tool. The GCS evaluates eye opening, verbal response, and motor response, assigning a score from 3 (deep coma) to 15 (fully alert). A decreasing GCS score indicates neurological deterioration.
Beyond the GCS, I assess the patient’s responsiveness to verbal and tactile stimuli. I observe their orientation to person, place, and time. I also look for signs of agitation, confusion, or lethargy. For example, a patient who is drowsy and difficult to arouse, with a GCS score below 15, requires immediate attention and further investigation.
Furthermore, I consider the patient’s pre-operative neurological status. A baseline assessment helps determine the significance of any post-operative changes. Regular neurological assessments, coupled with continuous monitoring of vital signs, are crucial for early detection and management of post-operative complications.
Q 24. What are the signs and symptoms of post-operative pneumonia?
Post-operative pneumonia is a serious complication characterized by infection of the lungs. Signs and symptoms can range from subtle to life-threatening and include:
- Cough: Often productive, with purulent (pus-containing) sputum.
- Fever: A common indication of infection.
- Shortness of breath (dyspnea): Due to reduced lung capacity.
- Tachypnea (rapid breathing): The body’s attempt to compensate for reduced oxygen levels.
- Increased heart rate (tachycardia): A response to hypoxia and infection.
- Chest pain: Often pleuritic (worsened by deep breaths).
- Lethargy and confusion: Due to reduced oxygenation affecting brain function.
- Auscultatory findings (on lung examination): Crackles, wheezes, or diminished breath sounds.
- Changes in oxygen saturation (SpO2): A low SpO2 reading signals hypoxemia.
Early recognition is vital. Patients with risk factors such as pre-existing lung disease, prolonged surgery, or immunocompromise require close monitoring. Chest X-ray and blood cultures help confirm the diagnosis, guiding appropriate antibiotic therapy and supportive measures like oxygen therapy and respiratory support.
Q 25. Describe your experience with managing a patient experiencing post-operative urinary retention.
Post-operative urinary retention (POUR) is the inability to urinate despite a full bladder. I’ve managed numerous cases, employing a systematic approach:
- Assessment: First, I assess the patient’s bladder distention by palpation and inquire about their last void. I check for any signs of lower urinary tract infection (UTI).
- Bladder scan: A non-invasive ultrasound technique to measure the volume of urine in the bladder. This helps determine the severity of retention.
- Catheterization: If bladder scan shows significant retention and the patient is unable to void, I typically perform intermittent catheterization, a sterile procedure to drain the urine. I document the volume and characteristics of the urine. If intermittent catheterization is unsuccessful or not appropriate, I may consider an indwelling catheter.
- Medication: In some cases, medications like alpha-blockers (to relax the bladder neck) or cholinergic agents (to stimulate bladder contraction) may be used to facilitate voiding, especially if the retention is due to bladder sphincter dysfunction. However, these are typically used after unsuccessful catheterization or as an ongoing treatment plan to prevent recurrent episodes.
- Fluid balance monitoring: Careful monitoring of fluid intake and output is essential to assess hydration and ensure adequate urine production.
For example, I recently managed a patient post-abdominal surgery who developed POUR. After confirming retention with a bladder scan, I performed intermittent catheterization, relieving significant discomfort and preventing potential complications such as bladder rupture or UTI. Post-catheterization, we explored potential underlying causes, ultimately identifying and managing a contributing factor related to opioid-induced constipation which was resolving the issue.
Q 26. Explain your understanding of the different phases of wound healing.
Wound healing is a complex process, typically described in three overlapping phases:
- Inflammatory phase: This initial phase, lasting 3-5 days, involves hemostasis (blood clot formation), vasodilation, and infiltration of inflammatory cells (e.g., neutrophils and macrophages) to clean the wound and begin tissue repair. This phase is characterized by pain, swelling, redness, and warmth around the incision.
- Proliferative phase: This phase, lasting from day 3-21, focuses on tissue formation. Fibroblasts synthesize collagen, creating new tissue called granulation tissue. Epithelial cells migrate across the wound bed, closing the surface. This phase shows evidence of granulation, contraction of the wound edges, and re-epithelialization.
- Maturation phase: This final phase can last for months or even years. The wound continues to gain strength as collagen is remodeled and cross-linking increases. Scar tissue forms, although it’s never as strong as the original tissue. This phase is characterized by progressive reduction of scar size and increased tensile strength.
Understanding these phases helps assess wound healing and identify potential problems. For example, delayed healing in the inflammatory phase could indicate infection, while impaired granulation in the proliferative phase might suggest poor nutrition or ischemia (reduced blood supply). Regular wound assessment, including monitoring for signs of infection, is crucial throughout the healing process.
