Every successful interview starts with knowing what to expect. In this blog, we’ll take you through the top Substance Abuse Assessment interview questions, breaking them down with expert tips to help you deliver impactful answers. Step into your next interview fully prepared and ready to succeed.
Questions Asked in Substance Abuse Assessment Interview
Q 1. Describe the different stages of substance use disorder.
Substance Use Disorder (SUD), as defined by the DSM-5, doesn’t have explicitly defined stages in the same way some other conditions do. Instead, it’s categorized by severity (mild, moderate, severe) based on the number of criteria met. However, we can conceptually understand a progression in substance use, often reflecting increasing dependence and severity. This progression isn’t linear and individuals may experience setbacks or periods of remission.
Experimentation/Initial Use: This involves initial exposure and infrequent use, often driven by curiosity or social pressure. There’s minimal impact on daily life.
Regular Use/Tolerance: Use becomes more frequent, potentially developing a pattern of regular use. The body starts to adapt, requiring increasing amounts of the substance to achieve the same effect (tolerance).
Dependence/Addiction: This stage is characterized by compulsive drug-seeking behavior, loss of control, continued use despite negative consequences (e.g., job loss, relationship problems), and withdrawal symptoms upon cessation. This is where the criteria for SUD are fully met.
Severe Addiction/Chronic Use: This represents the most severe form, with pervasive and debilitating effects on physical and mental health, relationships, and overall functioning. Life revolves around the substance use.
It’s crucial to remember that not everyone who experiments with substances will progress to severe addiction. Many factors influence the trajectory of substance use, including genetics, environment, social support, and individual coping mechanisms.
Q 2. Explain the assessment process for alcohol dependence.
Assessing for alcohol dependence involves a multi-faceted approach, combining several methods to gather a comprehensive picture of the individual’s situation. It’s not just about the quantity of alcohol consumed but also the impact on their life.
Screening Tools: The process usually begins with standardized screening tools like the AUDIT (Alcohol Use Disorders Identification Test) or CAGE questionnaire (Cut down, Annoyed, Guilty, Eye-opener). These provide a quick assessment of potential problems.
Clinical Interview: A detailed clinical interview is vital. This explores the individual’s drinking history, patterns of use (frequency, quantity, type of alcohol), consequences of drinking (physical, social, legal, occupational), coping mechanisms, and attempts at reducing or stopping drinking. It also explores family history of alcohol problems.
Collateral Information: If possible, gathering information from family members or significant others provides valuable context and can help corroborate or challenge the client’s self-report. This can be particularly helpful if the individual is minimizing their alcohol use.
Physical Examination: A physical exam can reveal signs of alcohol-related organ damage (liver, pancreas, etc.) and assess for any physical withdrawal symptoms.
Laboratory Tests: Blood or urine tests can measure blood alcohol levels (BAL) and detect biomarkers indicative of alcohol abuse. These can objectively support the assessment.
The information gathered from these sources is then used to determine the severity of alcohol dependence based on DSM-5 criteria. For example, someone consistently exceeding drinking guidelines, experiencing withdrawal symptoms, and having significant relationship problems would likely meet criteria for a severe alcohol use disorder.
Q 3. What are the key components of a comprehensive substance abuse assessment?
A comprehensive substance abuse assessment is more than just identifying the substance(s) used; it’s about understanding the individual’s entire context. Key components include:
Substance Use History: Detailed information on types of substances used, frequency, quantity, method of administration, age of onset, patterns of use, and history of detoxification or treatment attempts.
Medical History: Including any physical health conditions, past injuries or surgeries, medications taken (prescription and over-the-counter), and any history of medical or psychiatric hospitalizations. This is crucial to identify potential interactions and co-occurring conditions.
Psychiatric History: Thorough assessment for co-occurring mental health disorders (anxiety, depression, PTSD, bipolar disorder, schizophrenia, etc.) using validated screening tools and clinical interview techniques. This is critical because mental illness and substance use often coexist.
Social History: Information on family history, relationships, employment status, social support systems, education level, legal history, and significant life events. A strong support system significantly impacts recovery.
Legal History: Any arrests, convictions, or involvement with the legal system related to substance use. This helps understand the consequences of the individual’s actions and inform treatment planning.
Risk Assessment: Evaluating the risk of relapse, suicide, violence, and harm to self or others. This is a critical safety step and informs the development of safety plans.
Treatment Planning: Based on the overall assessment, a personalized treatment plan should be developed outlining specific goals, interventions, and referral recommendations tailored to individual needs and strengths.
Think of it like a puzzle – each piece (substance use history, medical history, etc.) contributes to the bigger picture of understanding the client and developing effective treatment.
Q 4. How do you assess for co-occurring disorders?
Co-occurring disorders (CODs), also known as dual diagnoses, refer to the presence of both a substance use disorder and a mental health disorder. Assessing for CODs requires a careful and thorough evaluation of both conditions. It’s often not a simple ‘either/or’ situation, as they frequently influence each other.
Structured Clinical Interviews: Validated clinical interviews, such as the SCID (Structured Clinical Interview for DSM Disorders), can help reliably assess both substance use and mental health disorders. These interviews follow a standardized format, reducing bias and increasing the accuracy of diagnosis.
Symptom Inventories and Rating Scales: Tools like the Beck Depression Inventory (BDI) for depression, the Generalized Anxiety Disorder 7-item scale (GAD-7) for anxiety, and the PTSD Checklist for PTSD help quantify symptom severity. This allows for a more objective measure of mental health symptoms.
Collateral Information: Information from family members, friends, or previous treatment providers can offer valuable insight into the individual’s history of mental health symptoms and their relationship to substance use. It can help verify or clarify information obtained directly from the individual.
Medical Records Review: A review of past medical records can identify previous diagnoses, treatment experiences, and hospitalizations, offering a complete timeline of both substance use and mental health issues.
It’s crucial to remember that the symptoms of a mental health disorder can be masked by or exacerbated by substance use. Therefore, careful assessment is needed to disentangle the effects of each and arrive at accurate diagnoses.
Example: An individual presenting with significant anxiety might be using alcohol to self-medicate. Without addressing both the anxiety disorder and the alcohol use, treatment is unlikely to be successful.
Q 5. What screening tools are commonly used in substance abuse assessment?
Many screening tools are available to assist in the initial assessment of substance use. The choice of tool depends on the specific substance(s) of concern, the client’s demographics, and the setting (e.g., primary care, emergency room, specialized treatment center).
Alcohol: AUDIT (Alcohol Use Disorders Identification Test), CAGE questionnaire, TWEAK (Tolerance, Worry, Eye-opener, Amnesia, K/Cut down).
Drugs: DAST (Drug Abuse Screening Test), SASSI (Substance Abuse Subtle Screening Inventory), CRAFFT (Car, Relax, Alone, Forget, Family, Trouble) – often used with adolescents.
Opioids: Specific screening tools are available for opioid use, assessing both misuse and potential for overdose risk. These often address pain medication use and prescription opioid diversion.
These screening tools are not diagnostic in themselves. A positive screening result indicates the need for a more thorough assessment, while a negative result doesn’t definitively rule out substance use. They serve as an efficient first step in identifying individuals who may benefit from further evaluation.
Q 6. Explain the difference between substance abuse and substance dependence.
The terms “substance abuse” and “substance dependence” are not used consistently across all diagnostic systems. The DSM-5, which is widely used in the US, uses the single term “Substance Use Disorder” (SUD) to encompass both previous concepts of abuse and dependence.
Historically, ‘substance abuse’ referred to a pattern of substance use leading to negative consequences in various life areas, while ‘substance dependence’ implied more severe problems including tolerance, withdrawal, and compulsive drug-seeking behavior. The DSM-5 integrated these into a single disorder classified by severity (mild, moderate, severe) based on the number of criteria met.
To illustrate, someone might have previously been diagnosed with ‘substance abuse’ if they frequently drank to excess and experienced occasional problems at work. With the DSM-5, they might now receive a diagnosis of mild or moderate SUD based on the specific criteria they meet.
Q 7. How do you determine the severity of a substance use disorder?
The severity of a SUD is determined by the number of DSM-5 criteria met. The more criteria met, the more severe the disorder. The criteria cover various aspects of substance use including:
Impaired control: Larger amounts or longer periods than intended, unsuccessful attempts to cut down, craving.
Social impairment: Failure to fulfill major obligations, continued use despite relationship problems, social activities given up.
Risky use: Use in physically hazardous situations, continued use despite physical or psychological problems exacerbated by use.
Pharmacological criteria: Tolerance, withdrawal.
A mild SUD involves meeting 2-3 criteria, moderate 4-5 criteria, and severe 6 or more criteria. This approach considers the totality of the individual’s experience with the substance, reflecting the impact on their life rather than solely relying on the amount or frequency of use.
For example, someone meeting six criteria might receive a diagnosis of severe SUD. This highlights the significant impact of the substance use on various facets of their life and reinforces the need for intensive treatment.
Q 8. Describe your experience with motivational interviewing.
Motivational Interviewing (MI) is a collaborative, person-centered counseling approach that aims to elicit and strengthen motivation for change. It’s not about directly persuading a client, but rather guiding them to explore their own ambivalence and resolve any discrepancies between their values and their current behavior. My experience with MI spans several years, working with diverse populations struggling with substance use disorders. I’ve used it extensively in individual and group settings.
For example, I recently worked with a client struggling with alcohol dependence. Instead of lecturing them about the dangers of alcohol, I used open-ended questions like, “Tell me about your thoughts and feelings regarding your drinking.” and “How important is it to you to make a change?” This allowed them to verbalize their concerns and identify their own reasons for wanting – or not wanting – to change. We then collaboratively explored the pros and cons of continuing to drink versus reducing or abstaining. This process, guided by MI principles, empowered them to make their own decision, rather than feeling pressured into change.
I’ve found that MI is particularly effective in engaging clients who are ambivalent about treatment, as it respects their autonomy and fosters a sense of partnership. I utilize the four core MI principles: expressing empathy, developing discrepancy, rolling with resistance, and supporting self-efficacy.
Q 9. How do you handle client resistance during an assessment?
Handling client resistance is a crucial aspect of substance abuse assessment. Resistance often manifests as defensiveness, denial, or avoidance. Instead of confronting resistance directly, which can be counterproductive, I utilize strategies rooted in motivational interviewing. This involves acknowledging and validating their feelings, reflecting their concerns, and reframing resistance as a normal part of the change process.
Imagine a client who minimizes their substance use. Instead of arguing, I might say, “I hear you saying that your use isn’t a big problem, but I also understand you’re here seeking help. Can you tell me more about what’s led you to seek help today?” This acknowledges their perspective while gently guiding them towards a more honest self-assessment. It’s about understanding the underlying reasons for their resistance, which often stem from fear, shame, or a lack of perceived self-efficacy.