Q 27. How do you handle a situation where a patient experiences unexpected post-operative bleeding?
Unexpected post-operative bleeding is a serious emergency. My response is immediate and systematic:
- Assessment: First, I assess the patient’s hemodynamic stability – blood pressure, heart rate, respiratory rate, and oxygen saturation. I look for signs of hypovolemic shock (e.g., pallor, cool clammy skin, hypotension). I would also assess the location and amount of bleeding.
- Control the bleeding: This is the immediate priority. Depending on the site of bleeding, this may involve direct pressure, elevation of the affected limb, or packing the wound. I would also ensure IV access is established for fluid resuscitation.
- Fluid resuscitation: To counteract blood loss, I would administer intravenous fluids (crystalloids or colloids), guided by the patient’s hemodynamic parameters. Blood transfusion may be needed if blood loss is significant.
- Notification of the surgical team: The surgeon needs to be notified immediately. They may need to return to the operating room to control the bleeding surgically.
- Monitoring: Continuous monitoring of vital signs, urine output, and hemoglobin/hematocrit levels is essential to assess the effectiveness of interventions and to detect any further deterioration.
For instance, I once encountered a patient who experienced significant bleeding from a surgical incision following abdominal surgery. I immediately applied direct pressure, initiated intravenous fluid resuscitation, and simultaneously contacted the surgical team. The surgeon returned and successfully controlled the bleeding surgically, preventing a potentially life-threatening situation.
Q 28. Describe your approach to documenting pre-operative and post-operative care.
Documentation of pre-operative and post-operative care is meticulous and thorough, adhering to the highest standards. My approach involves:
- Pre-operative documentation: This includes a complete patient history, physical examination findings, relevant laboratory results, imaging studies, informed consent documentation, and pre-operative medication reconciliation. I detail the patient’s baseline condition and any relevant risk factors.
- Intraoperative documentation: This is done by the surgical team, but I ensure accurate recording of the surgery specifics such as duration, complications, anesthesia used, blood loss, and any drains placed.
- Post-operative documentation: This is a comprehensive record covering the patient’s vital signs, pain assessment, fluid balance, medication administration, wound assessment, and any complications encountered. I also note the patient’s neurological assessment, bowel sounds, and urine output. Regular entries are made to document the progress or any changes in the patient’s condition.
- Use of standardized formats: I utilize standardized forms and electronic health records (EHRs) to ensure consistency and completeness of documentation. This ensures clear and concise communication with the medical team.
- Clarity and accuracy: I prioritize accuracy and clarity in my documentation, employing precise medical terminology and avoiding ambiguities. Any significant changes in the patient’s condition are promptly documented with a clear description of interventions taken.
Thorough and accurate documentation is essential for continuity of care, facilitates effective communication among healthcare providers, and protects both the patient and the healthcare team from legal issues. It allows future healthcare providers to understand the patient’s history and condition, and it supports the delivery of optimal care.
Key Topics to Learn for Pre-Operative and Post-Operative Care Interview
- Patient Assessment and Preparation: Understanding pre-operative patient history, physical assessment, and identifying potential risks. Practical application: Developing a comprehensive pre-operative checklist and risk mitigation plan.
- Surgical Site Preparation: Mastering sterile techniques, skin preparation protocols, and the importance of infection control. Practical application: Describing your experience with surgical site preparation and managing potential complications.
- Intraoperative Monitoring and Support: Understanding vital sign monitoring, assisting with anesthesia, and providing patient support during the procedure. Practical application: Explain your role in a specific surgical scenario, highlighting your problem-solving skills.
- Post-Operative Monitoring and Recovery: Recognizing post-operative complications (e.g., hemorrhage, infection, pain management), managing pain effectively, and ensuring patient comfort and safety. Practical application: Detail your experience with post-operative patient care, including pain management strategies and complication prevention.
- Medication Administration and Documentation: Safe and accurate administration of pre- and post-operative medications, alongside precise and thorough documentation. Practical application: Demonstrate your knowledge of common pre- and post-operative medications and their potential side effects.
- Wound Care and Dressing Changes: Proper techniques for wound assessment, cleaning, and dressing changes; recognizing signs of infection. Practical application: Describe your approach to wound care and managing different types of wounds.
- Discharge Planning and Patient Education: Preparing patients for discharge, providing clear and concise instructions, and ensuring patient understanding. Practical application: Outline a discharge plan for a specific post-operative patient, including home care instructions and follow-up appointments.
- Ethical and Legal Considerations: Understanding patient confidentiality, informed consent, and legal implications of medical decisions. Practical application: Discuss a scenario highlighting ethical decision-making in a pre- or post-operative setting.