If resistance persists despite these efforts, I may adjust my approach, perhaps exploring alternative assessment methods or collaborating with the client to determine what feels most comfortable and conducive to open communication. Ultimately, building rapport and trust is key to overcoming resistance and achieving a thorough and accurate assessment.
Q 10. What ethical considerations are involved in substance abuse assessment?
Ethical considerations in substance abuse assessment are paramount. These considerations revolve around maintaining client confidentiality, ensuring informed consent, avoiding bias, and safeguarding client well-being.
- Confidentiality: Client information must be protected, adhering to HIPAA regulations and professional ethical guidelines. I carefully explain confidentiality limits at the outset, such as mandated reporting of child abuse or threats of harm to self or others.
- Informed Consent: Clients must fully understand the purpose, procedures, and potential risks and benefits of the assessment before agreeing to participate. This includes explaining how the information will be used and who will have access to it.
- Cultural Sensitivity: Assessments should be culturally appropriate and account for individual differences in beliefs, values, and experiences. Biased assessments can lead to inaccurate diagnoses and inappropriate treatment plans.
- Dual Relationships: Avoiding dual relationships (e.g., therapist-client and social relationships) is crucial to maintain objectivity and ethical boundaries.
- Competence: I only conduct assessments within my scope of practice. If a client’s needs extend beyond my expertise, I refer them to a more appropriate professional.
Ethical dilemmas may arise, requiring careful consideration and consultation with supervisors or ethics committees. For instance, balancing client confidentiality with the need to protect others from harm necessitates thoughtful decision-making guided by ethical guidelines.
Q 11. How do you maintain client confidentiality during the assessment process?
Maintaining client confidentiality is crucial. I strictly adhere to HIPAA regulations and all relevant professional ethical guidelines. This includes securing client records, using encrypted electronic systems, and limiting access to client information to only those individuals with a legitimate need to know.
During assessments, I explain confidentiality limits upfront. For instance, I clearly state that while most information shared will remain confidential, there are exceptions, such as mandated reporting of child abuse or situations where there’s an imminent threat to self or others. I use anonymized data when presenting case studies or discussing client information with colleagues. Physical records are stored securely, and electronic records are password-protected and encrypted. My commitment to confidentiality builds trust and encourages clients to openly share crucial information for a comprehensive assessment.
Q 12. What are the limitations of standardized assessments?
Standardized assessments offer valuable data, but they have limitations. One major limitation is that they may not fully capture the complexity of individual experiences. These instruments often rely on self-report, which can be influenced by factors like denial, social desirability bias, and memory limitations.
For instance, a standardized test might categorize a client as having a certain level of alcohol dependence based on a structured questionnaire, but it might not accurately reflect the nuances of their lived experience or the impact of their substance use on their relationships and overall functioning. Additionally, standardized assessments may not be culturally sensitive or appropriate for all populations. It’s crucial to interpret standardized test results cautiously, considering these limitations and integrating them with clinical judgment and other assessment data (e.g., collateral information, clinical interviews). A comprehensive assessment requires more than just a standardized test score; it’s about building a holistic picture of the individual.
Q 13. Describe your approach to assessing for relapse risk.
Assessing relapse risk is crucial in substance abuse treatment. My approach is multifaceted and involves several key steps. First, I conduct a thorough history taking, including details about past substance use patterns, triggers, coping mechanisms, and previous treatment experiences. This helps to identify individual risk factors.
I also assess current psychosocial functioning, including their social support network, housing stability, employment status, and mental health. These factors significantly impact relapse risk. I utilize validated screening tools that assess for relapse risk, but this information is then integrated into a broader clinical picture. For example, I might use the Drug Abuse Screening Test (DAST) or similar tools but focus as much on the client’s narrative and personal insights during the assessment.
Finally, I collaborate with the client to develop a personalized relapse prevention plan. This involves identifying potential high-risk situations, developing coping strategies, and establishing support systems. The plan is a collaborative effort, empowering the client to take an active role in their recovery.
Q 14. How do you develop a treatment plan based on the assessment findings?
Developing a treatment plan based on assessment findings is a collaborative process. I begin by summarizing the key findings from the assessment, including the client’s substance use history, current level of functioning, identified strengths, weaknesses, and specific relapse risk factors. Then, I engage the client in a discussion about their treatment goals, preferences, and resources available to them.
Based on this, I collaboratively develop a treatment plan that addresses the client’s unique needs. This plan typically outlines specific treatment goals, interventions, and timelines. Interventions might include individual therapy, group therapy, medication management, 12-step participation, or other evidence-based approaches. The treatment plan is a dynamic document—it can be adjusted as the client’s needs evolve and their progress is monitored throughout treatment. Regular review sessions are essential to ensuring its ongoing relevance and effectiveness.
For example, if a client shows significant anxiety alongside their substance abuse, the treatment plan would incorporate anxiety management techniques, potentially including medication or specialized therapy, alongside the substance abuse treatment.
Q 15. What are some common barriers to treatment that you have encountered?
Barriers to substance abuse treatment are multifaceted and often intertwined. They can be broadly categorized into individual, social, and systemic factors.
- Individual Barriers: These include denial of the problem, lack of motivation, mental health comorbidities (like depression or anxiety which often co-occur with substance use disorders), and the presence of trauma which can significantly impact engagement in treatment. For example, a client might minimize their substance use, believing it doesn’t impact their life significantly, creating a roadblock to seeking help.
- Social Barriers: These involve lacking a supportive social network, financial constraints which can prevent access to treatment, stigma associated with addiction preventing people from seeking help, and family dynamics that inadvertently reinforce substance use. Imagine a scenario where a client’s family members are also struggling with addiction, providing an unstable and potentially triggering home environment.
- Systemic Barriers: This encompasses limitations within the healthcare system, such as lack of access to affordable or appropriate treatment programs, long waiting lists for services, and insufficient insurance coverage. For instance, a rural individual might lack proximity to specialized substance abuse programs, leading to increased difficulties.
Addressing these barriers requires a holistic approach, involving not just the individual but also their support systems and the systems that affect access to care. This may include providing financial assistance, connecting clients with social support, and addressing the co-occurring mental health issues.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you tailor your assessment approach to different client populations (e.g., adolescents, adults, older adults)?
Tailoring my assessment approach is crucial for effective intervention. Each age group presents unique challenges and considerations.
- Adolescents: Assessments with adolescents necessitate a developmentally appropriate approach. The language used needs to be clear and accessible, and the setting should be comfortable and non-judgmental. Parental involvement (with the adolescent’s consent) is often essential, as it can provide valuable context and support. We need to be sensitive to developmental issues like peer pressure and family conflict.
- Adults: Assessments with adults may be more straightforward, but must still be tailored to their individual circumstances. It’s important to explore their personal history with substance use, their current coping mechanisms, and their goals for treatment. Identifying their strengths and resources is key to a successful treatment plan. This is the group where the use of standardized instruments like the AUDIT or CAGE is frequently used.
- Older Adults: Older adults may present with unique challenges, including multiple medical conditions that interact with substance use, changes in physical functioning, and social isolation. Assessing for medication interactions and other health issues is critical. The assessment process might need to be adjusted to their physical or cognitive limitations, involving family members more frequently for clarity and contextual information. For example, considering hearing or vision impairment in the assessment process.
In all cases, a collaborative and empathetic approach is key. It’s vital to build rapport with the client to foster trust and ensure a reliable assessment.
Q 17. Explain your experience with using different assessment instruments (e.g., AUDIT, CAGE, DAST).
I have extensive experience using various assessment instruments to screen for and evaluate the severity of substance use disorders. Each tool serves a specific purpose.
- AUDIT (Alcohol Use Disorders Identification Test): This is a widely used, 10-item questionnaire that screens for alcohol problems. It covers frequency, quantity, and consequences of alcohol use. Its strength lies in its brevity and ease of administration. However, it might not capture the nuances of all types of problematic drinking.
- CAGE Questionnaire: A short, four-item screening tool focusing on cutting down, annoyance at criticism, guilt, and eye-openers. It’s effective at quickly identifying individuals who may require further assessment. However, it misses individuals who may have problems that don’t fit neatly into the questions.
- DAST (Drug Abuse Screening Test): This is a 20-item instrument that screens for drug use problems across various substance categories. It covers frequency, quantity, and consequences of drug use. It provides a broader assessment of substance use patterns beyond alcohol.
It’s important to note that these are screening tools, not diagnostic tests. Positive results warrant a more comprehensive clinical interview to fully understand the nature and severity of the substance use disorder. The interpretation of these tools also needs to take into account cultural context and any potential biases.
Q 18. How do you document your assessment findings?
Accurate and comprehensive documentation is crucial for legal, ethical, and clinical reasons. My documentation follows a standardized format, typically including:
- Identifying information: Client’s name, date of birth, etc. (protected using appropriate methods).
- Reason for referral: Why the client is seeking assessment.
- History of substance use: Detailed information about the types of substances used, frequency, quantity, duration, and patterns of use (including past and present usage).
- Assessment findings: Results from standardized screening tools (AUDIT, CAGE, DAST etc.), clinical observations, and the client’s self-reported information.
- Mental health history and status: Presence of co-occurring mental health disorders.
- Medical history: Relevant medical conditions and medications that could interact with substances.
- Social history: Family history of substance use, social support network, housing, employment.
- Diagnosis: Based on DSM-5 criteria for substance use disorders.
- Treatment recommendations: Specific recommendations for treatment modality, level of care, and referral sources.
Documentation is always maintained in accordance with HIPAA guidelines to maintain client confidentiality and privacy. The goal is to create a clear, concise, and accurate record that can be easily understood by other healthcare professionals involved in the client’s care.
Q 19. How do you ensure the cultural competency of your assessment practices?
Cultural competency is paramount in substance abuse assessment. It acknowledges that cultural factors significantly impact substance use patterns, help-seeking behavior, and responses to treatment.
- Awareness of cultural differences: I actively strive to understand the cultural backgrounds of my clients and the ways their culture might influence their experiences with substance use. This includes being mindful of potential language barriers and employing interpreters when necessary.
- Use of culturally sensitive assessment tools: Some standardized instruments may not be equally valid across all cultural groups. I carefully select instruments that have demonstrated cultural appropriateness or use culturally modified versions.
- Collaboration with community resources: I maintain relationships with community organizations that serve diverse cultural groups to ensure culturally tailored support services.
- Self-reflection and ongoing learning: I regularly engage in continuing education to improve my understanding of different cultural perspectives on substance use and mental health.