Next Steps
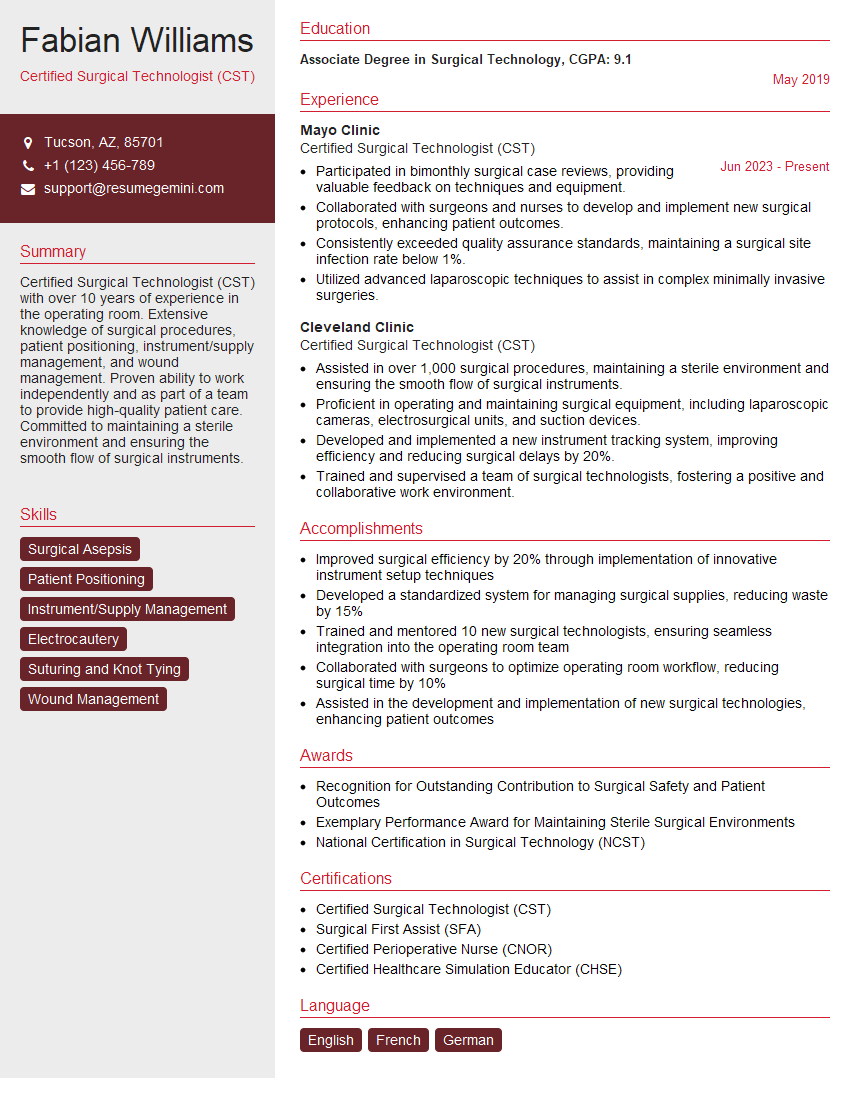
Mastering Pre-Operative and Post-Operative Care is crucial for career advancement in the healthcare field, opening doors to specialized roles and increased responsibility. To significantly boost your job prospects, crafting a strong, ATS-friendly resume is essential. ResumeGemini is a trusted resource to help you build a professional and impactful resume that showcases your skills and experience effectively. Examples of resumes tailored to Pre-Operative and Post-Operative Care are available to help guide you.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
hello,
Our consultant firm based in the USA and our client are interested in your products.
Could you provide your company brochure and respond from your official email id (if different from the current in use), so i can send you the client’s requirement.
Payment before production.
I await your answer.
Regards,
MrSmith
hello,
Our consultant firm based in the USA and our client are interested in your products.
Could you provide your company brochure and respond from your official email id (if different from the current in use), so i can send you the client’s requirement.
Payment before production.
I await your answer.
Regards,
MrSmith
These apartments are so amazing, posting them online would break the algorithm.
https://bit.ly/Lovely2BedsApartmentHudsonYards
Reach out at [email protected] and let’s get started!
Take a look at this stunning 2-bedroom apartment perfectly situated NYC’s coveted Hudson Yards!
https://bit.ly/Lovely2BedsApartmentHudsonYards
Live Rent Free!
https://bit.ly/LiveRentFREE
Interesting Article, I liked the depth of knowledge you’ve shared.
Helpful, thanks for sharing.
Hi, I represent a social media marketing agency and liked your blog
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?