For example, understanding how cultural norms regarding alcohol consumption can influence a client’s self-perception of their drinking habits or the stigma associated with mental health conditions within certain communities is vital for conducting a fair and valid assessment. It’s about building trust and ensuring the client feels understood and respected.
Q 20. Describe your experience with the DSM-5 criteria for substance use disorders.
The DSM-5 criteria for substance use disorders provide a standardized framework for diagnosing these conditions. The criteria are based on a dimensional approach, meaning the severity of the disorder is rated along a continuum from mild to severe, based on the number of criteria met.
The criteria encompass various aspects of problematic substance use, including:
- Impaired control: Difficulty controlling substance use, craving, using more than intended.
- Social impairment: Relationship problems, failure to fulfill obligations.
- Risky use: Continued use despite physical or psychological harm.
- Pharmacological criteria: Tolerance and withdrawal.
Understanding these criteria is crucial for making accurate diagnoses and developing effective treatment plans. It allows for a consistent and objective assessment of the client’s substance use patterns and their impact on their lives. The DSM-5 allows for a nuanced understanding of the disorder, recognizing the spectrum of severity and allowing for more precise treatment recommendations.
Q 21. How do you assess for withdrawal symptoms?
Assessing for withdrawal symptoms involves a combination of methods, including clinical interviews, physical examinations, and the use of standardized scales.
- Clinical Interview: A detailed interview focusing on the client’s recent substance use patterns, any changes in their physical or mental state, and symptoms they have experienced since reducing or stopping their substance use. This is crucial for understanding the temporal relationship between substance cessation and symptom onset.
- Physical Examination: A physical examination helps to identify any physical manifestations of withdrawal, such as elevated heart rate, blood pressure, tremors, or sweating. These physical signs are often substance-specific.
- Standardized Scales: Various scales exist to assess withdrawal severity, such as the Clinical Institute Withdrawal Assessment for Alcohol (CIWA-Ar) for alcohol withdrawal or the COWS (Clinical Opiate Withdrawal Scale) for opioid withdrawal. These scales provide objective measurements of withdrawal symptoms.
The severity of withdrawal can vary greatly depending on the type of substance, the duration and intensity of use, and the individual’s physical and mental health. It’s critical to monitor individuals experiencing withdrawal closely, as severe withdrawal can be life-threatening. Early recognition and intervention are essential in managing withdrawal safely and effectively. Appropriate medical management, including medication, is usually necessary for severe withdrawal.
Q 22. How do you differentiate between substance-induced disorders and primary mental health disorders?
Differentiating between substance-induced disorders and primary mental health disorders can be complex, as they often co-occur. A substance-induced disorder is a mental disorder whose symptoms are directly caused by the physiological effects of a substance (e.g., alcohol, drugs). These symptoms resolve or significantly improve when the substance is discontinued. Think of it like this: the substance is the *cause* of the mental health problem. For instance, someone experiencing severe anxiety and paranoia after a binge of cocaine would be exhibiting a substance-induced anxiety disorder. In contrast, a primary mental health disorder exists independently of substance use. While substance use might exacerbate symptoms, the underlying condition would persist even in the absence of substance use. For example, someone with pre-existing depression might use alcohol to self-medicate, but the depression itself is the primary issue. Accurate diagnosis requires a thorough assessment considering the timing of symptoms relative to substance use, the individual’s history, and a careful examination of symptom clusters.
Clinicians utilize diagnostic tools like the DSM-5 to make this distinction. It’s crucial to rule out a substance-induced disorder before diagnosing a primary mental health condition, as treatment approaches differ significantly. For example, addressing the substance use might alleviate the symptoms of the substance-induced disorder, while a primary depression would require a different treatment plan, perhaps including therapy and medication.
Q 23. What is your understanding of the biopsychosocial model of addiction?
The biopsychosocial model of addiction is a holistic framework that recognizes the interplay of biological, psychological, and social factors in the development and maintenance of addiction. It moves beyond the simplistic ‘moral failing’ or purely biological explanations.
- Biological factors include genetics (family history of addiction), brain chemistry (neurotransmitter imbalances), and physiological responses to substances. For example, a predisposition to dopamine dysregulation might increase vulnerability to substance dependence.
- Psychological factors encompass personality traits (impulsivity, risk-taking), cognitive processes (beliefs about substance use), emotional regulation, and past trauma. Someone with unresolved trauma might use substances to cope with emotional pain.
- Social factors include family dynamics, peer influences, cultural norms, socioeconomic status, and access to resources. A community with easy access to drugs and high rates of substance use would increase an individual’s risk.
The model emphasizes that addiction is not solely a matter of individual willpower, but a complex interaction of these three domains. This understanding is crucial for developing comprehensive and effective treatment plans that address all contributing factors. For example, a treatment program might incorporate medication to address biological imbalances, cognitive-behavioral therapy to change maladaptive thoughts and behaviors, and social support groups to foster healthy relationships and coping mechanisms.
Q 24. How do you work with clients who are mandated to treatment?
Working with mandated clients presents unique challenges and requires a nuanced approach. The key is to build rapport and establish a therapeutic alliance, even though the client’s initial motivation might be low. I prioritize understanding their perspective and validating their feelings about being mandated to treatment. I avoid judgmental language and focus on collaborative goal-setting.
For example, instead of saying, ‘You have to do this,’ I might say, ‘Let’s explore what you hope to achieve through this process.’ We collaboratively create a treatment plan that considers their individual needs and preferences within the parameters of the court order or other mandate. Regular progress reviews and open communication are essential to address any resistance or challenges. It’s important to consistently monitor compliance, document progress, and effectively communicate with relevant stakeholders (e.g., probation officers, courts).
Ultimately, my goal is to help the client engage in treatment and move toward recovery, even if their initial motivation is externally driven. Sometimes, external accountability can become a catalyst for internal change.
Q 25. Describe your experience with crisis intervention in the context of substance abuse.
Crisis intervention in substance abuse often involves managing life-threatening situations like overdoses, acute withdrawal symptoms, or suicidal ideation. My experience includes assessing the immediate risk, providing stabilization, and connecting clients with necessary resources. This often involves a rapid assessment of the client’s current state, including their physical and mental health, recent substance use, and potential for harm to self or others.
For example, if a client presents with an overdose, immediate medical intervention is paramount, including calling emergency services and administering naloxone if appropriate. Following stabilization, I would assess the underlying factors contributing to the crisis, which may include withdrawal, relapse triggers, or unresolved psychological distress. Once the immediate crisis is addressed, I help develop a safety plan to prevent future crises, which might involve connecting them with detox, residential treatment, or intensive outpatient programs.
Crisis intervention is time-sensitive and requires strong clinical judgment, rapid assessment skills, and the ability to work effectively under pressure. Collaboration with other professionals, such as medical personnel and law enforcement, is often essential. Following a crisis, ongoing care and support are crucial to prevent relapse.
Q 26. How do you utilize collateral information in your assessment?
Collateral information plays a vital role in a comprehensive substance abuse assessment. This involves gathering information from sources other than the client, such as family members, friends, employers, medical professionals, or legal representatives. This provides valuable context and corroboration of the client’s self-report.
For instance, a client might downplay their substance use, but a family member might provide information about the frequency and severity of their substance use. Similarly, medical records can reveal the history of substance-related health problems. Obtaining informed consent whenever possible is critical. Ethical considerations always guide this process, balancing the need for information with the client’s right to confidentiality.
I carefully integrate collateral information with the client’s self-report and other clinical data to build a comprehensive picture of their substance use patterns, associated problems, and treatment needs. This ensures a holistic perspective and reduces reliance on potentially biased or inaccurate self-reports.
Q 27. What are your strategies for managing clients with severe mental illness and substance use disorders?
Clients with co-occurring severe mental illness (SMI) and substance use disorders (SUDs) require specialized treatment approaches. The treatment is often referred to as dual diagnosis treatment. A common mistake is to treat one disorder in isolation from the other. It’s crucial to address both simultaneously using an integrated approach.
My strategies involve:
- Integrated assessment: A comprehensive assessment to thoroughly evaluate both the mental health and substance use conditions. This might include psychological testing and psychiatric evaluation.
- Medication management: Working closely with psychiatrists to manage both psychiatric symptoms (e.g., depression, psychosis) and substance withdrawal symptoms.
- Psychotherapy: Using evidence-based therapies such as Cognitive Behavioral Therapy (CBT) or Dialectical Behavior Therapy (DBT) to address underlying psychological issues contributing to both the SMI and SUD.
- Case management: Coordinating care across multiple providers and ensuring access to needed services, such as housing, vocational rehabilitation, and social support.
- Harm reduction strategies: Employing harm reduction strategies to minimize the negative consequences of substance use while working toward abstinence or moderation.
For example, a client with schizophrenia and alcohol dependence might benefit from antipsychotic medication for their schizophrenia, medication for alcohol withdrawal, CBT to manage cravings and relapse prevention, and case management to access housing and social support. Collaboration with a multidisciplinary team of mental health professionals and substance abuse specialists is essential to success.
Q 28. How do you ensure your own self-care and prevent burnout when working with this population?
Self-care is not a luxury; it’s a necessity for professionals working in substance abuse. The emotional toll of this work can be significant, and burnout is a serious risk. My self-care strategies include:
- Maintaining healthy boundaries: Not allowing the work to consume my personal life and setting limits on my emotional investment in client cases.
- Regular supervision: Meeting regularly with a supervisor to process challenging cases and receive support.
- Peer support: Connecting with colleagues to share experiences and discuss strategies for managing challenging situations.
- Stress management techniques: Practicing stress-reducing techniques such as mindfulness, meditation, or exercise.
- Hobbies and interests: Engaging in activities outside of work that promote relaxation and enjoyment.
- Seeking personal therapy: Utilizing personal therapy as a way to address personal challenges and maintain mental wellness.
Burnout is not a sign of weakness, but a consequence of sustained stress. By prioritizing self-care, I can maintain my own well-being and provide the best possible care to my clients. Recognizing the signs of burnout and taking proactive steps to address them is crucial to sustaining a fulfilling and effective career in this field.
Key Topics to Learn for Substance Abuse Assessment Interview
- Assessment Techniques: Understanding various assessment methods, including standardized tests, clinical interviews, and collateral information gathering. Consider the strengths and limitations of each approach.
- Diagnostic Criteria: Deep understanding of DSM-5 and ICD-11 criteria for substance use disorders, including different severity levels and specifiers. Be prepared to discuss how these criteria are applied in practice.
- Ethical Considerations: Familiarity with ethical guidelines and legal implications related to confidentiality, informed consent, and mandated reporting in substance abuse assessment. This includes navigating complex situations and boundaries.
- Cultural Competence: Demonstrating an awareness of how cultural factors influence substance use and assessment practices. Be prepared to discuss culturally sensitive approaches and potential biases.
- Co-occurring Disorders: Understanding the prevalence and treatment implications of co-occurring mental health and substance use disorders. Be able to discuss integrated assessment and treatment strategies.
- Treatment Planning: Knowledge of different treatment modalities and the ability to formulate effective treatment plans based on assessment findings. This includes matching interventions to individual needs and preferences.
- Case Management & Referral: Understanding the process of coordinating care and making appropriate referrals to other services, such as detoxification, medication-assisted treatment, or support groups.
- Documentation & Reporting: The importance of accurate, concise, and thorough documentation of assessment findings and treatment plans, adhering to professional standards and legal requirements.
- Relapse Prevention Strategies: Knowledge of different relapse prevention strategies and the ability to integrate them into treatment planning. This involves understanding individual risk factors and protective factors.
Next Steps
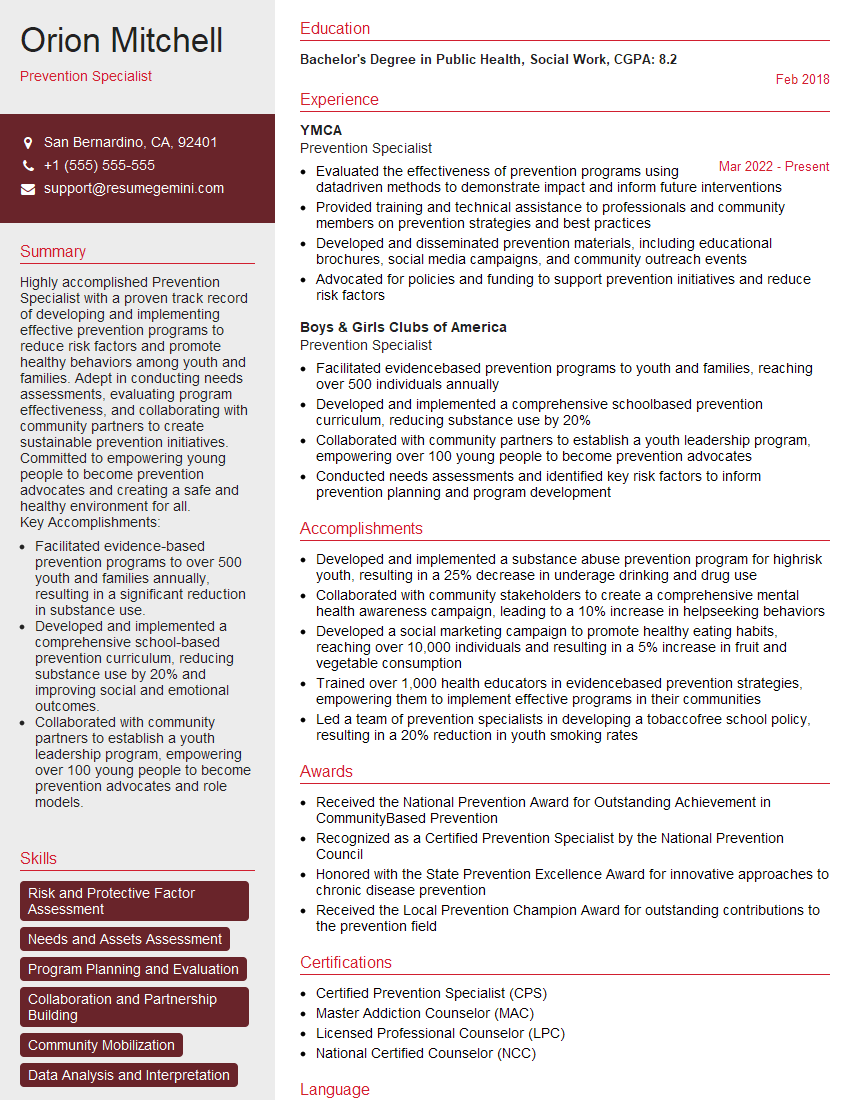
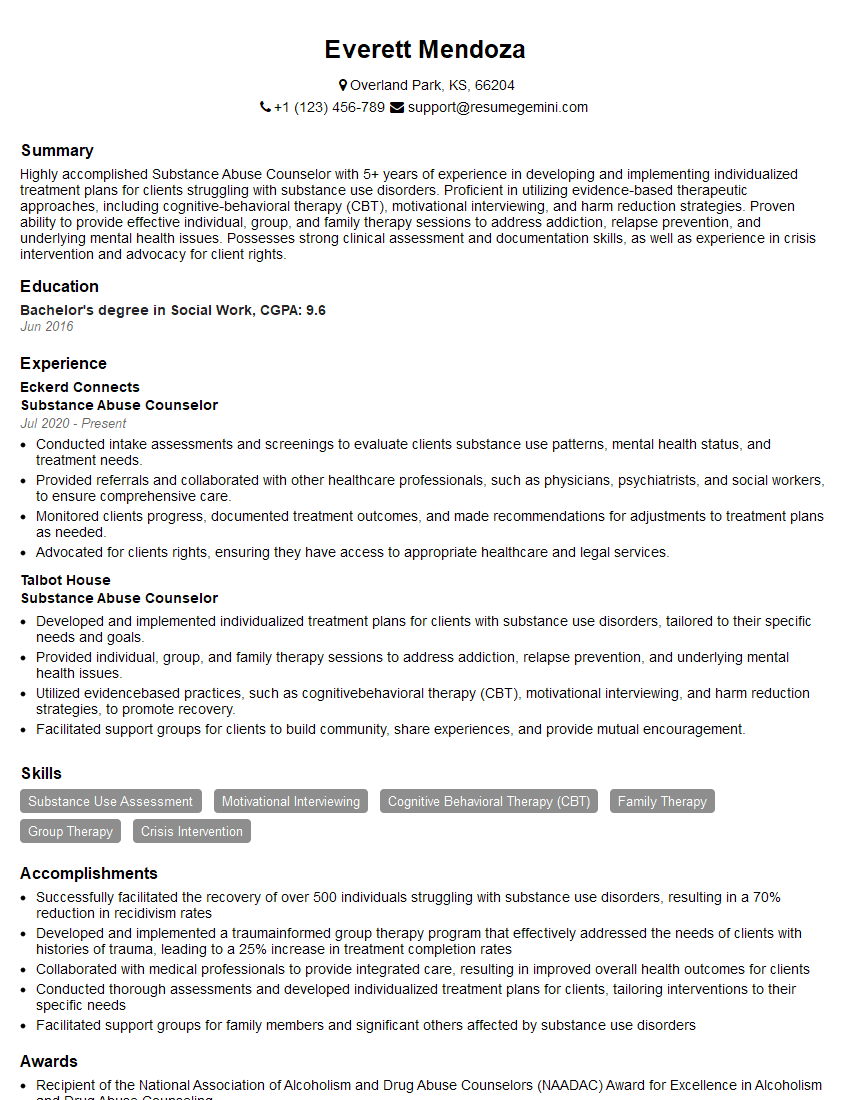
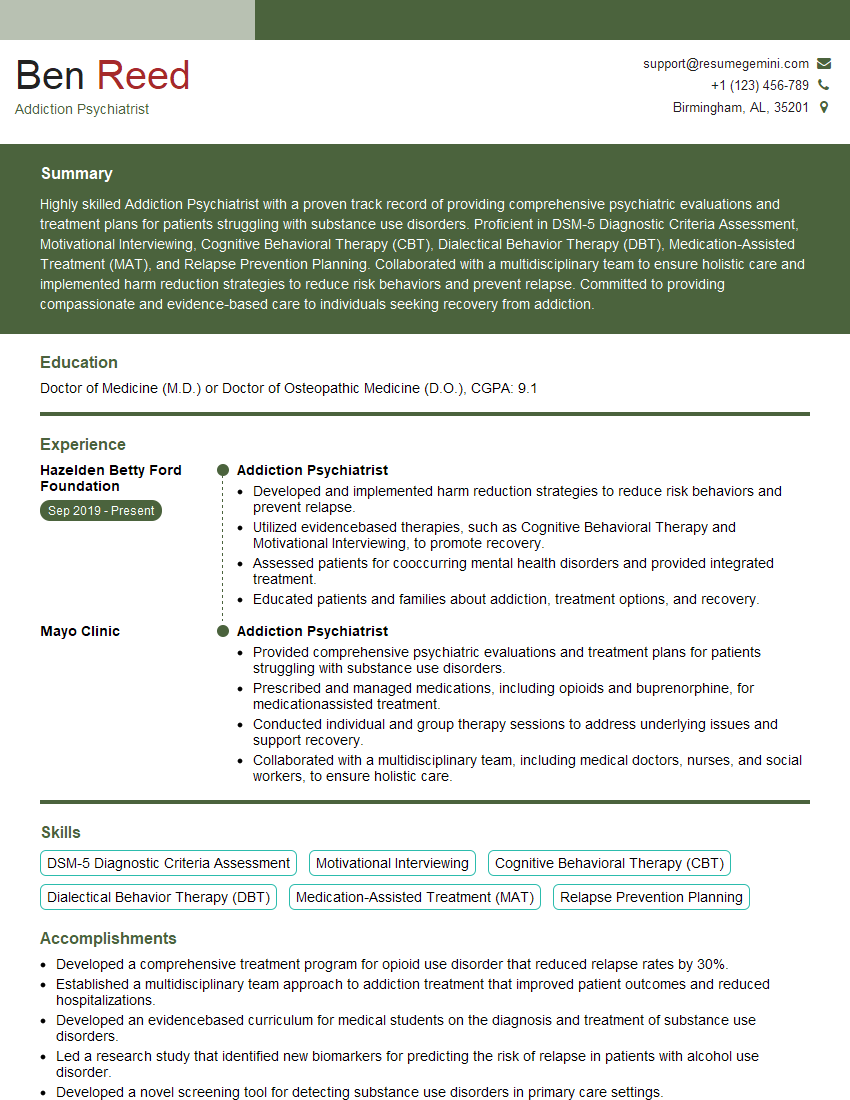
Mastering Substance Abuse Assessment is crucial for a rewarding and impactful career in behavioral health. It opens doors to diverse roles offering significant contributions to individuals and communities grappling with addiction. To maximize your job prospects, focus on creating a strong, ATS-friendly resume that highlights your skills and experience effectively. ResumeGemini is a trusted resource to help you build a professional resume that truly showcases your capabilities. We offer examples of resumes tailored specifically to Substance Abuse Assessment roles to guide you in this process.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Interesting Article, I liked the depth of knowledge you’ve shared.
Helpful, thanks for sharing.
Hi, I represent a social media marketing agency and liked your blog
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?